Abstract
Background
Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis accounts for the vast majority of cases of autoimmune encephalitis. Its common clinical symptoms are psychiatric symptoms, behavioral dysfunction, seizures, speech impairment, cognitive impairment, movement disorders, decreased consciousness, and autonomic instability. This report was aimed to provide evidence for anti-NMDAR encephalitis with seizure-like activity, based on the clinical presentations, brain magnetic resonance imaging (MRI), and electroencephalogram (EEG) recordings.
Case presentation
We report a 11-year-old girl who suffered epigastric pain after vigorous physical activity. She felt weakness of the muscles. She had syncope only once and urinary incontinence on the way to the hospital and vomited at the arrival. The entire procedure lasted approximately 15 min. The next night she had recurrent headache attacks along with irritability, like someone “tapping” to the right occipital region. She experienced numbness in the left upper limbs and shallowing of the frontal lines on the left side. Holter monitoring showed normal findings, but brain MRI, EEG recording, and cerebrospinal fluid (CSF) antibody testing showed abnormal results. The patient was finally diagnosed with anti-NMDAR encephalitis. After treatment with glucocorticoids and acyclovir, she fully recovered and was discharged from the hospital.
Conclusions
Although the patient presented with pain and impaired limb movements, she did not have respiratory or (and) circulatory failure, and the symptoms entirely resolved. Early accurate diagnosis and timely treatment are essential for patients with anti-NMDAR encephalitis.
Similar content being viewed by others
Background
Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis accounts for the vast majority of autoimmune encephalitis cases, with common clinical symptoms including seizures, psychiatric symptoms, behavioral dysfunction, movement disorders, speech impairment, and autonomic instability [1]. Without imediate treatment, the significant complications would cause more severe adverse outcomes. Therefore, early accurate diagnosis and timely treatment of anti-NMDAR encephalitis are critical for the outcomes. As the clinical manifestations of anti-NMDAR encephalitis are complicated and varied, it is often misdiagnosed, which would delay the formal treatment.
Here, we report a 11-year-old Chinese girl with anti-NMDAR encephalitis who had seizure-like activity and left hemiplegia, with abnormal findings from brain MRI, EEG recording and cerebrospinal fluid (CSF) antibody testing during disease progression.
Case presentation
The patient was an 11-year-old girl weighing 33.5 kg, who was presented to the cardiovascular medicine department with syncope after vigorous physical activity. The entire procedure lasted approximately 15 min, during which she had urinary incontinence and vomited. One day later, she had a severe headache attack and experienced left hemiplegia. She had a temperature of 37.6 °C, a heart rate of 102 beats per minute, a breathing rate of 20 beats per minute, and a blood pressure of 93/51 mmHg. Because of the fixed region of the headache and hemiplegia (numbness with decreased muscle strength), while heart rate and blood pressure were normal, a hemiplegic syndrome (episodic), hemiplegic migraine with suspected stroke-like episodes, or cerebral vasospasm due to thrombosis was considered for the patient. Brain magnetic resonance imaging (MRI) showed abnormal findings, while magnetic resonance angiography (MRA), magnetic resonance venography (MRV), and diffusion-weighted imaging (DWI) examinations all had normal findings. As the patient was restless, we used midazolam for sedation and she fell asleep at night. The radiologist considered an intracranial infection because the patient had fever at admission. Then ceftriaxone (anti-infection), dexamethasone (reduction of cerebral edema) and levocarnitine (nutrition of cerebral nerve) were used. The next day she was transferred to the department of neurology and underwent other examinations. The long-range EEG recording showed slow waves, but the CSF routine biochemical, etiologic, and cellular examinations, the chest computed tomography (CT) scan, the abdominal and gynecological ultrasound, and the testing for tumor markers all showed normal results.
To verify if this case was autoimmune encephalitis, we performed autoimmune encephalitis-related examinations in serum and CSF. The results showed CSF was positive for anti-NMDAR IgG (1:1 titer), and the final diagnosis was made as anti-NMDAR encephalitis. The patient received methylprednisolone treatment (i.v., 4 mg/kg on the first day, 15 mg/kg on the second and third days, 10 mg/kg on the fourth day, and 4 mg/kg on the fifth day) to modulate immunity. When all symptoms had entirely resolved, she was discharged for observation. MRI lesions disappeared at the 2-week follow-up.
