Abstract
Recent epidemiological studies have suggested a positive association between ultra-processed food consumption and breast cancer risk, although some studies also reported no association. Furthermore, the evidence regarding the associations between intake of food with lower degrees of processing and breast cancer risk is limited.
Thus, we investigated the associations between dietary intake by degree of food processing and breast cancer risk, overall and by breast cancer subtypes in the European Prospective Investigation into Cancer and Nutrition (EPIC) study.
Dietary intake of EPIC participants was assessed via questionnaires at baseline. More than 11,000 food ingredients were classified into four groups of food processing levels using the NOVA classification system: unprocessed/minimally processed (NOVA 1), culinary ingredients (NOVA 2), processed (NOVA 3) and ultra-processed (NOVA 4). Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) of breast cancer per standard deviation increase in daily consumption (grams) of foods from each NOVA group.
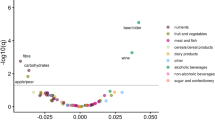
The current analysis included 14,933 breast cancer cases, diagnosed among the 318,686 EPIC female participants, (median follow-up of 14.9 years). No associations were found between breast cancer risk and the level of dietary intake from NOVA 1 [HR per 1 SD=0.99 (95% CI 0.97 – 1.01)], NOVA 2 [HR per 1 SD =1.01 (95% CI 0.98 – 1.03)] and NOVA 4 [HR per 1 SD =1.01 (95% CI 0.99 – 1.03)] foods. However, a positive association was found between NOVA 3 and breast cancer risk [HR per 1 SD =1.05 (95% CI 1.03 – 1.07)] which became non-significant after adjustment for alcohol intake [HR per 1 SD =1.01 (95% CI 0.98 – 1.05)] or when beer and wine were excluded from this group [HR per 1 SD =0.99 (95% CI 0.97 – 1.01)]. The associations did not differ by breast cancer subtype, menopausal status or body mass index. Findings from this large-scale prospective study suggest that the positive association between processed food intake and breast cancer risk was likely driven by alcoholic beverage consumption.
Graphical Abstract

Similar content being viewed by others
Introduction
Diets have transitioned from fresh, unprocessed, and minimally processed foods toward a rise in the consumption of ultra-processed foods. These now contribute roughly 25 to 60% of the total daily energy intake of individuals across countries (Adams & White, 2015; Juul et al., 2022; Latasa et al., 2018; Levy et al., 2022; Madruga et al., 2022; Marrón-Ponce et al., 2019; Moubarac et al., 2014a; Wang et al., 2021). In the past decades, several food processing frameworks have been developed, such as the NOVA classification, the Food Standards Australia New Zealand, the International Food and Information Council, and the International Food Policy and Research Institute (Bleiweiss-Sande et al., 2019; Crino et al., 2017; Moubarac et al., 2014b). Although most of these similarly classify basic foods as processed or unprocessed, the NOVA system is the most widely applied to scientific studies and may be more useful for monitoring changes in the food supply and evaluating associations with health outcomes (Crino et al., 2017; Monteiro et al., 2019). The NOVA classification categorizes foods into four groups based on the extent and purpose of food processing they undergo: unprocessed/minimally processed foods (NOVA 1), processed culinary ingredients (NOVA 2), processed foods (NOVA 3) and ultra-processed foods (NOVA 4) (Monteiro et al., 2019). Foods classified as NOVA 4, which are foods that undergo multiple physical, biological, and/or chemical processes, have been suggested to have detrimental health effects due to their poorer nutritional qualities on average (e.g. they are often energy dense and/or rich in saturated and trans-fatty acids) or the presence of a wide range of additives and contaminants formed during processing (Lane et al., 2021; Pagliai et al., 2021; Srour et al., 2022). Epidemiological studies investigating the association between the consumption of foods classified by the NOVA scale and the risk of breast cancer are sparse. Breast cancer risk was inversely associated with NOVA 1 (Fiolet et al., 2018; Jacobs et al., 2022), positively associated with NOVA 3 (Kliemann et al., 2023), and either not associated (Jacobs et al., 2022; Romaguera et al., 2021) or positively (Chang et al., 2023; Fiolet et al., 2018; Romieu et al., 2022) associated with NOVA 4. A recent analysis in the European Prospective Investigation into Cancer and Nutrition (EPIC), performed by our group, suggested that higher consumption of NOVA 1 was associated with lower breast cancer risk while higher consumption of NOVA 3 was associated with higher breast cancer risk (Kliemann et al., 2023). In that study, we did not stratify our analyses by breast cancer subtype although such analyses could shed light on the potential mechanisms underlying the associations observed between different degrees of food processing and breast cancer, since the etiologies behind breast cancer subtypes are different. Furthermore, few previous studies were able to stratify their analyses by breast cancer subtypes or by alcohol intake and body mass index (BMI). Therefore, the aim of this study was to investigate the associations between diet according to the degree of food processing and breast cancer risk, overall and by breast cancer subtype, menopausal status, alcohol intake and BMI, within the EPIC cohort.
