Abstract
Background
Difficulty kneeling following total knee arthroplasty (TKA) remains highly prevalent, and has cultural, social, and occupational implications. With no clear evidence of superiority, whether or not to resurface the patella remains debatable. This systematic review examined whether resurfacing the patella (PR) or not (NPR) influences kneeling ability following TKA.
Methods
This systematic review was conducted by following PRISMA guidelines. Three electronic databases were searched utilizing a search strategy developed with the aid of a department librarian. Study quality was assessed using MINROS criteria. Article screening, methodological quality assessment and data extraction were performed by two independent authors, and a third senior author was consulted if consensus was not reached.
Results
A total of 459 records were identified, with eight studies included in the final analysis, and all deemed to be level III evidence. The average MINORS score was 16.5 for comparative studies and 10.5 for non-comparative studies. The total number of patients was 24,342, with a mean age of 67.6 years. Kneeling ability was predominantly measured as a patient-reported outcome measure (PROM), with two studies also including an objective assessment. Two studies demonstrated a statistically significant link between PR and kneeling, with one demonstrating improved kneeling ability with PR and the other reporting the opposite. Other potential factors associated with kneeling included gender, postoperative flexion, and body mass index (BMI). Re-operation rates were significantly higher in the NPR cohort whereas PR cohorts had higher Feller scores, patient-reported limp and patellar apprehension.
Conclusion
Despite its importance to patients, kneeling remains not only under-reported but also ill-defined in the literature, with no clear consensus regarding the optimum outcome assessment tool. Conflicting evidence remains as to whether PR influences kneeling ability, and to clarify the situation, large prospective randomized studies are required.
Similar content being viewed by others
Background
Despite COVID-19 disruptions, 226,350 primary total knee arthroplasties (TKAs) were carried out within England and Wales between January 2018 to December 2020 as per National Joint Registry (NJR) data and it is estimated that, by the year 2030, about 3.48 million TKAs will be performed annually [1, 2]. TKA remains an effective management option for end-stage osteoarthritis (OA) of the knee, and has demonstrated safe and reproducible long-term results with regards to improvement in pain and quality of life. TKA has been shown to significantly improve physiological knee alignment, patient-reported outcome measures (PROMs), functional scores and to confer postural benefits, such as centre of gravity correction and normalization of both pressure and body-weight displacement through the operated limb in the early postoperative period [3]. Regardless of these benefits, approximately one in five patients remain dissatisfied with the outcome of their surgery [4].
Cohort studies revealed that post-TKA satisfaction ranged from 81%–89%, with a large UK cohort study exhibiting that 18.6% of 1217 consecutive patients were either unsure of or dissatisfied with their results one-year post-TKA [4,5,6]. Many factors have been implicated in the post-TKA dissatisfaction, including age, gender, mental health scores, personality traits, preoperative morbidity and pain scores [4]. Rotational alignment of TKA prosthetic components and maintaining correct mechanical axes are related to optimal functional recovery following surgery [7]. A retrospective study defined a new patellar angle to be used in the early diagnosis of prosthetic rotational malalignment, which has been implicated in the prediction of the incidence of anterior knee pain after surgery [7]. Nevertheless, the strongest predictor for dissatisfaction remains unmet patient expectations with regards to functional and symptomatic improvement after surgery [5]. One such outcome measure, which, despite being rated highly important by patients, fails to meet preoperative expectations of improvement, is the ability to kneel [8, 9].
Prost defined kneeling in 1974 as a postural position in which at least one knee is in contact with the ground while body-weight is supported predominantly through the knees [10]. Different positional patterns can fulfill this definition, including single-leg kneeling, upright kneeling, high flexion kneeling and praying position kneeling. Activities of daily living as well as many leisure activities, such as cleaning, decorating, gardening, sports, and exercise, are impacted by an inability to kneel, with patients often needing adjustments or relying on support from friends and family to compensate, negatively impacting their emotional state, social independence, and well-being [11]. Kneeling is also an important function for dining and social participation in east Asian cultures [12] and of religious practice among both the Christian and Islamic faith, with followers of the latter requiring high flexion kneeling for daily prayer [13, 14]. Many occupations require kneeling, such as plumbing, cleaning, roofing and floor laying [15]. Despite its importance, kneeling remains the activity least improved following surgery, with one-third of patients not returning to work following TKA [16].
