Abstract
Background
Sudden unexpected death of epilepsy (SUDEP) is a severe outcome of epilepsy. This study aimed to report the clinical and pathological findings in patients with SUDEP.
Methods
The record of patients with sudden death was screened. When the reason of death matched with the definition of SUDEP, the clinical and pathological data were analyzed. Eleven patients with SUDEP were included in the study.
Results
Eight patients died after a generalized tonic-clonic seizure, seizures were induced by emotional changes in five patients, four cases were found dead in bed. Carbamazepine was prescribed in six patients. The autopsy showed brain edema and pulmonary edema in all eleven patients. Loss of neurons and gliosis were presented in some brains of SUDEP subjects. The main pathological changes in SUDEP include brain edema, pulmonary edema, loss of neurons and gliosis.
Conclusions
Risk factors for SUDEP in the study are generalized tonic-clonic seizure, emotional disturbance and carbamazepine treatment.
Similar content being viewed by others
Introduction
Sudden unexpected death of epilepsy (SUDEP) was defined as “sudden unexpected witnessed or unwitnessed, non-traumatic and non-drowning death in a patient with epilepsy, with or without evidence for a seizure and excluding documented status epilepticus where necropsy examination does not reveal a toxicological or an anatomical cause for death” [1]. SUDEP is a common cause of death in patients with epilepsy. The incidence of SUDEP ranges from 0.09 to 9.3 per 1000 person-years depending on variant study design and epilepsy population under study [2]. Epidemiological studies indicate that the incidence of SUDEP in adult is higher than in children and it increases with the duration and severity of epilepsy [3, 4]. Without or the lack of therapeutic levels of antiepileptic drugs(AEDs), frequent changes in regimens, and multiple episodes of epilepsy, especially tonic-clonic seizures, are considered risk factors for SUDEP [3,4,5].
While many clinical and animal experimental studies have examined the pathophysiological mechanisms underlying SUDEP, the precise mechanisms have not been elucidated, and it is still difficult for clinicians to conduct appropriate therapeutic interventions to prevent the physiological changes that complicate seizures and lead to SUDEP [6]. These difficulties are in part attributed to the complexities of the mechanisms of SUDEP, the lack of an ideal animal model, and the patients’ rapidly progression to death without providing clinicians sufficient time to acquire complete information [7]. However, another important explanation for these difficulties is the shortage of detailed histopathological examination of patients died of SUDEP, which could provide clinicians not only a better understanding of the mechanisms of SUDEP but also a reference for evaluating the risk of sudden death and conducting accurate interventions [7, 8], Moreover, a neuropathological examination and risk factors assessment are necessary for a potential patient of SUDEP to confirm the diagnosis. Here, we reported pathological data and risk factors of eleven patients with SUDEP in Southwest China.
Methods
The people with sudden death were screened from department of Forensic Medicine(also known as Chongqing Institute of Forensic Medicine), Chongqing Medical University which is an authoritative inspection institution for autopsy dissection and settling the medical disputes designated by Chongqing Municipal Government from 1996 to 2016. We have diagnosed these patients with SUDEP according to the definition for SUDEP. Sudden unexpected death in epilepsy (SUDEP): Sudden, unexpected, witnessed or unwitnessed, non-traumatic, and non-drowning death that occurs in benign circumstances in an individual with epilepsy, with or without evidence for a seizure, and excludes documented status epilepticus, in which post-mortem examination does not reveal a cause of death [9]. Briefly, SUDEP is commonly defined as sudden death in a patient diagnosed with epilepsy, in which status epilepticus, trauma, or drowning were excluded, and there are no other possible causes of death. All the eleven patients have met the criteria of SUDEP. The autopsy reports were obtained and the diagnosis of SUDEP were confirmed. Meanwhile, the recruitment of study subjects and data collection have been completed by searching the autopsy reports in the department of Forensic Medicine.
The autopsy was carried out according to the forensic procedures [10].
These important organs, including brain, heart, lung, liver, kidney, ect, were cut into paraffin sections which were stained by hematoxylin-eosin (HE) staining to assess the histopathological characteristics.