METHODS
EPIC Cohort
Between 1992 and 2000, a total of 521,323 EPIC participants were recruited from 23 centers across 10 European countries (Riboli et al., 2002). At recruitment, socio-demographic, dietary, lifestyle, anthropometric and medical data were collected for all participants by administration of validated country-specific questionnaires. Ethical approval for the study was obtained from the relevant ethical review boards of the participating centers of EPIC as well as from the ethics committee of the International Agency for Research on Cancer (IARC).
Study population and follow-up
The selection of the study population is shown in Supplementary Figure S1. We used data from all participating countries apart from Greece due to a lack of data access. Participants were further excluded if they (i) had any cancer diagnosis before recruitment, (ii) had no follow-up, (iii) had no lifestyle or dietary information, (iv) had an energy intake-to-requirement ratio within the extreme ranking (top and bottom 1%, which are implausible dietary exposure values), or (v) were men. Women were followed from study inclusion until the date of their latest known contact, cancer diagnosis, death, emigration, or the end of the follow-up period (between 2008 and 2014 depending on the center), whichever occurred first. The analytical sample included 318,686 women who were free of cancer at recruitment.
Identification of incident breast cancer cases
In Italy, Spain, the United Kingdom, the Netherlands, Denmark, Norway, and Sweden, population-based cancer registries were used to identify breast cancer cases. In France and Germany, a combination of methods was used, including health insurance records, contacts with cancer and pathology registries, and active follow-up of participants and their next of kin. Almost all centers (except Malmö, Granada, and Murcia) had information on tumor characteristics, including invasiveness status (in situ/invasive/unknown), estrogen receptor (ER) status (ER-positive/ER-negative/unknown), progesterone receptor (PR) status (PR-positive/PR-negative/unknown), and human epidermal growth factor receptor 2 (HER2) status (HER2-positive/HER2-negative/unknown). The diagnosis of breast cancer cases was based on the 2nd or the 3rd revision (depending on the year of diagnosis) of the International Classification of Diseases for Oncology (ICD-O-2 or ICD-O-3) (International Statistical Classification of Diseases and Related Health Problems 10th Revision, n.d.). In the present work, the first diagnosis of breast cancer was identified as primary incident breast tumors. Vital status was collected from regional or national mortality registries.
Dietary data and NOVA classification
Country-specific dietary questionnaires were used in EPIC and validated at the center level (Huybrechts et al., 2022). Semi-quantitative food frequency questionnaires, extensive quantitative dietary questionnaires, and combined methods (i.e. a 7-day record on hot meals was combined with quantitative food-frequency questionnaires in Malmö, Sweden) were used to collect dietary data at baseline. These were center specific to account for local dietary habits and were either self-administered or administered in-person by trained interviewers. These data were then harmonized to obtain a standardized food list with comparable detail across countries. The dietary questionnaires and their mode of administration were described in detail in previous publications (Riboli et al., 2002, Huybrechts I et al., 2022). Then, more than 11,000 foods/ingredients/beverages were categorized into one of the four NOVA groups based on their degrees of food processing. The different NOVA groups are defined in the Additional File (Text S1). The classification of EPIC foods into NOVA groups has been described in depth elsewhere (Huybrechts et al., 2022). To account for potential changes in industrialization over time, lower, middle, and upper bound scenarios were created. The "middle bound" scenario, deemed most likely in the past 25 years, was used for the primary analysis. In the “lower bound” scenario, foods with potential for less processing were assigned to a lower processed NOVA group, while in the “upper bound” scenario, foods with potential for more processing were assigned to a higher processed.
For each study participant, we calculated the dietary intake from each NOVA group as expressed by (1) the total absolute intake in grams/day (g/day) and (2) the total absolute intake in kcal/day (kcal/d). We also calculated the relative contribution of each NOVA food group to the total daily dietary intake in grams (%g/day) and kcal (%kcal/day). The g/d unit was considered the primary exposure because it better captures industrial foods with zero calorie content (e.g., artificially sweetened drinks) and food processing factors (e.g., neoformed contaminants or food additives).
Covariates at recruitment
Information on lifestyle, reproductive/hormonal factors, and medical history was gathered using baseline questionnaires. All EPIC centers collected information on educational level, age at menarche, age at first full term pregnancy and parity, breastfeeding, and use of oral contraceptives and menopausal hormone therapy (MHT). Menopausal status was determined by combining different baseline information. Women who reported to have menstrual cycles, had at least nine menstrual periods over the previous 12 months, or were younger than 42 years were considered as premenopausal women. Women who reported fewer than four menses in the past year, a bilateral ovariectomy, or were older than 55 years were considered as postmenopausal women. Otherwise, women were considered perimenopausal.