Kneeling ability is consistently the poorest of the patient-reported outcome measures (PROMs) following TKA and remains prevalent in both the short and longer terms, with one study revealing that 67% of patients reported much difficulty or found it impossible to kneel five years after TKA [17]. Kneeling ability is usually assessed as a self-reported outcome measure. Its assessment commonly uses question seven of the Oxford Knee Score (OKS), which rates it on a five-point ordinal scale, ranging from 4 ("yes, easily") to 0 ("no, impossible"). The OKS has been adopted by the UK government and the NJR as a validated tool to assess outcomes [4].
Associations between intraoperative variables and postoperative kneeling ability have been investigated with contradictory results. One such variable is whether or not to resurface the patella during TKA, which remains largely at the discretion of the operating surgeon [11, 18]. This review investigated whether PR or NPR influences the ability to kneel following TKA.
Methods
This systematic review was conducted by following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [19] and was registered with PROSPERO (International Prospective Register of Systematic Reviews), (ID = CRD42022306341) [20].
Search strategy and eligibility criteria
A systematic search strategy and syntax were developed with the aid of the department librarian. A combination of Medical Subject Heading (MeSH) terms and keywords were incorporated to electronically search EMBASE and Medline libraries using Healthcare Database Advanced Search (HDAS) and the native PubMed database from inception to October 2021 (Table 1). An additional grey literature search was performed using Open Grey, and the reference lists of included studies were reviewed to identify articles missed by the original search strategy.
Inclusion criteria were (1) Studies involving patients undergoing a TKA, with PR or NPR, with kneeling outcomes reported, (2) Papers published in English with full text available, (3) Peer reviewed clinical studies. Exclusion criteria included (1) Studies presenting non-original data, case reports, review studies, conference abstracts, editorials, opinion papers and letters to the editor. (2) Mixed cohort of patellar resurfaced (PR)/non-resurfaced (NPR) TKA patients with no direct comparative analysis of kneeling outcomes.
Article screening
Duplicates were removed from the list of papers identified. Titles and abstracts were screened by two independent reviewers (OAS, CS), who then screened the full-text papers of relevant studies. The final study selection was completed by two independent reviewers as per pre-defined inclusion/exclusion criteria. Any inconsistencies were discussed with a third, senior reviewer (DHS) available for consultation if consensus was not achieved.
Level of evidence and methodological quality
The methodological quality of the studies was scored by two independent reviewers (OAS, CS) using the Methodological Index for Non-Randomized Studies (MINORS) tool [21]. The level of evidence of each study was reported by two reviewers as per the Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence [22]. Critical appraisal of included studies was performed by two independent reviewers (OAS, CS) with a third, senior reviewer (DHS) present to resolve potential failure to reach a consensus.
Data extraction
Two independent authors (OAS, CS) extracted data from the included studies, comprising study characteristics, patient demographics, implant characteristics, surgical details, details of kneeling outcomes compared between PR and NPR, details of variables associated with kneeling outcomes other than PR, variables other than kneeling compared between PR and NPR cohorts, study conclusions and limitations.
Based on the heterogeneity in study data particularly in the tools utilized to assess kneeling ability, it was decided a quantitative meta-analysis was not feasible.
Results
Search results
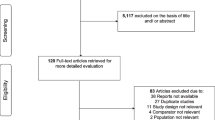
The electronic search of the EMBASE and Medline libraries via HDAS and the native PubMed database identified 459 articles. After removing duplicates and irrelevant records based on titles and abstracts, nine articles were eligible for full-text screening. One additional record was identified by reviewing reference list of a relevant review article. No articles were identified by a search of grey literature. Full texts for a total of ten articles were screened with two records excluded as per inclusion/exclusion criteria, leaving eight records included in the final qualitative analysis of the review (Fig. 1).
Risk of bias and quality assessment
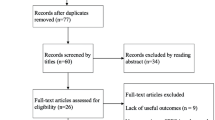
All eight studies included were of retrospective cohort design with a level of evidence of III [23,24,25,26,27,28,29,30]. Average MINORS score was 16.5 (SD = 1.98) for comparative studies [23, 25,26,27,28,29] and 10.5 (SD = 0.5) for non-comparative studies [24, 30]. Risk of bias assessed using MINORS criteria is presented in Fig. 2. Table 2 shows the level of evidence and quality assessment of each study included.
Study and cohort characteristics
All eight studies were published between 2002 and 2020. Four were UK-based, with one each from the USA, Canada, Australia, and Switzerland (Table 2). The total number of patients involved in the studies was 24,342, with a mean age of 67.6 years (range 63.4–71.6) of the studies that reported this. The total number of patients was 8,625 in the PR cohort and was 15,689 in NPR cohort, with one study not reporting the number of patients by whether they had PR or NPR. Cohort characteristics are detailed in Table 3.