Clinical information was collected if possible, included age, gender, seizure type and frequency, family history of epilepsy, CT scan of brain, EEG results and Anti-epileptic Drugs. The study have been performed in accordance with the Declaration of Helsinki and the committee on human research at Chongqing Medical University has approved the study. Informed consents were obtained from family members of all patients.
Results
Clinical features of patients
Eleven patients with SUDEP were included in this study. The clinical features were listed in Table 1. Eight patients were considered as idiopathic epilepsy, one patient was diagnosed symptomatic epilepsy followed by head trauma. All patients died without evidence of seizures and epileptic status. Among them, six cases died in bed during sleep, five patients in our study suddenly died during trepidation or after quarreling with others. The antiepileptic drugs (AEDs) that the patients have taken are listed in Table 1, carbamazepine was prescribed in five patients. Other two cases, who used to accept AEDs polytherapy, had stopped AEDs by themselves half or 1 year before death. Electrocardiogram examination was normal in periodic follow-up in all eleven patients. The serum concentration of AED(s) was not tested due to practical reason. The postmortem examination was performed 6 h to 24 h after death.
Autopsy findings of patients
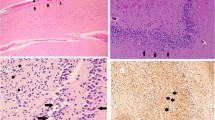
The postmortem examination showed brain edema in all patients (Fig. 1). Four patients showed brain edema with gliosis (Fig. 1a-b), the majority of our series presented perivascular oligodendroglia, oligodendroglial clusters around some neurons and remarkable cerebellar Bergmann’s gliosis. Three patients showed brain edema with loss of neurons (Fig. 1c-d). Pulmonary edema was detected in all patients, including a large number of infiltrates in pulmonary alveoli and pulmonary interstitial edema (Fig. 2a-b), pulmonary interstitial edema and fibrosis with remarkable inflammatory cell infiltration (Fig. 2c). In addition, a low-grade swelling myocardial cells with orderly arrangement was found in case 1, 2, 3 (Fig. 3a). The structure of hepatic lobules was disarranged with low-grade hepatic fibrosis in case 4 (Fig. 3b). And immersion of inflammatory cells in kidneys was also found at autopsy in case 4 (Fig. 3c). The details of pathological findings were listed in Table 2.
The pathological changes of the brains in the patients with SUDEP: the brain edema, gliosis and loss of neurons in the brains. a There are brain edema and gliosis in HE staining (magnification: × 200). b There are brain edema and gliosis brain edema and gliosis in HE staining (magnification: × 400). c There are brain edema and loss of neurons in HE staining (magnification: × 200). d There are brain edema and loss of neurons in HE staining (magnification: × 400)
The pathological changes of the lungs of the patients with SUDEP: the pulmonary edema, much fluid in pulmonary alveoli and interstitial fibrosis in the lungs. a There are pulmonary edema in HE staining (magnification: × 200). b There are much fluid in pulmonary alveoli in HE staining (magnification: × 200). c There are pulmonary interstitial fibrosis in HE staining (magnification: × 200)
The pathological findings in other organs of the patients with SUDEP. a There are myocardial cell swelling in HE staining of heart (magnification: × 200). bThere are disarrangement of hepatic lobules in HE staining of liver (magnification× 200). c There are inflammatory cell infiltration in HE staining of kidneys (magnification: × 200)
Discussion
There are lots of sudden unexplained death in patients with epilepsy in clinical practice, and no evidence of epileptic seizures before death presents in some patients. So far, the argument on the relationship between epilepsy and sudden death continue until now. A study of 22 cases of SUDEP revealed that both hot shock protein and immediate early gene increased significantly in the SUDEP group, while remained normal in the non-epileptic group or sudden cardiac death group [11]. These results have implied that epileptic patients had cerebral dysfunction even before sudden death, and the dysfunction becomes a pathological basis of SUDEP. The investigation of death cases (including epileptic sudden death cases) showed that the sudden unexpected death in patients with epilepsy was 3.5 to 8 times than that in normal control group [12, 13], suggesting that SUDEP is associated with epilepsy. Because the cause of SUDEP still remains unclear, the pathological examination is necessary for the patients to reveal the enigma. Furthermore, the risk factors would be analyzed to discover the etiology of SUDEP.