Body weight and height were either measured by a health care professional or self-reported in each center. Weight and height were used to calculate BMI defined as weight in kilograms divided by height in meters squared (kg/m2). Physical activity levels were estimated using a questionnaire focused on past-year physical activity in occupational, leisure, and household domains. The Cambridge physical activity index was then created by combining occupational physical activity with time spent in physical exercise (such as cycling, swimming, and jogging) (Wareham et al., 2003). Alcohol intake in grams per day was based on the number of standard glasses of wine, beer, cider, sweet liquor, distilled spirits, or fortified wines consumed daily or weekly during the 12 months before recruitment. The Mediterranean diet score was calculated using a methodology previously described (Couto et al., 2011).
Statistical analysis
In the main analyses, the middle-bound scenario for the NOVA classification and the absolute g/d of the four NOVA food groups were used.
Baseline characteristics were examined by quartiles of each NOVA food group intake. Multivariable Cox proportional hazards regression models were performed to estimate hazard ratios (HRs) and their corresponding 95% confidence intervals (CIs) for the associations between the intake of each NOVA food group [1 standard deviation (SD) increment] and breast cancer incidence, overall and by breast cancer subtypes. Age served as the primary time scale. All four NOVA groups were simultaneously included in the Cox model.
All models were stratified by age at recruitment in 1-year categories and study center and adjusted for potential confounding factors including educational level (none, primary school, technical/professional school, higher education), physical activity (inactive, moderately inactive, moderately active, active), height in cm (continuous), age at menarche in years (≤ 13, > 13), oral contraceptive use (never, ever, unknown), pregnancies (nulliparous,1 or 2 children, >3 children), age at first full-term pregnancies (continuous), breastfeeding (never, ever, unknown), menopausal status (pre, peri, post-menopause), and menopausal hormone therapy (MHT) use (never, ever, unknown). We investigated whether adding different dietary-related factors/components (BMI, total energy intake, total fat, sodium intake, carbohydrate intake, Mediterranean diet, and alcohol intake) to the model changed the HR associated with NOVA groups. Only alcohol consumption modified the HRs and was therefore included in an additional model (Supplementary Table S1). Ever use of oral contraceptives and MHT and breastfeeding had >5% missing values, which were accommodated by using a “missing” category in the models. All other covariates had <5% missing values, which were replaced with the mode for categorical variables, or the median for continuous variable values observed among the subjects with complete data.
Heterogeneities according to the invasiveness status or hormonal receptor status were evaluated with competing risk analyses. In these analyses, cases with missing information on the studied subtype were excluded from the corresponding analysis and those who developed the competing breast cancer subtypes were censored at the time of occurrence (Lunn & McNeil, 1995). Heterogeneities were calculated as the deviations of logistic beta-coefficients observed in each of the subgroup relative to the overall beta-coefficient.
As subgroup and sensitivity analyses, we repeated the analyses (1) by using lower and upper bound scenarios for the NOVA classification, (2) by using consumption of NOVA groups measured as %g/d, kcal/d and %kcal/d instead of g/d, and (3) by removing alcoholic drinks (present in NOVA groups 3 and 4). When we analyzed the intake of NOVA food groups measured as the proportion of overall daily food intake (%g/d) or daily kcal intake (%kcal/d), Cox regression analyses were performed separately for each NOVA group. Finally, we explored whether associations between NOVA groups and breast cancer risk varied by alcohol intake, BMI categories, menopausal status and country. Effect modification was evaluated by using likelihood ratio tests to compare models with and without cross-product interaction terms. Statistical analyses were conducted using SAS software (version 9.4, Copyright © 2017, SAS Institute Inc.).
Results
During a median follow-up time of 14.9 years (13.5-16.4), 14,933 breast cancer cases were diagnosed (1,603 in situ, 13,320 invasive, and 10 of unknown invasiveness status) among the 318,686 participants. Among the invasive breast cancer cases, 9,525 had information on ER status (7,789 ER-positive and 1,736 ER-negative), 7,994 on PR status (5,268 PR-positive and 2,726 PR-negative), and 4,577 on HER2 status (901 HER2-positive and 3,676 HER2-negative). There were 573 ER+PR±HER2+, 3023 ER+PR±HER2-, 264 ER-PR-HER2-, and 419 ER-PR-HER2+ breast cancer cases.