Assessment of kneeling ability
All eight studies recorded kneeling as a PROM. One study used question SP5 from the Knee Injury and Osteoarthritis Outcome Score (KOOS) [27]. One study used question 7 of the OKS [28], with another using cumulative sum of questions 5,7 and 12 of the OKS to assess kneeling [25]. The remaining five studies used non-validated questionnaires [23, 24, 26, 29, 30]. Two studies utilized an additional objective clinical assessment to report kneeling outcomes [26, 30] and the details regarding objective and subjective measured kneeling outcomes are presented in Table 3.
Surgical techniques and implant characteristics
Three studies used a cruciate-retaining (CR) implant preserving the posterior cruciate ligament (PCL) [23, 29, 30], one used a medial rotation design sacrificing the PCL [25] and one used CR implants in 56% of cases and a cruciate sacrificing (CS) implant in 44% [24]. Three studies did not report on the implant used [26,27,28] (Table 4).
In two studies, a medial parapatellar approach [25, 30] was used, and in one, either a medial parapatellar or a subvastus approach [23] was used, with the remaining studies not reporting the approach. None of the eight studies reported the specifics of the skin incision or whether mobile or fixed-bearing prostheses were used. One study documented that drains had not been used [25].
Kneeling ability following TKA
Two studies reported a statistically significant link between PR and kneeling following TKA [23, 26]. Huish et al. reported a significantly greater (64% vs. 39%) ability to kneel with NPR at 2.5 years follow-up, with the ability to kneel defined as patients reporting that they could kneel easily, with little or moderate difficulty [23]. In contrast, Wilding et al. employed an objective assessment of kneeling ability, with inability defined as being unable to kneel on either a soft couch or hard floor due to discomfort or pain. They found that 78.6% of patients with PR were able to kneel compared to 45.6% of NPR patients, with the difference being statistically significant [26] (Tables 5, 6).
Sangoi et al. used the summation of OKS questions 5, 7 and 12 to assess self-reported kneeling ability, although only question 7 is specifically about kneeling. They showed that the PR cohort reported greater improvements compared to the NPR group, and the improvement postoperatively was statistically significant for the PR group but not the NPR group [25]. Baker et al. reported a statistically significant difference between pre- and postoperative self-reported kneeling scores measured using question 7 of the OKS between the PR and the NPR cohorts, but this was not significant once adjusted for multivariate analysis [28]. None of the other studies reported a statistically significant difference in kneeling outcomes between PR and NPR patients (Table 6).
Huish Jr et al. reported that kneeling ability was significantly higher in female patients [23], but conversely, Rooks et al. found that males were significantly more likely to self-report being able to kneel [24]. Although age and type of implant did not impact kneeling ability in their study, they also reported an inverse relationship between body mass index (BMI) and kneeling ability, with patients having a BMI greater than 33 being significantly less likely to be able to kneel [24]. Palmer et al. reported no significant link between postoperative flexion or Knee Society Score (KSS) and kneeling ability [30], although Wilding et al. reported a significant link between postoperative flexion and kneeling ability, with knee flexion to 100° or greater demonstrating a higher ability to kneel [26]. Age, status of PCL, or type of surgery (revision vs. primary) did not influence kneeling ability and variables other than PR and their impact on kneeling are presented in Table 7.
Patellar resurfacing vs. non-resurfacing
Outcomes other than kneeling compared between PR and NPR are presented in Table 8. Huish Jr et al. reported no significant difference in OKS scores between PR and NPR patients [23]. This was also reported by Sangoi et al. and Baker et al., who found no significant difference in either pre- or postoperative OKS scores when comparing the PR and NPR groups [25, 28]. Garneti et al. found no significant difference in the PR and NPR groups when comparing Euroqol scores and KSS scores [29], with Albrecht et al. also reporting no difference in KSS scores [27]. Sangoi et al. reported higher Feller scores in the PR group [25]. Garneti et al. reported a significantly higher revision rate in the NPR group but higher patient-reported limp and patellar apprehension in the PR group [29]. Albrecht et al. found no significant differences in ROM or revision rates [27].
Discussion
There remains a sparsity of literature directly comparing kneeling outcomes between PR and NPR cohorts of patients receiving TKA. Of the studies identified in the systematic search process of this review, only two reported statistically significant findings, with one study favoring PR [26] and another favoring NPR [23].