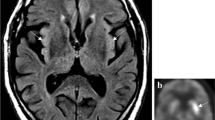
The brain MRI, EEG recording and CSF antibody testing results are shown in Figs. 1, 2, 3, 4.
The T1WI phase (a), T2WI phase (b), T2 flair phase (c), and DWI phase (d) of brain MRI of the patient. Brain MRI showed hyperintensity of the right central sulcus and the temporal parietal lobe in the T2 flair phase. The MRI lesions disappeared at 2-week follow-up. The long arrows refer to the central sulcus and the short arrows refer to the temporal parietal lobe
Discussion
The clinical manifestations of anti-NMDAR encephalitis are complicated and varied. In severe cases, respiratory and circulatory disturbances occur and may lead to death. Flu-like symptoms such as headache can be present at the beginning of the illness, but intense pain at the site of the head has not been described in literature. The symptoms of this case were like the seizure activity. Slow waves were shown on EEG, but the characteristic “extreme delta brush” [2, 3] was not seen. There might be some unspecific abnormalities in this patient. In anti-NMDAR encephalitis, diffuse slowing is usually more often seen with or without epileptic discharges, while focal slowing is relatively uncommon, unless with active epileptiform discharges. So we considered this patient as having focal seizures with impaired awareness. Although the clinical symptoms did not fully match the typical features of this disease, CSF examination showed positive results for anti-NMDAR IgG, which pointed out to the diagnosis of anti-NMDAR encephalitis.
In south China, the median age of onset is about 7 years, females are affected more often than males, and movement disorders are the most common symptoms at the onset or during the course of anti-NMDAR encephalitis. In addition, this disease is rarely seen with tumors, most patients respond well to the immunity-modulating treatments, they have a favorable prognosis, and the case fatality rate is low [4]. Impaired unresponsive consciousness and seizures could occur with anti-NMDAR encephalitis [5], with the most common onset being generalized tonic seizures and the most common movement disorder being weakness of muscles of facial expression [6]. However, these symptoms were not fully compatible with this case. Anti-NMDAR encephalitis is divided into three types based on clinical presentation [7]: disease duration less than 60 days with symptoms of coma as type I and with mental and behavioral disorders as type II, and disease duration more than 60 days with stressful mental status as type III. The present case belonged to the type I according to her clinical presentations.
The current pathogenesis of anti-NMDAR encephalitis is associated with tumor and (or) former viral infections [8]. Previous animal studies showed that all symptoms completely disappeared when IgG antibodies were removed, suggesting that the antibody-mediated dysregulation of NMDAR function and reduction of the specific density underlie the pathology of various psychiatric symptoms observed in patients [9]. The patient received abdominal and gynecological ultrasound to exclude tumor and she had fever during the disease, so we considered a prodromal viral infection and acyclovir was used for 1 week, even if the herpes simplex virus was not detected in the serum and CSF. However, re-check of abdominal and gynecological ultrasound was not performed when the patient was re-examined by brain MRI. We also know that teratoma have a delayed arrival, so the abdominal and gynecological ultrasounds should be performed in her follow-ups.
The patient suffered severe pain at a fixed site of the head and hemiplegia, which was more like the syndrome of hemiplegia (episodic) or cerebral vasospasm, but the cranial MRA and MRV had normal findings. Brain MRI showed hyperintensity of the right central sulcus and the temporal parietal lobe in the T2 flair phase, which fully matched the site of her headache and left hemiplegia. It is interesting that the symptoms completely disappeared after immunotherapy, suggesting that atypical anti-NMDAR encephalitis can be easily misdiagnosed as other diseases. The patient presented with syncope but the head-up tilt test (HTT) was not refined. It may be possible that syncope would be the primary manifestation in cardiovascular medicine, so the HTT trial remains refined to exclude vagal excited vascular syncope. The long-range EEG showed abnormal activities, consistent with the EEG findings of autoimmune encephalitis, suggesting that the long-range EEG examination is beneficial for diagnosing atypical anti-NMDAR encephalitis.
Previous reports showed that brain atrophy caused by anti-NMDAR encephalitis is fully reversible and patients can fully recover from the disease [10]. However, the behavioral cognitive changes and psychological disorders [11, 12] often receive less attention from clinicians. As in the case of this patient, the mere treatment of collision injury such as headache from a fall after syncope would delay the correct diagnosis and worsen the condition. Timely refinement of additional examinations is highly recommended for timely diagnosis of anti-NMDAR encephalitis and improvement of discharge after a short-term immunotherapy.