Using the middle-bound scenario expressed as g/d, consumption of food classified as NOVA 1 contributed 74% of the total diet (Table 1). The main foods contributing to this group were coffee/tea (31%), water (19%), fruits (12%) and milk/plain yogurt (12%) (Table 2). The contribution of NOVA 2 to the total diet was 1%, with plant oils being the highest contributor to the group (37%) followed by table sugar (29%), and animal fats (28%). The contribution of processed foods (NOVA 3) to the total diet was 11%, with an important contribution of beer/wine (35%) and processed bread (26%). Overall, ultra-processed foods (NOVA 4) contributed 13% to the total diet with dairy desserts and drinks among the top group contributors (14%), followed by soft drinks (13%), ultra-processed breads (12%) and sweetened beverages (11%). The relative intake of food classified as NOVA 1 was highest in France (80%) and Denmark (79%). The relative intake of food classified as of NOVA 2 was highest in Italy (3%) and Spain (2%). NOVA 3 foods were mostly highly consumed in Italy (23%), Spain (14%) and Germany (14%), while NOVA 4 foods were highly consumed in Norway (23%) and the United Kingdom (19%).
The main baseline characteristics of participants by quartiles of intake of NOVA 1, NOVA 2, NOVA 3, and NOVA 4 are presented in supplementary Tables S2, S3, S4 and S5, respectively.
Table 3 shows the associations between the middle-bound scenario of each NOVA group intake (in g/d) and breast cancer, overall and by breast cancer subtypes. Overall, intake of NOVA 1 [HRper 1 SD=0.99 (95% CI 0.97 – 1.01)], NOVA 2 [HRper 1 SD=1.01 (0.98 – 1.03)], and NOVA 4 [HRper 1 SD=1.01 (0.99 – 1.03)] were not associated with breast cancer risk. However, intake of processed foods (NOVA 3) was associated with a higher risk of breast cancer [HRper 1 SD=1.05 (1.03 – 1.07)]. Estimates did not differ by invasiveness or hormone receptor status (Table 3, Phomogeneity≥ 0.11). When the model was further adjusted for alcohol intake (Table 4), the positive association between NOVA 3 and breast cancer risk was attenuated and no longer statistically significant [HRper 1 SD=1.01 (0.98 – 1.03)]. Furthermore, when alcoholic drinks were excluded from NOVA 3 the association with breast cancer risk was also null [HRper 1 SD=0.99 (0.97 – 1.01), Table 5]. Associations were similar when models were stratified by alcohol intake, BMI at recruitment (Pinteraction ≥ 0.17, Table 6) or menopausal status (Table S6).
In secondary analyses using %g/d, kcal/d or %kcal/d as the exposure, the results were consistent with those obtained in the main analyses (Supplementary Table S7). However, when using %g/d as an exposure variable, a higher intake of NOVA 1 was associated with a slightly lower risk of breast cancer [HRper 1 SD =0.96 (0.94 - 0.98)]. Nevertheless, this association was no longer statistically significant when the model was further adjusted for alcohol intake [HRper 1 SD =0.98 (0.94-1.00), Supplementary Table S7]. In addition, the results were similar when we used lower and upper bound scenarios (data not shown). Finally, no heterogeneity was reported by country (Phomogeneity ≥ 0.09, Supplementary Table S8).
Discussion
In this large-scale prospective analysis, we found a positive association between the consumption of processed foods and breast cancer, which was likely driven by alcohol – an already established risk factor for breast cancer. The association between the degree of food processing and breast cancer risk did not differ by breast cancer subtype, menopausal status, alcohol intake or BMI.
In this study, no associations were found between the consumption of food included in the NOVA 1 group and breast cancer risk, overall or by breast cancer subtypes when the absolute values of intake were evaluated (g/day or kcal/day). Although a slight inverse association was reported when the %g/day values were used, this association disappeared when models were further adjusted for alcohol intake. Furthermore, because we only observed an inverse association when the variable was expressed as %g/d, these results might be because individuals who consumed more food from NOVA group 1 also consumed less food from NOVA group 3. Only one cohort study (Fiolet et al., 2018) and one case-control study (Jacobs et al., 2022) investigated associations between NOVA 1 and breast cancer risk and reported an inverse association (using %g/d and %kcal/d, respectively). Although NOVA 1 foods have low energy density and are rich in phytochemicals (carotenoids, flavonoids, dietary fiber), vitamins and minerals, known to be anticancerogenic (Bakker et al., 2016), our study does not support the hypothesis of a lower breast cancer risk with higher intake of NOVA 1 foods. In addition, we found no evidence of an association between NOVA 2 and breast cancer risk, as also reported in a South African case-control study (Jacobs et al., 2022).
