Abstract
Background
Approximately half of patients with spontaneous intracerebral hemorrhage (ICH) die within 1 year. Prognostication in this context is of great importance, to guide goals of care discussions, clinical decision-making, and risk stratification. However, available prognostic scores are hardly used in clinical practice. The purpose of this review article is to identify existing outcome prediction scores for spontaneous intracerebral hemorrhage (ICH) discuss their shortcomings, and to suggest how to create and validate more useful scores.
Main text
Through a literature review this article identifies existing ICH outcome prediction models. Using the Essen-ICH-score as an example, we demonstrate a complete score validation including discrimination, calibration and net benefit calculations. Score performance is illustrated in the Erlangen UKER-ICH-cohort (NCT03183167). We identified 19 prediction scores, half of which used mortality as endpoint, the remainder used disability, typically the dichotomized modified Rankin score assessed at variable time points after the index ICH. Complete score validation by our criteria was only available for the max-ICH score. Our validation of the Essen-ICH-score regarding prediction of unfavorable outcome showed good discrimination (area under the curve 0.87), fair calibration (calibration intercept 1.0, slope 0.84), and an overall net benefit of using the score as a decision tool. We discuss methodological pitfalls of prediction scores, e.g. the withdrawal of care (WOC) bias, physiological predictor variables that are often neglected by authors of clinical scores, and incomplete score validation. Future scores need to integrate new predictor variables, patient-reported outcome measures, and reduce the WOC bias. Validation needs to be standardized and thorough. Lastly, we discuss the integration of current ICH scoring systems in clinical practice with the awareness of their shortcomings.
Conclusion
Presently available prognostic scores for ICH do not fulfill essential quality standards. Novel prognostic scores need to be developed to inform the design of research studies and improve clinical care in patients with ICH.
Similar content being viewed by others
Background
Among all deaths caused by neurological disease worldwide two thirds are related to stroke [1]. Spontaneous intracerebral hemorrhage (ICH), the most lethal stroke subtype, has shown a remarkable increase in incidence over the past decades to currently approximately 176 cases per 100,000 person-years [2]. Although ICH accounts for only 10–15% of stroke cases it is associated with about 70% of 1-month stroke mortality. Approximately half of patients with ICH die within the first year [3]. Because of the high likelihood of unfavorable outcome after ICH, clinicians are often forced to develop a clinical strategy that is determined by both medical and ethical considerations.
Prognostic models may guide health care providers and families when they are confronted with these complex decisions. However, recent outcome research suggests that current clinical scores, typically designed to estimate the risk of mortality or disability, are neither accurate, nor are they predicting those endpoints that matter to patients and families [4]. The discrepancy between what prognostic scores offer and what is needed in clinical practice has led physicians to increasingly neglect these scores. This trend is fueled by research showing that subjective clinical judgment may be superior to prediction model estimates [5,6,7].
Here we will review current ICH prognostication tools and point out their shortcomings. The unused potential of new predictor variables and a growing movement towards patient reported outcome measures (PROMs) highlight the need for novel ICH prediction scores. We delineate concepts on how to create and validate new scores, and how to manage and reduce major biases. Lastly, we discuss how currently available scores, despite their shortcomings, can facilitate meaningful prognostication and informed decision-making in clinical practice.
Main text
Methods
Literature search
We conducted a literature review searching pubmed up to December 31, 2020. Studies were selected according to the CHARMS checklist [8]. We included studies in humans reporting prognostic scores regardless of type or timing of predicted endpoints. The search algorithm and detailed inclusion and exclusion criteria are reported in the online supplement.
Complexity of prediction scores
To quantify the ease of use of current scores, we assigned an availability factor to each score component with greater numbers indicating more difficult to obtain data (lower availability). Easily accessible clinical information, e.g., the patient’s age, Glasgow Coma Scale (GCS), serum glucose, or ICH location, was assigned a value of 1. Complex imaging information requiring the use of a software or additional radiological knowledge, e.g., ICH or IVH volume, was assigned a value of 2. Past medical history information was assigned a value of 3. Imaging or physiological scores integrated into a prediction score as one variable, e.g., the APACHE score, were assigned a value of 4. The sum of the weighting factors was then plotted for each prediction score.
Examples score validation
To illustrate the steps of a complete score validation, we calculated and validated the Essen-ICH-score in the UKER ICH-cohort (n = 1166). We chose the Essen-score because its original publication was the only score that reported absolute and relative outcome risks [9]. Characteristics of the UKER ICH-cohort have been described previously and are available online at clinicaltrials.gov (NCT03183167) [10]. The Essen-score is designed to predict favorable functional outcomes, as defined by Barthel index > 95. Because the Barthel index was not available in the Erlangen cohort, we assessed the performance of the Essen-score with regards to prediction of favorable functional outcome, defined as modified Rankin score (mRS) 0–3, at 90 days, and survival at 90 days (mRS 0–5).
Standard protocol approvals, and patient consents
The UKER ICH-cohort study was approved by the ethics committees and institutional review boards based on the vote from Friedrich-Alexander-University Erlangen-Nuremberg, Germany. Consent was obtained by patients or legal representatives.