Conclusions
This case provides us with new insights into the clinical presentation of anti-NMDAR encephalitis and facilitates early detection and treatment of patients with atypical anti-NMDAR encephalitis.
Availability of data and materials
Supporting data are available upon request.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- DWI:
-
Diffusion-weighted imaging
- EEG :
-
Electroencephalogram
- HTT:
-
Head-up tilt test
- NMDAR:
-
N-methyl-D aspartate receptors
- MRA:
-
Magnetic resonance angiography
- MRI:
-
Magnetic resonance imaging
- MRV:
-
Magnetic resonance venography
References
Neurology Branch of the Chinese Medical Association. Expert consensus on the diagnosis and treatment of autoimmune encephalitis in China. Chin J Neurol. 2017;50:91–8.
Schmitt SE, Pargeon K, Frechette ES, Hirsch LJ, Dalmau J, Friedman D. Extreme delta brush: a unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology. 2012;79(11):1094–100.
Mohammad SS, Soe SM, Pillai SC, Nosadini M, Barnes EH, Gill D, et al. Etiological associations and outcome predictors of acute electroencephalography in childhood encephalitis. Clin Neurophysiol. 2016;127(10):3217–24.
Li X, Hou C, Wu WL, Liang H, Zheng K, Zhang Y, et al. Pediatric anti-N-methyl-d-aspartate receptor encephalitis in southern China: analysis of 111 cases. J Neuroimmunol. 2021;352:577479.
Liu X, Yan B, Wang R, Li C, Chen C, Zhou D, et al. Seizure outcomes in patients with anti-NMDAR encephalitis: a follow-up study. Epilepsia. 2017;58(12):2104–11.
Granata T, Matricardi S, Ragona F, Freri E, Zibordi F, Andreetta F, et al. Pediatric NMDAR encephalitis: a single center observation study with a closer look at movement disorders. Eur J Paediatr Neurol. 2018;22(2):301–7.
Desena AD, Greenberg BM, Graves D. Three phenotypes of anti-N-methyl-D-aspartate receptor antibody encephalitis in children: prevalence of symptoms and prognosis. Pediatr Neurol. 2014;51(4):542–9.
Planagumà J, Leypoldt F, Mannara F, Gutiérrez-Cuesta J, Martín-García E, Aguilar E, et al. Human N-methyl D-aspartate receptor antibodies alter memory and behaviour in mice. Brain. 2015;138(Pt 1):94–109.
Hughes EG, Peng X, Gleichman AJ, Lai M, Zhou L, Tsou R, et al. Cellular and synapic mechanisms of anti-NMDA receptor encephalitis. J Neurol Sci. 2010;30(17):5866–75.
Iizuka T, Yoshii S, Kan S, Hamada J, Dalmau J, Sakai F, et al. Reversible brain atrophy in anti-NMDA receptor encephalitis: a long-term observational study. J Neurol. 2010;257(10):1686–91.
Matricardi S, Patrini M, Freri E, Ragona F, Zibordi F, Andreetta F, et al. Cognitive and neuropsychological evolution in children with anti-NMDAR encephalitis. J Neurol. 2016;263(4):765–71.
de Bruijn MAAM, Aarsen FK, van Oosterhout MP, van der Knoop MM, Catsman-Berrevoets CE, Schreurs MWJ, et al. Long-term neuropsychological outcome following pediatric anti-NMDAR encephalitis. Neurology. 2018;90(22):e1997–2005.
Acknowledgements
We thank the patient and her family for allowing us to share her details.
Funding
This study was funded by Sanming Project of Medicine in Shenzhen (SZSM201812005).
Author information
Authors and Affiliations
Contributions
JH designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. CZ, XZ, YF, HZ and DC designed the data collection instruments, collected the data, and reviewed and revised the manuscript. JL designed the study, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Shenzhen Children Hospital Ethics Committee (Ethics Approval No. 2021002). Written informed consent was given by the patient’s parents.
Consent for publication
The written informed consent for publication was obtained from the patient’s parents.
Competing interests
The authors declare that they have no conflict of interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hu, J., Zhao, C., Zhao, X. et al. Anti-NMDAR encephalitis with seizure-like activity and hemiplegia - a case report and literature review. Acta Epileptologica 4, 30 (2022). https://doi.org/10.1186/s42494-022-00100-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42494-022-00100-5