We observed a positive association between NOVA 3 intake and breast cancer risk. To our knowledge, no previous population study has reported a positive association between NOVA 3 and breast cancer risk (Fiolet et al., 2018; Jacobs et al., 2022). Interestingly, in our study population, the positive association disappeared when models were adjusted for alcohol consumption or when alcoholic drinks were excluded from the NOVA groups. Indeed, alcohol is an established risk factor for breast cancer and, as such, could drive the positive association between processed foods and breast cancer risk. Of note, in this study we observed that, on average, beer and wine made up 35% of NOVA 3 g/day intake.
Furthermore, we found no evidence of an association between the consumption of NOVA 4 and breast cancer risk. Other studies have also reported no association between NOVA 4 intake and breast cancer risk (Jacobs et al., 2022; Romaguera et al., 2021). However, our results differ from those from the NutriNet-Santé French cohort and two case-control studies, which reported a positive association between the consumption of NOVA 4 and breast cancer risk (Fiolet et al., 2018; Queiroz et al., 2018; Romieu et al., 2022). It has been suggested that NOVA 4 foods may increase breast cancer risk through several factors such as their high energy density due to added sugars and fats, the presence of a variety of additives, preservatives and processing contaminants (e.g. acrylamide, trans-fatty acids, endocrine disrupters, etc.) or lack of fiber, proteins, and other components that are associated with fullness and satisfaction, leading individuals to eat more in an attempt to feel satisfied/saturated (Friedman, 2015; Luiten et al., 2016; Moubarac et al., 2013; Pouzou et al., 2018). In addition, we might have expected to observe a positive association between NOVA 4 and breast cancer risk due to alcoholic distilled drinks, however, in this study population alcoholic distilled drinks made up 2.2% of NOVA 4 g/day intake. The lack of association between NOVA 4 and breast cancer risk in the current study might be explained by the fact that the consumption of NOVA 4 in EPIC was quite low as this was based on dietary intakes at recruitment (during the nineties); since then, the consumption of NOVA 4 has replaced the consumption of other NOVA groups (e.g. recipes that were made at home in the 1990s may currently be industrially processed), which may bias the associations with breast cancer risk. Indeed, NOVA 4 has been recently suggested to represent up to 60% of total daily energy intake in some countries of the European area such as the UK (Rauber et al., 2018) while in the current EPIC study population, NOVA 4 contributed to 31% of total energy intake (data not shown). However, when we classified food products based on the modern/current food environment (upper bound scenario), the association between NOVA 4 and breast cancer risk was still null.
Finally, in our study, the associations between the degree of food processing and breast cancer risk did not differ by invasiveness and hormone receptor status. Our results are consistent with a previous study that investigated the association between NOVA 4 and breast cancer risk by molecular status suggesting no differences in risk estimates [ER+ or PR+: OR10% increase=1.04 (0.96 – 1.13); HER2+: OR10% increase=0.96 (0.84 – 1.10); ER-PR-HER2-: OR10% increase=0.93 (0.75 – 1.15)] (Romaguera et al., 2021). However, another study reported a positive association between NOVA 4 and ER+ breast cancer [ORT3vsT1=2.44 (1.01 - 5.90)] and no clear association with ER- breast cancer [ORT3vsT1=1.87 (0.43 - 8.13)] (Romieu et al., 2022). No other studies reported results for other NOVA groups by invasiveness and molecular status of breast cancer, which makes any comparison with our results challenging.
Our study has several strengths including the prospective design, the multicenter aspect, the long-term follow-up, and the availability of a comprehensive assessment of participant characteristics, as well as the large number of incident breast cancer cases. We had self-reported data on lifestyle, reproductive, and medical factors and were therefore able to consider a wide range of potential confounders. We also stratified the analyses according to menopausal status, alcohol intake, obesity breast cancer subtype. However, it should be noted that the statistical power for some of these stratified analyses was rather low (e.g. for some of the breast cancer subtypes), therefore, these results should be interpreted with caution. The major limitation of the study is that dietary data were only collected at baseline (in the 1990s) while the food environment changed in the intervening years, exposing the EPIC participants to potentially different degrees of food processing over the course of their follow-up. However, three different scenarios were created considering that the food environment may have changed over time compared to the baseline. The lower and upper bound scenarios were used in sensitivity analyses to explore the potential impact of further industrialization of food products and of changes in consumer habits to convenience foods over time, and results were virtually unchanged. The fact that dietary data were collected only once may cause random measurement error and may fail to reflect long-term habits; any such bias would likely lead to an underestimation of true associations (i.e. regression dilution bias) (Clarke et al., 1999; Hutcheon et al., 2010). However, it is noteworthy that recent analyses comparing dietary follow-up data in some of the EPIC countries demonstrate only minor changes in dietary intakes among the EPIC participants, potentially due to the relatively older age of the participants included in the cohort (unpublished data). Finally, the dietary questionnaires used in EPIC were not designed to identify different food processing categories. Therefore, several assumptions had to be made when insufficient information about the processing of the food item was available, potentially contributing to measurement error. However, byproducts of processing (e.g. trans fatty acids or syringol metabolites) have been positively associated with NOVA group 4 in EPIC which is a sign of a good measurement of ultra-processed foods in EPIC (Huybrechts et al., 2022).