Wilding et al. reported significantly improved kneeling ability after TKA with PR [26]. Kneeling involves flexion angles of between 120 to 150 degrees, retention of the medial pivot of the medial femoral condyle with posterior movement of the lateral femoral condyle and internal tibial rotation [31]. Early TKA designs neglected the patellofemoral joint (PFJ), and until in 1974, resurfacing of the patella using a polyethylene dome was introduced with the Insall-Burstein total condylar replacement (Zimmer, Warsaw, IN, USA). However, PR presented its own complications, leading to disagreement in the orthopedic community with regards to the optimal intraoperative management of the patella [32]. PR allows for the optimization of modern ‘patellar friendly designs’ by providing an improved congruence between the patella and flange implant surfaces, negating morphological and anatomical variations that may be present in the native patellae. This can improve patellar tracking and overall flexion [33], theoretically positively impacting kneeling ability.
Conversely, Huish et al. reported that NPR patients had a higher self-reported ability to kneel [23]. Resurfacing the patella can also lead to complications that can impact kneeling ability, such as instability, dislocation, aseptic loosening, overstuffing of the PFJ and patellar clunk syndrome [32]. The articulating surface of the patella changes during flexion with patellofemoral pressures peaking at around 90–120 degrees [34] and during high flexion activities, computational and biomechanical studies have demonstrated that the patella undergoes significant sagittal strains that increase inversely to the residual thickness of the patella [35]. Over-resection of the patella during PR can therefore predispose to an increased risk of fracture and pain in deep flexion impacting kneeling ability.
It is important to note that Huish Jr et al. reported kneeling ability as a PROM whereas Wilding et al. additionally assessed kneeling ability clinically. Self-reported kneeling ability has been shown to be inferior to observed kneeling ability [36] and a study comparing TKA, uni-compartmental knee arthroplasty and PFJ replacement reported that, while only 37% of patients thought that they could kneel, 81% were actually able to do so [37]. Palmer et al. found that patients avoided kneeling after TKA for fear of harming the prosthesis and that there were uncertainties regarding the advice given by doctors and nurses [30]. It is uncertain as to why kneeling avoidance advice is given but could be due to concerns regarding wound infection in the early postoperative phase or kinematic concerns regarding increasing patellar loads during high flexion activities, but patient education programs have been shown to improve patient-reported kneeling ability postoperatively [38]. Despite discordance between perceived and actual kneeling ability, six of the eight studies in this review only assessed kneeling as a PROM, with the remaining two also using an additional objective clinical assessment.
Huish Jr et al., however, conducted a follow-up of longer period (both for PR and NPR cohorts) for their study when compared to Wilding et al. This is significant as kneeling PROMs have been shown, in a large prospective study of 5,600 OKS questionnaires, to drastically improve up to a year following surgery and subsequently worsen in the years thereafter, which might be explained by old age of the subjects [39]. In addition, Wilding et al. reported a higher MINORS score when compared to Huish Jr et al., indicating a more robust overall methodological quality (Table 2).
Whether or not to resurface the patella remains a contentious topic, with a lack of clear evidence supporting one technique over the other. A meta-analysis of RCTs in 2005 commented on an increased risk of re-operation with NPR [40] and these findings were echoed in more recent reviews and meta-analyses [41, 42]. In contrast, an RCT comparing PR and NPR in patients with bilateral TKA found no significant difference in revision rates at 10 years [43]. Of the studies included in this review, a study by Garneti et al. reported a significantly increased re-operation rate in the NPR cohort [29], but Huish Jr et al. and Albrecht et al. found no significant difference [23, 27], although it is important to note that, despite absence of statistical significance, both studies reported higher re-operation rates in the NPR group.
Conflicting evidence has also been presented with regards to whether PR influences PROMs. One study found no significant difference in the IKS function score [37] while another reported no short-term differences in terms of KSS scores, but found a significant difference at a longer-term follow-up of five years [41]. Most studies included in this review reported no significant difference with regards to OKS, KSS, Euroqol or Baldini scores. Sangoi et al. did report improved Feller scores for PR, which includes items on anterior knee pain and stair climbing [25] but Garneti et al. found higher rates of patient-reported limp and patellar apprehension in the PR group [29].
Many studies reported no difference between posterior-stabilized (PS) and cruciate-retaining (CR) designs with regards to clinical, functional and radiological outcomes [44, 45]. However, PS knees have been shown to demonstrate higher ROM when compared to CR designs, with some high flexion prostheses having been shown to improve kneeling outcomes [45,46,47]. Wilding et al. reported that favorable kneeling outcomes remained independent of whether the PCL was retained or sacrificed [26].