Pathological characteristics of SUDEP
Cerebral pathology
The brain sections of our eleven cases showed significant brain edema with unknown reasons. CT scan of brain has shown that epileptic seizure may lead to brain edema, and brain edema may last for weeks to months [14]. However, another study showed only two of 107 SUDEP cases had seizures several hours before death [15], which did not support the hypothesis that epileptic seizure caused brain edema. In our study, death occurred after a seizure in eight patients; therefore, brain edema in pathological examination might be induced by epileptic seizure. However, brain edema caused by the metabolism termination after death cannot be excluded in the present study. All cases in our study presented brain edema, but no case showed brain hernia, significant displacement of brain or status epileptic caused by brain edema. Therefore, brain edema is not considered as a cause of SUDEP.
Loss of neurons was found in three cases. The exact incidence of neuronal loss and its relationship to SUDEP are unknown. Our previous study has found that neuron specific enolase, a neuronal marker, significantly increases after seizure activity, which suggests that epileptic seizures contribute to neuronal necrosis [14]. Seizures occurred before death in patients with neuronal loss, we then postulate that neuronal loss in SUDEP is associated with seizure. Researches of SUDEP animal models have revealed that dysfunction of neurons may result to lethal cardiac arrhythmia and central apnea. Therefore, loss of neuron becomes one cause of sudden epileptic death. However, seven cases in our study showed no neuronal loss; thus, other reasons could contribute to SUDEP besides neuronal loss.
Gliosis is common in SUDEP patients. Our results presented perivascular oligodendroglia, oligodendroglial clusters and Bergmann’s gliosis. However, gliosis has been also observed in the surgical specimens of non-SUDEP; therefore, gliosis is not be a cause of SUDEP.
Pulmonary pathology
Pulmonary congestion and edema, which is common in SUDEP, are the strong evidence of SUDEP. All cases in our study have presented pulmonary edema, enlarged pulmonary interstitial and alveolar hydrops on microscopic examination. It is believed that the underlying mechanism for pulmonary edema is due to the dysfunction of the central nervous system [16]. This neurogenic pulmonary edema is regarded as a possible cause of SUDEP. However, the metabolism stopping after death can also cause pulmonary edema. Therefore, we cannot draw a conclusion that pulmonary edema is a specific pathological change of SUDEP.
The pulmonary fibrosis with moderate inflammatory cell infiltration in one case show possible chronic pulmonary infection. However, the patient had no respiratory failure before death, and no severe hypoxia features after death. Then, his sudden death could not be a result of the pulmonary problem. Moreover, no similar pulmonary pathological changes were found in other SUDEP patient, thus we think the pulmonary changes might co-exist with SUDEP in this individual.
Cardiac pathology
Fatal arrhythmia is another possible cause of sudden death [17, 18]. No significant morphologic abnormality of the hearts were found in eleven patients with SUDEP. The result have suggested that the cardiac morphologic changes could not be the cause of SUDEP in the present study. Lack of the record of the electrocardiogram at the time of death, we cannot corfirm whether or not the SUDEP subjects developed fatal cardiac arrhythmia before death. But all electrocardiogram examinations were normal in follow-up before death. Therefore, it is less possible that the cardiac dysfunction induces SUDEP in our group.
Others
One case showed dearrangement of the nephric cell with immersion of inflammatory cells, suggesting possible chronic nephritis, whereas, it was not a cause of SUDEP. Of eleven cases, the hepatic configuration was normal in ten, slightly bigger than expected in one. Although two cases presented hepatic blood sinuses dilation and congestion with disorderedly arranged hepatic lobules and inflammatory cell infiltration, the hepatic changes could not explain SUDEP.
Risk factors of SUDEP
The most effective way of SUDEP prevention is to investigate risk factors. Recent study has shown that SUDEP associated factors included poor seizure control, in particular generalized tonic-clonic seizures (GTCS), absence of treatment with AEDs, polytherapy with AEDs, onset of epilepsy at a young age, long duration of epilepsy, male sex [1]. Risk factor identification can assist doctors in educating patients and family members about SUDEP, and to take some measures to reduce risk. After analyzing the clinical data in our cohort, several possible risk factors are discussed.