Conclusion
This large-scale prospective analysis among European women suggests that the positive association between processed food intake and breast cancer risk was likely driven by alcoholic beverage consumption. Other degrees of food processing were not associated with breast cancer risk.
Availability of data and materials
For information on how to apply for gaining access to EPIC data and/or biospecimens, please follow the instructions at https://epic.iarc.fr/access/submit_appl_access.php.
Abbreviations
- BMI:
-
Body Mass Index
- CIs:
-
Confidence Intervals
- EPIC:
-
European Prospective Investigation into Cancer and Nutrition
- ER:
-
Estrogen Receptor
- HER2:
-
Human Epidermal Growth Factor Receptor 2
- HRs:
-
Hazard Ratios
- IARC:
-
International Agency for Research on Cancer
- ICD-O:
-
International Classification of Diseases for Oncology
- MHT:
-
Menopausal Hormone Therapy
- OR:
-
Odd Ratio
- PR:
-
Progesterone Receptor
- SD:
-
Standard Deviation
References
Adams, J., & White, M. (2015). Characterisation of UK diets according to degree of food processing and associations with socio-demographics and obesity: cross-sectional analysis of UK National Diet and Nutrition Survey (2008–12). International Journal of Behavioral Nutrition and Physical Activity., 12(1), 160.
Bakker, M. F., Peeters, P. H., Klaasen, V. M., Bueno-de-Mesquita, H. B., Jansen, E. H., Ros, M. M., et al. (2016). Plasma carotenoids, vitamin C, tocopherols, and retinol and the risk of breast cancer in the European Prospective Investigation into Cancer and Nutrition cohort. The American Journal of Clinical Nutrition, 103(2), 454–64.
Bleiweiss-Sande, R., Chui, K., Evans, E. W., Goldberg, J., Amin, S., & Sacheck, J. (2019). Robustness of Food Processing Classification Systems. Nutrients, 11(6), 1344.
Chang, K., Gunter, M. J., Rauber, F., Levy, R. B., Huybrechts, I., Kliemann, N., et al. (2023). Ultra-processed food consumption, cancer risk and cancer mortality: a large-scale prospective analysis within the UK Biobank. EClinicalMedicine, 56, 101840.
Clarke R, Shipley M, Lewington S, Youngman L, Collins R, Marmot M, et al. (1999) Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. American Journal Of Epidemiology;150(4):341‑53.
Couto, E., Boffetta, P., Lagiou, P., Ferrari, P., Buckland, G., Overvad, K., et al. (2011). Mediterranean dietary pattern and cancer risk in the EPIC cohort. British Journal of Cancer, 104(9), 1493–9.
Crino M, Barakat T, Trevena H, Neal B (2017) Systematic Review and Comparison of Classification Frameworks Describing the Degree of Food Processing. Nutrition Food Technology;3(1).
Fiolet, T., Srour, B., Sellem, L., Kesse-Guyot, E., Allès, B., Méjean, C., et al. (2018). Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ: British medical journal / British Medical Association, 360, k322.
Friedman, M. (2015). Acrylamide: inhibition of formation in processed food and mitigation of toxicity in cells, animals, and humans. Food & Function, 6(6), 1752–72.
Hutcheon, J. A., Chiolero, A., & Hanley, J. A. (2010). Random measurement error and regression dilution bias. BMJ, 340, c2289. British Medical Journal Publishing Group.
Huybrechts I, Rauber F, Nicolas G, Casagrande C, Kliemann N, Wedekind R, et al (2022) Characterization of the degree of food processing in the European Prospective Investigation into Cancer and Nutrition: Application of the Nova classification and validation using selected biomarkers of food processing. Frontiers in Nutrition.
International Statistical Classification of Diseases and Related Health Problems 10th Revision. https://icd.who.int/browse10/2010/en. Accessed 11 Nov 2023.
Jacobs I, Taljaard-Krugell C, Wicks M, Cubasch H, Joffe M, Laubscher R, et al (2022) Degree of food processing and breast cancer risk in black urban women from Soweto, South African: the South African Breast Cancer study. British Journal of Nutrition: 1‑12.
Juul, F., Parekh, N., Martinez-Steele, E., Monteiro, C. A., & Chang, V. W. (2022). Ultra-processed food consumption among US adults from 2001 to 2018. The American Journal of Clinical Nutrition, 115(1), 211–21.