Skin incision has been shown to impact kneeling ability, with a recent systematic review and meta-analysis reporting that patients had improved odds of kneeling with anterolateral incisions compared to anteromedial incisions; a transverse incision compared to a longitudinal incision and a shorter incision compared to a longer one [48]. Longer and anteromedial incisions have been reported to result in larger areas of cutaneous sensory change, which can subsequently impact kneeling ability negatively [49, 50]. Two studies in this review used a medial parapatellar approach [25, 30], with one study utilizing a combination of medial parapatellar and subvastus approaches [23] but none of the included studies specifically commented directly on the effect of the type, size or location of the skin incision used.
One of the non-surgical variables associated with kneeling ability is postoperative ROM. Most kneeling postures are high flexion activities with a minimum of 90 degrees of knee flexion required. Wilding et al. reported that knees that were able to flex to at least 100 degrees had significantly improved chances of kneeling [26], which is consistent with studies demonstrating that high flexion TKA designs improved postoperative flexion by 15–25 degrees and also improved the ability to kneel, squat and sit cross-legged [47]. Palmer et al. found the mean ROM was 114 degrees in patients able to kneel and 110 degrees in those unable to do so, but this was not statistically significant [30].
Other non-surgical factors associated with kneeling ability include BMI and gender. An inverse relationship between kneeling ability and BMI has been reported in the literature [51]. This may simply be due to increased amounts of adipose tissue resulting in earlier contact between the posterior thigh and lower leg, thus preventing deep flexion and kneeling, and one study reported that lower BMI was associated with improved kneeling ability in upright and single-leg kneeling positions [52], although another demonstrated no significant relationship between BMI and short-term functional performance following TKA [53]. Rooks et al. reported that patients with a BMI more than 33 were significantly less likely to be able to kneel [24].
Morphological differences between male and female knees previously led to the development of gender-specific implants, but studies looking at whether these differences result in variation in clinical and functional outcomes between men and women have produced conflicting findings [54, 55]. Rooks et al. reported that males were significantly more likely to be able to kneel [24], which was consistent with the findings of a retrospective cohort analysis of 404 patients [51]. Conversely, Huish Jr et al. reported kneeling ability to be higher in females [23]. Age, revision as opposed to primary surgery, and KSS scores were not significantly associated with kneeling ability post-TKA [24, 26, 30].
Limitations
Kneeling and the ability to kneel are poorly defined and infrequently reported in the literature, limiting the number of studies appropriate for inclusion. Variability also remains in how this outcome is assessed, often using Question 7 of the OKS or Question SP5 of the KOOS. There are, however, issues, because Question 7 of the OKS is not designed to be used in isolation to assess kneeling ability and neither question considers kneeling position, kneeling duration, the surface knelt upon, social, cultural or occupational importance. There is also variability with regards to how kneeling is assessed, which makes comparisons difficult. Due to the heterogeneous nature of the data, it was not possible to perform a meta-analysis.
Comparing PR and NPR is difficult because there is a lack of standardization in the reporting of the surgical techniques and designs of implants used. There are also various options available to the surgeon with regards to the intraoperative management of the patella, including circumpatellar dennervation, osteophyte removal, patelloplasty and lateral retinacular release, which can be performed in isolation or combination, but once again, but these were not clearly reported.
Kneeling is a complex multi-joint movement and hence also is affected by global disease, with arthritis of the spine, hips or contralateral knee affecting kneeling ability regardless of the postoperative outcomes of a TKA.
Conclusions
Despite being highly important to patients and known to impact patient satisfaction, kneeling remains ill-defined, under-reported and under-investigated as an outcome measure. The available data regarding intra-operative variables such as PR and its impact on postoperative kneeling ability consists largely of small retrospective studies with no randomized studies identified in the systematic search of this review process. The results were conflicting, with a statistically significant association being identified in only two studies, one favoring PR and the other NPR. Other factors associated significantly with kneeling included BMI, postoperative flexion, and gender, with one study favoring females and the other males. No significant differences were observed between PR and NPR with regards to OKS, KSS and Euroqol scores. However, an increased rate of re-operation was reported in the NPR group. In the absence of large, randomized data sets comparing kneeling ability in PR and NPR patients, it is difficult to reach meaningful conclusions. In order to clarify the situation, large, long-term prospective randomized controlled studies (RCTs) are required with clear definitions of what kneeling entails and how to assess it best, so that standardized reporting can be performed and compared.
Availability of data and materials
Not applicable.