Sleep asphyxia
In an eleven-year investigation of sudden death of patients with epilepsy, 69% of SUDEP has died in sleep [19], another report indicates the great majority of 103 SUDEP patients in their study has died in bed [20]. In our group, four cases of eleven have also died in sleep with a prone position. Given the association between SUDEP and prone position, we can hypothesize that these cases of SUDEP may have been due to airway obstruction. The prone position may be dangerous if epilepsy patients remain immobile despite hypoxemia during the postictal period. These studies have showed that SUDEP is prone to occur at night, so the asphyxia during postictal confusion might be a possible risk factor of SUDEP.
Trepidation and emotional disturbance
It is supported in clinics that trepidation and emotional disturbance can induce epileptic seizures. Five SUDEP cases in our study have suddenly died during trepidation or after quarreling with others. The results suggest that trepidation and emotional disturbance are probably the risk factors for SUDEP. Therefore, it may reduce SUDEP by reminding the patients and their relatives to control their mood.
Antiepileptic drugs (AEDs)
Although the relationship of AEDs with SUDEP is still controversial, sub-therapeutic level of AEDs and polytherapy with more than two AEDs have been considered to be risk factors for SUDEP [21]. Phenytoin, valproate, carbamazepine, gabapentin, lamotrigine and tiagabin were rarely associated with SUDEP [18]. It is reported that the fluctuation of serum levels of carbamazepine leads to cardiac arrhythmias and vegetable neural dysfunction, which then contribute to the sudden death in epileptic patients [18]. Six cases in our study took carbamazepine, one took carbamazepine and valproate combined, this suggests that carbamazepine is possibly related to SUDEP. It is regretful that the serum levels of AED(s) had not been tested due to practical reasons; however, the overdose of AED(s) cannot explain sudden death because no AED(s) dosage was altered recently or no clinical manifestation of AEDs toxicity was presented before death. In addition, irregular AED(s) treatment is a possible risk factor for SUDEP because AEDs were terminated in two patients.
Pattern and frequency of seizure
In general, GTCS is associated with SUDEP, and at least 90% of SUDEP patients had a history of primary or secondary generalized tonic-clonic seizure [22]. 90% of these patients with GTCS or GTCS component demonstrate that SUDEP occurred easily in GTCS epilepsy. It is reported that frequent GTCS increased the risk of SUDEP [23]. However, at least 50% of patients in our study showed infrequent seizures (< 2 seizures per year), thus, our results do not support that SUDEP is a seizure-associated event.
Conclusion
The underlying pathophysiologic mechanisms of SUDEP are still remain unclear. Our studies have shown that SUDEP is a heterogeneous condition in terms of both the underlying epilepsy neuropathology, risk factors as well as mechanism of death. In the future, neurologists, neuropathologists, medical examiners, and coroners will collaborate together to improve our understanding of the mechanisms of SUDEP. Continued education, research, and the development of new interventions are needed to further implement effective prevention of SUDEP.
Availability of data and materials
All data generated or analyzed in this study are included in this manuscript and its additional files.
Abbreviations
- AEDs:
-
Antiepileptic drugs
- CBZ:
-
Carbamazepine
- GTCS:
-
Generalized tonic-clonic seizures
- PHT:
-
Phenytoin
- SUDEP:
-
Sudden unexpected death of epilepsy
- VPA:
-
Valproate
References
Nashef L. Sudden unexpected death in epilepsy: terminology and definitions. Epilepsia. 1997;38(suppl. 11):6–8.
Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current knowledge and future directions. Lancet Neurol. 2008;7:1021–31.
Devinsky O. Sudden, unexpected death in Epilepsy. N Engl J Med. 2011;365:1801–11.
Sillanpää M, Shinnar S. Long-term mortality in childhood-onset epilepsy. N Engl J Med. 2010;363:2522–9.
Langan Y, Nashef L, Sander JW. Casecontrol study of SUDEP. Neurology. 2005;64:1131–3.
Friedman D, Donner EJ, Stephens D, Wright C, Devinsky O. Sudden unexpected death in epilepsy: knowledge and experience among U.S. and Canadian neurologists. Epilepsy Behav. 2014;35:13–8.
Pansani AP, Colugnati DB, Scorza CA, de Almeida AC, Cavalheiro EA, Scorza FA. Furthering our understanding of SUDEP: the role of animal models. Expert Rev Neurother. 2016;16:561–72.