Kliemann, N., Rauber, F., Bertazzi Levy, R., Viallon, V., Vamos, E. P., Cordova, R., et al. (2023). Food processing and cancer risk in Europe: results from the prospective EPIC cohort study. Lancet Planet Health, 7(3), e219-32.
Lane, M. M., Davis, J. A., Beattie, S., Gómez-Donoso, C., Loughman, A., O’Neil, A., et al. (2021). Ultraprocessed food and chronic noncommunicable diseases: a systematic review and meta-analysis of 43 observational studies. Obesity Reviews, 22(3), e13146.
Latasa, P., Louzada, M. L. D. C., Martinez Steele, E., & Monteiro, C. A. (2018). Added sugars and ultra-processed foods in Spanish households (1990–2010). European Journal of Clinical Nutrition, 72(10), 1404–12. Nature Publishing Group.
Levy RB, Andrade GC, Cruz GL da, Rauber F, Louzada ML da C, Claro RM, et al. (2022) Três décadas da disponibilidade domiciliar de alimentos segundo a NOVA – Brasil, 1987–2018. 56:75.
Luiten, C. M., Steenhuis, I. H., Eyles, H., Ni Mhurchu, C., & Waterlander, W. E. (2016). Ultra-processed foods have the worst nutrient profile, yet they are the most available packaged products in a sample of New Zealand supermarkets. Public Health Nutrition, 19(3), 530–8.
Lunn, M., & McNeil, D. (1995). Applying Cox regression to competing risks. Biometrics, 51(2), 524–32.
Madruga M, Martínez Steele E, Reynolds C, Levy RB, Rauber F (2022) Trends in food consumption according to the degree of food processing among the UK population over 11 years. British Journal of Nutrition: 1‑24.
Marrón-Ponce, J. A., Flores, M., Cediel, G., Monteiro, C. A., & Batis, C. (2019). Associations between Consumption of Ultra-Processed Foods and Intake of Nutrients Related to Chronic Non-Communicable Diseases in Mexico. Journal of the Academy of Nutrition and Dietetics, 119(11), 1852–65.
Monteiro, C. A., Cannon, G., Levy, R. B., Moubarac, J.-C., Louzada, M. L., Rauber, F., et al. (2019). Ultra-processed foods: what they are and how to identify them. Public Health Nutrition, 22(5), 936–41.
Moubarac, J.-C., Martins, A. P. B., Claro, R. M., Levy, R. B., Cannon, G., & Monteiro, C. A. (2013). Consumption of ultra-processed foods and likely impact on human health. Evidence from Canada. Public Health Nutrition, 16(12), 2240–8.
Moubarac, J.-C., Batal, M., Martins, A. P. B., Claro, R., Levy, R. B., Cannon, G., et al. (2014). Processed and ultra-processed food products: consumption trends in Canada from 1938 to 2011. Canadian Journal of Dietetic Practice and Research, 75(1), 15–21.
Moubarac, J.-C., Parra, D. C., Cannon, G., & Monteiro, C. A. (2014). Food classification systems based on food processing: significance and implications for policies and actions: a systematic literature review and assessment. Current Obesity Reports, 3(2), 256–72.
Pagliai, G., Dinu, M., Madarena, M. P., Bonaccio, M., Iacoviello, L., & Sofi, F. (2021). Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. British Journal of Nutrition, 125(3), 308–18.
Pouzou, J. G., Costard, S., & Zagmutt, F. J. (2018). Probabilistic assessment of dietary exposure to heterocyclic amines and polycyclic aromatic hydrocarbons from consumption of meats and breads in the United States. Food and Chemical Toxicology, 114, 361–74.
Queiroz SA, Sousa IM de, Silva FR de M, Lyra C de O, Fayh APT (2018) Nutritional and environmental risk factors for breast cancer: a case-control study. Scientia Medica. 28(2):ID28723‑ID28723.
Rauber F, da Costa Louzada ML, Steele EM, Millett C, Monteiro CA, Levy RB. (2018). Ultra-Processed Food Consumption and Chronic Non-Communicable Diseases-Related Dietary Nutrient Profile in the UK (2008-2014). Nutrients, 10(5), 587
Riboli, E., Hunt, K. J., Slimani, N., Ferrari, P., Norat, T., Fahey, M., et al. (2002). European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutrition, 5(6B), 1113–24.
Romaguera, D., Fernández-Barrés, S., Gracia-Lavedán, E., Vendrell, E., Azpiri, M., Ruiz-Moreno, E., et al. (2021). Consumption of ultra-processed foods and drinks and colorectal, breast, and prostate cancer. Clinical Nutrition, 40(4), 1537–45.