Abbreviations
- CR:
-
Cruciate-retaining
- CS:
-
Cruciate-sacrificing
- HDAS:
-
Healthcare database advanced search
- IKS:
-
International knee society
- KOOS:
-
Knee injury and osteoarthritis outcome score
- KSS:
-
Knee society score
- MeSH:
-
Medical subject heading
- MINORS:
-
Methodological index for non-randomised studies
- NJR:
-
National joint registry
- NPR:
-
Non-patellar resurfacing
- OA:
-
Osteoarthritis
- OCEBM:
-
Oxford centre for evidence-based medicine
- OKS:
-
Oxford knee score
- PCL:
-
Posterior cruciate ligament
- PFJ:
-
Patellofemoral joint
- PR:
-
Patellar resurfacing
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- PROM:
-
Patient-reported outcome measure
- PROSPERO:
-
International prospective register of systematic reviews
- RCT:
-
Randomized control trial
- ROM:
-
Range of movement
- TKA:
-
Total knee arthroplasty
References
Gemayel AC, Varacallo M. Total knee replacement techniques. 2022 Sep 4. In: StatPearls. Treasure Island: StatPearls Publishing; 2023.
Ben-Shlomo Y, Blom A, Boulton C, Brittain R, Clark E, Dawson-Bowling S, et al. The national joint registry 18th annual report 2021. London: National Joint Registry; 2021.
Notarnicola A, Maccagnano G, Fiore A, Spinarelli A, Montenegro L, Paoloni M, et al. Baropodometry on patients after total knee arthroplasty. Musculoskelet Surg. 2018;102(2):129–37. Available from: https://pubmed.ncbi.nlm.nih.gov/28971359/. cited 2023 Jan 7.
Scott CEH, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br. 2010;92(9):1253–8.
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57.
Bourne RB, Chesworth B, Davis A, Mahomed N, Charron K. Comparing patient outcomes after THA and TKA: is there a difference? Clin Orthop Relat Res. 2010;468(2):542–6.
Spinarelli A, Pesce V, Campagna C, Maccagnano G, Moretti B. Painful knee prosthesis: CT scan to assess patellar angle and implant malrotation. Muscles Ligaments Tendons J. 2016;6(4):461. [Cited 2023 Jan 8]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5310746/.
Neuprez A, Delcour JP, Fatemi F, Gillet P, Crielaard JM, Bruyère O, et al. Patients’ expectations impact their satisfaction following total hip or knee arthroplasty. PLoS One. 2016;11(12):e0167911.
Tilbury C, Haanstra TM, Leichtenberg CS, Verdegaal SHM, Ostelo RW, de Vet HCW, et al. Unfulfilled expectations after total hip and knee arthroplasty surgery: there is a need for better preoperative patient information and education. J Arthroplasty. 2016;31(10):2139–45.
Prost J. Varieties of human posture. Hum Biol. 1974;46(1):1–19.
Fletcher D, Moore AJ, Blom AW, Wylde V. An exploratory study of the long-term impact of difficulty kneeling after total knee replacement. Disabil Rehabil. 2019;41(7):820–5.
Sitting on the floor versus sitting on a chair - PubMed. [cited 2022 Jan 7]. Available from: https://pubmed.ncbi.nlm.nih.gov/4792150/
Acker SM, Cockburn RA, Krevolin J, Li RM, Tarabichi S, Wyss UP. Knee kinematics of high-flexion activities of daily living performed by male Muslims in the Middle East. J Arthroplasty. 2011;26(2):319–27.
Benfayed R, Hamilton D, Moran M, Simpson A, Macdonald D. Interpretation of kneeling citation for published version: orthopedic & muscular system: current research interpretation of kneeling. Orthop Muscular Syst. 2017;6:3.
Ditchen DM, Ellegast RP, Gawliczek T, Hartmann B, Rieger MA. Occupational kneeling and squatting: development and validation of an assessment method combining measurements and diaries. Int Arch Occup Environ Health. 2015;88(2):153–65.
Kievit AJ, Van Geenen RCI, Kuijer PPFM, Pahlplatz TMJ, Blankevoort L, Schafroth MU. Total knee arthroplasty and the unforeseen impact on return to work: a cross-sectional multicenter survey. J Arthroplasty. 2014;29(6):1163–8.
Vikki Wylde, Sam Dixon, Laura Miller, Michael R Whitehouse, Ashley W Bloo. 5 Year Outcomes and Survivorship of the Triathlon Total Knee Replacement: A Cohort Study. G. Balint, Antala B, Carty C, Mabieme JMA, Amar IB, Kaplanova A, editors. Acta Orthop Belg. 2017;83(2):259–67.