Swinghamer J, Devinsky O, Friedman D. Can post-ictal intervention prevent sudden unexpected death in epilepsy? A report of two cases. Epilepsy Behav. 2012;24:377–9.
Devinsky O, Hesdorffer DC, Thurman DJ, et al. Sudden unexpected death in epilepsy: epidemiology, mechanisms, and prevention. Lancet Neurol. 2016;15(10):1075–88.
Bucholtz A. Death investigation: an introduction to forensic pathology for the nonscientist. Waltham: Elsevier; 2015.
Thom M, Seetah S, Sisodiya S, et al. Sudden and unexpected death in epilepsy (SUDEP): evidence of acute neuronal injury using HSP70 and c-Jun immunohistochemistry. Neurepathol Appl Neurobio1. 2003;29:132–43.
Camfield CS, Camfield PR, Veugelem PJ. Death in children with epilepsy: a population-based study. Lancet. 2002;359:1891–5.
Langan Y, Nashef L, Sander JW. Certification of deaths attributable to epilepsy. J Neurol Neuresurg Psychiatry. 2002;73:751–2.
Myers KA, McMahon JM, Mandelstam SA, et al. Fatal cerebral edema with status epilepticus in children with Dravet syndrome: report of 5 cases. Pediatrics. 2017;139(4). https://doi.org/10.1542/peds.2016-1933
Morentin B, Alcaraz R. Sudden unexpected death in epilepsy in children and adolescents. Rev Neurol. 2002;34(5):462–5.
So EL. What is known about the mechanisms underlying SUDEP? Epilepsia. 2008;49(Suppl 9):93–8.
Donner EJ, Waddell B, Osland K, et al. After sudden unexpected death in epilepsy: lessons learned and the road forward. Epilepsia. 2016;57(Suppl 1):46–53.
Aurlien D, Gjerstad L, Taubøll E. The role of antiepileptic drugs in sudden unexpected death in epilepsy. Seizure. 2016;43:56–60.
Ali A, Wu S, Issa NP, Rose S, et al. Association of sleep with sudden unexpected death in epilepsy. Epilepsy Behav. 2017;76:1–6.
Mostacci B, Bisulli F, Vignatelli L, et al. Incidence of sudden unexpected death in nocturnal frontal lobe epilepsy: a cohort study. Sleep Med. 2015;16(2):232–6.
Hesdorffer DC, Tomson T. Sudden unexpected death in epilepsy. Potential role of antiepileptic drugs. CNS Drugs. 2013;27(2):113–9.
Epilepsy BE. Risk factors for sudden unexpected death in epilepsy-combined analysis from case-control studies. Nat Rev Neurol. 2011;7(4):188.
Hesdorffer DC, Tomson T, Benn E, et al. Combined analysis of risk factors for SUDEP. Epilepsia. 2011;52(6):1150–9.
Acknowledgements
We would like to thank the family members of all patients who participated in this study.
Funding
This work was supported by grants from the National Natural Science Foundation of China (81671286, 81871019), Key-project of Social undertakings and people’s livelihood security of Chongqing Science & Technology Commission (cstc2017shms-zdyfX0009), Scientific Research Project of Chongqing Municipal Education Commission (KJ1702011).
Author information
Authors and Affiliations
Contributions
WY performed research and was a major contributor in writing the manuscript. YZ, QL performed research and participated in writing the manuscript. XT, PZ analyzed data. Professor YL designed research and revised the manuscript. All authors read and approved the final manuscript.
Authors’ information
All the authors come from Chongqing Medical University, which is one of the largest epilepsy centers in China totally. Our team has engaged in epilepsy research for more than 10 years and has published dozens of English papers which cover the pathogenesis of seizure, the treatment of epilepsy et al.!
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The experiments have been performed in accordance with the Declaration of Helsinki and the ethical committee on human research at Chongqing Medical University has approved the study. Informed consents were obtained from family members of all patients.
Consent for publication
The family members of all patients have consent for publication.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yu, W., Zhu, Y., Li, Q. et al. A clinical and pathological study in patients with sudden unexpected death in Epilepsy. Acta Epileptologica 1, 7 (2019). https://doi.org/10.1186/s42494-019-0007-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42494-019-0007-5