Romieu I, Khandpur N, Katsikari A, Biessy C, Torres-Mejía G, Ángeles-Llerenas A, Alvarado-Cabrero I, Sánchez GI, Maldonado ME, Porras C, Rodriguez AC, Garmendia ML, Chajés V, Aglago EK, Porter PL, Lin M, His M, Gunter MJ, Huybrechts I, Rinaldi S; PRECAMA team (2022) Consumption of industrial processed foods and risk of premenopausal breast cancer among Latin American women: the PRECAMA study. BMJ Nutr Prev Health, 5(1), 1–9
Srour, B., Kordahi, M. C., Bonazzi, E., Deschasaux-Tanguy, M., Touvier, M., & Chassaing, B. (2022). Ultra-processed foods and human health: from epidemiological evidence to mechanistic insights. The Lancet Gastroenterology & Hepatology, S2468–1253(22), 00169–8.
Wang, L., Martínez Steele, E., Du, M., Pomeranz, J. L., O’Connor, L. E., Herrick, K. A., et al. (2021). Trends in Consumption of Ultraprocessed Foods Among US Youths Aged 2–19 Years, 1999–2018. JAMA, 326(6), 519–30.
Wareham, N. J., Jakes, R. W., Rennie, K. L., Schuit, J., Mitchell, J., Hennings, S., et al. (2003). Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutrition, 6(4), 407–13.
Acknowledgements
The authors thank all participants in the EPIC cohort for their invaluable contribution to the study. The authors also thank Bertrand Hémon (IARC) for his precious help with the EPIC database and the National Institute for Public Health and the Environment (RIVM), Bilthoven, the Netherlands, for their contribution and ongoing support to the EPIC Study. We acknowledge the use of data from the EPIC-Oxford cohort.
Disclaimer
Where authors are identified as personnel of the International Agency for Research on Cancer/World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy, or views of the International Agency for Research on Cancer/World Health Organization.
Funding
FMB was supported by a Wellcome Trust PhD studentship in Molecular, Genetic and Lifecourse Epidemiology (224982/Z/22/Z).
The coordination of EPIC is financially supported by IARC and by the Department of Epidemiology and Biostatistics, School of Public Health, Imperial College London which has additional infrastructure support provided by the NIHR Imperial Biomedical Research Centre (BRC). The national cohorts are supported by: Danish Cancer Society (Denmark); Ligue Contre le Cancer, Institut Gustave Roussy, Mutuelle Générale de l’Education Nationale, Institut National de la Santé et de la Recherche Médicale (Inserm) (France); German Cancer Aid, German Cancer Research Center (DKFZ), German Institute of Human Nutrition Potsdam-Rehbruecke (DIfE), Federal Ministry of Education and Research (BMBF) (Germany); Associazione Italiana per la Ricerca sul Cancro-AIRC-Italy, Compagnia di SanPaolo and National Research Council (Italy); Dutch Ministry of Public Health, Welfare and Sports (VWS), Netherlands Cancer Registry (NKR), LK Research Funds, Dutch Prevention Funds, Dutch ZON (Zorg Onderzoek Nederland), World Cancer Research Fund (WCRF), Statistics Netherlands (The Netherlands); Health Research Fund (FIS) - Instituto de Salud Carlos III (ISCIII), Regional Governments of Andalucía, Asturias, Basque Country, Murcia and Navarra, and the Catalan Institute of Oncology - ICO (Spain); Swedish Cancer Society, Swedish Research Council and County Councils of Skåne and Västerbotten (Sweden); Cancer Research UK (14136 to EPIC-Norfolk; C8221/A29017 to EPIC-Oxford), Medical Research Council (1000143 to EPIC-Norfolk; MR/M012190/1 to EPIC-Oxford). (United Kingdom).
The work reported in this paper was performed during Agnès Fournier’s term as a Visiting Scientist at the IARC. This work was supported by Cancer Research UK C33493/A29678; l’Institut National du Cancer (« INCa ») APPEL À PROJET SHS 2021 Grant number: INCa N°2021-138 and APPEL À PROJET 2021 Grant number: INCa N°SHSESP 21-074 and the World Cancer Research Fund (WCRF) Grant reference number: IIG_FULL_2020_033. Researchers were independent from the funders. Funders had no role in the collection, analysis, and interpretation of data, the writing of the report, and the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
The food processing indicators were generated by FR, RBL, IH, GN and CC. The statistical analyses were performed by MC. MC, SY and IH were responsible for drafting the manuscript. All authors had the opportunity to comment on the analysis and interpretation of the findings and approved the final version for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The EPIC cohort was conducted in accordance with the Declaration of Helsinki and received ethical approval from the IARC ethics committee and all study centers. Participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cairat, M., Yammine, S., Fiolet, T. et al. Degree of food processing and breast cancer risk: a prospective study in 9 European countries. Food Prod Process and Nutr 6, 89 (2024). https://doi.org/10.1186/s43014-024-00264-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43014-024-00264-2