Li S, Chen Y, Su W, Zhao J, He S, Luo X. Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthop. 2011;35(3):305.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
PROSPERO. [cited 2022 Jan 8]. Available from: https://www.crd.york.ac.uk/prospero/
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–6.
OCEBM Levels of Evidence — Centre for Evidence-Based Medicine (CEBM), University of Oxford. [cited 2022 Jan 8]. Available from: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence
Huish EG, Coury JG, Ummel JR, Deans JT, Cohen J, Casey JJ. Higher rate of kneeling after primary knee arthroplasty without patellar resurfacing at midterm review. J Orthop. 2020;20:204. [cited 2022 Jan 9]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6997512/.
Rooks K, Houdek D, Obaid H, Dust W. Primary total knee arthroplasty: correlation between preoperative radiographic severity of arthritis and postoperative patient satisfaction. J Knee Surg. 2021;34(13):1441–5.
Sangoi D, Gokhale N, Kulkarni S, Kodumuri P, Kothari P, Kulkarni S. Does patellar resurfacing matter? Midterm follow-up of MRK total knee replacement. Indian J Orthop. 2020;55(Suppl 1):56–61.
Wilding CP, Snow M, Jeys L. Which factors affect the ability to kneel following total knee arthroplasty? An outpatient study of 100 postoperative knee replacements. J Orthop Surg (Hong Kong). 2019;27(3):2309499019885510. Available from: https://pubmed.ncbi.nlm.nih.gov/31709898/. [cited 2022 Jan 9].
Albrecht DC, Ottersbach A. Retrospective 5-year analysis of revision rate and functional outcome of TKA with and without patella implant. Orthopedics. 2016;39(3 Suppl):S5-31.
Baker PN, Petheram T, Dowen D, Jameson SS, Avery PJ, Reed MR, et al. Early PROMs following total knee arthroplasty–functional outcome dependent on patella resurfacing. J Arthroplasty. 2014;29(2):314–9.
Garneti N, Mahadeva D, Khalil A, McLaren CA. Patellar resurfacing versus no resurfacing in Scorpio total knee arthroplasty. J Knee Surg. 2008;21(2):97–100.
Palmer SH, Servant CT, Maguire J, Parish EN, Cross MJ. Ability to kneel after total knee replacement. J Bone Joint Surg Br. 2002;84(2):220–2.
Galvin CR, Perriman DM, Newman PM, Lynch JT, Smith PN, Scarvell JM. Squatting, lunging and kneeling provided similar kinematic profiles in healthy knees-A systematic review and meta-analysis of the literature on deep knee flexion kinematics. Knee. 2018;25(4):514–30.
Abdel MP, Parratte S, Budhiparama NC. The patella in total knee arthroplasty: to resurface or not is the question. Curr Rev Musculoskelet Med. 2014;7(2):117.
Benazzo F, Perticarini L, Jannelli E, Ivone A, Ghiara M, Rossi SMP. Controversy: supporting patellar resurfacing in total knee arthroplasty – do it. EFORT Open Rev. 2020;5(11):785.
McConaghy K, Derr T, Molloy RM, Klika AK, Kurtz S, Piuzzi NS. Patellar management during total knee arthroplasty: a review. EFORT Open Rev. 2021;6(10):861.
Abo-Alhol TR, Fitzpatrick CK, Clary CW, Cyr AJ, Maletsky LP, Laz PJ, et al. Patellar mechanics during simulated kneeling in the natural and implanted knee. J Biomech. 2014;47(5):1045–51.
Schai PA, Gibbon AJ, Scott RD. Kneeling ability after total knee arthroplasty. perception and reality. Clin Orthop Relat Res. 1999;(367):195–200.
Hassaballa MA, Porteous AJ, Newman JH. Observed kneeling ability after total, unicompartmental and patellofemoral knee arthroplasty: perception versus reality. Knee Surg Sports Traumatol Arthrosc. 2004;12(2):136–9.
Jenkins C, Barker KL, Pandit H, Dodd CAF, Murray DW. After partial knee replacement, patients can kneel, but they need to be taught to do so: a single-blind randomized controlled trial. Phys Ther. 2008;88(9):1012–21.
Williams DP, Blakey CM, Hadfield SG, Murray DW, Price AJ, Field RE. Long-term trends in the Oxford knee score following total knee replacement. J Bone Joint Surgery - Series B. 2013;95 B(1):45–51. [Cited 2023 Jan 18]. Available from: https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.95B1.28573.
Nizard RS, Biau D, Porcher R, Ravaud P, Bizot P, Hannouche D, et al. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res. 2005;432(432):196–203.
Chen K, Li G, Fu D, Yuan C, Zhang Q, Cai Z. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: a meta-analysis of randomised controlled trials. Int Orthop. 2013;37(6):1075–83. BioMed Central Ltd.
Parsons T, Al-Jabri T, Clement ND, Maffulli N, Kader DF. Patella resurfacing during total knee arthroplasty is cost-effective and has lower re-operation rates compared to non-resurfacing. J Orthop Surg Res. 2021;16:185.
Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL. A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res. 2007;464:65–72. https://doi.org/10.1097/BLO.0b013e31812f783b.
Tanzer M, Smith K, Burnett S. Posterior-stabilized versus cruciate-retaining total knee arthroplasty: balancing the gap. J Arthroplasty. 2002;17(7):813–9.
Jiang C, Liu Z, Wang Y, Bian Y, Feng B, Weng X. Posterior cruciate ligament retention versus posterior stabilization for total knee arthroplasty: a meta-analysis. PLoS One. 2016;11(1):e0147865.
Longo UG, Ciuffreda M, Mannering N, D’Andrea V, Locher J, Salvatore G, et al. Outcomes of posterior-stabilized compared with cruciate-retaining total knee arthroplasty. J Knee Surg. 2018;31(4):321–40.
Jain S, Pathak AC, Kanniyan K, Kulkarni S, Tawar S, Mane P. High-flexion posterior-stabilized total knee prosthesis: Is it worth the hype? Knee Surg Relat Res. 2013;25:100–5. BioMed Central Ltd.
Nadeem S, Mundi R, Chaudhry H. Surgery-related predictors of kneeling ability following total knee arthroplasty: a systematic review and meta-analysis. Knee Surg Relat Res. 2021;33:36. BioMed Central Ltd.
Tsukada S, Kurosaka K, Nishino M, Hirasawa N. Cutaneous hypesthesia and kneeling ability after total knee arthroplasty: a randomized controlled trial comparing anterolateral and anteromedial skin incision. J Arthroplasty. 2018;33(10):3174–80.
Hassaballa M, Artz N, Weale A, Porteous A. Alteration in skin sensation following knee arthroplasty and its impact on kneeling ability: a comparison of three common surgical incisions. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):1983–7.
Sabeh KG, Hernandez VH, Cohen-Levy WB, Ong A, Orozco F, Bennett V, et al. The effects of patient occupation, hobbies, and body mass index on kneeling after total knee arthroplasty. J Knee Surg. 2021;34(7):772–6.
Scott CEH, Holland G, Gillespie M, Keenan OJ, Gherman A, MacDonald DJ, et al. The ability to kneel before and after total knee arthroplasty: the role of the pattern of osteoarthritis and the position of the femoral component. Bone Joint J. 2021;103-B(9):1514–25.
Stevens-Lapsley JE, Petterson SC, Mizner RL, Snyder-Mackler L. Impact of body mass index on functional performance after total knee arthroplasty. J Arthroplasty. 2010;25(7):1104–9.
Nassif JM, Pietrzak WS. Clinical outcomes in men and women following total knee arthroplasty with a high-flex knee: no clinical effect of gender. Sci World J. 2015;2015:285919.
Lim JBT, Chi CH, Lo LE, Lo WT, Chia SL, Yeo SJ, et al. Gender difference in outcome after total knee replacement. J Orthop Surg. 2015;23(2):194–7.
Acknowledgements
The authors would like to thank Irrum Afzal, Research Manager at the Academic Surgical Unit, South West London Elective Orthopaedic Centre, for her continued support and guidance. We are also grateful to Potenza Atiogbe, Multi-professional Education and Library Services Manager at Epsom and St Helier’s NHS Foundation Trust, for her help in assisting with the formulation of the search strategy for the review process along with acquisition of full-text articles.
Funding
This project did not receive any external or internal funding.
Author information
Authors and Affiliations
Contributions
All the authors have contributed significantly to and take public responsibility for study design, data acquisition along with the analysis and interpretation of the data. All authors have been involved in the revision and approval of the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have read the final version of the manuscript and confirm consent for publication.
Competing interests
All authors confirm no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shah, O.A., Spence, C., Kader, D. et al. Patellar resurfacing and kneeling ability after total knee arthroplasty: a systematic review. Arthroplasty 5, 32 (2023). https://doi.org/10.1186/s42836-023-00184-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42836-023-00184-5