Results
Literature review
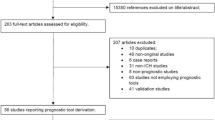
The search returned 4867 pubmed hits, 3825 of which were studies conducted in humans. Title and abstract of these 3825 references were screened, and 3792 papers were excluded after the first screening. The remaining 33 referenced papers were read in full. Among these, 19 studies met inclusion criteria (Table 1). Specific reasons for excluding the other 14 studies are reported in the online data supplement. An inclusion/exclusion flow chart is available in the online Supplement (eFigure 1 in the online supplement).
Scores and score complexities
All available prognostic scores identified in our literature search contain mortality and/or functional disability as predicted outcome, although the timing of outcome assessment varies substantially (Table 1). More than half of the scoring systems were intended to predict mortality in-hospital or 30 days after the index ICH. In the remainder, the endpoint is functional outcome, invariably dichotomized, at varying times after the ICH, quantified by one or a combination of the following three grading scales: mRS, the Glasgow outcome scale, or the Barthel index (more information available in the online supplement). Figure 1 provides a conceptual illustration of prognostic score complexities for the currently available ICH scores.
Validation of the Essen-ICH-score
With the exception of the max-ICH score, which was fully validated recently, none of the scores identified in our literature search provided complete score validation [29]. Here we chose the Essen-ICH-score to illustrate the three methodological pillars of validation discrimination, calibration, and net benefit analysis. We validated the Essen-score in the Erlangen UKER ICH cohort (Fig. 2) [9, 10].
Three validation measures. Discrimination (panel a + b), calibration (panel c + d) and net benefit analysis (panel e + f) are shown for the outcomes mRS score 0–3 (left column), and mRS score 0–5 (=survival, right column). Panels c + d: the dotted indicates the ideal ratio where expected and observed outcomes are identical. The red line indicates the actually observed ratios. Panels e + f: the red line indicated the net benefit when using the Essen ICH score on the full range of threshold probabilities, the curved dotted line indicates the net benefit of treating all patients, and the straight dotted line on the x-axis indicated the net benefit of treating no one. Panel e shows an overall benefit (mRS 0–3) while panel f (mRS 0–5) does not indicate a clear benefit (red line mostly lower than the curved dotted line). Abbreviations: mRS modified Rankin scale, E:O expected/observed ratio, AUC area under the receiver-operating characteristic curve
Discrimination
The first step of score validation is to understand discriminatory performance, which can be graphically represented by the area under the receiver operator characteristic curve (AUC), and statistically expressed by the concordance statistic (c-statistic). The c-statistic is a measure of the chance that a randomly selected patient with unfavorable outcome had a higher prediction score grade than a patient with favorable outcome. In our example (Fig. 2) the AUC for mRS 0–3 can be considered to be good (0.87, 95% confidence interval, CI, 0.85–0.90). Even though not developed for this endpoint the Essen ICH score’s discriminatory properties regarding survival (mRS 0–5) are good as well (AUC 0.85, CI 0.83–0.87).
Calibration
Calibration quantifies the absolute risk of having a certain outcome. Calibration is a necessary addition to discrimination. Absolute risks are illustrated by a calibration curve, where the expected risk (x-axis) needs to be in line with the observed risk (y-axis) for calibration to be perfect. In our example the calibration curve for mRS 0–3 shows that the observed risks of favorable outcomes are greater than what is predicted by the model. The importance of score calibration becomes clear when calibration is plotted for survival as outcome. Because survival is a very broadly defined outcome, it is not surprising that the calibration plots show a strong underestimation of the absolute risks of outcome, despite good discrimination (Fig. 2).
Net benefit
The two previous steps have the goal to identify patients who will develop unfavorable outcome and to provide a risk estimate for that. In recent years, a third element has been added that combines discrimination and calibration in a graphical representation, the so-called net clinical benefit curve [30]. There are three main elements of net benefit plots: the net benefit when using the prediction score on the full range of score grades, which is then compared to the net benefit of treating all patients on the one hand (without using a prediction score), and the net benefit of treating no one on the other hand (again without using a prediction score). Our analysis indicates a net benefit from using the Essen ICH score for the prediction endpoint mRS 0–3, but not for the endpoint mRS 0–5 (Fig. 2).
Discussion
Published in 2018 and including a systematic literature review up to September 2016, a meta-analysis by Gregorio et al. provided a thorough overview on all ICH outcome prediction scores that were available at the time [31]. Interestingly, the authors attempted a direct comparison between machine-learning and conventional regression-based prognostication tools coming to the conclusion that regression-based scores were overall superior. However, scores were mainly judged on their ability to discriminate between dichotomized endpoints (favorable versus unfavorable mRS categories, or alive versus dead), and conceptual problems like the withdrawal of care (WOC) bias or negligence of patient-reported outcomes were not addressed in-depth. In the following discussion our goal was to include those issues that affect prognostic tools at the level of score design and validation.
Clinical use of currently available scores
The ICH score is probably the most broadly known prognostication tool as it was one of the first available scores and has been extensively studied for different predicted time points [15, 32]. However, there is little data to quantify the actual use of prediction scores in clinical practice. A 2012 survey in 77 German neurointensive care units showed that only 10% of neurologists, 8% of neurosurgeons and none of the surveyed anesthesiologists routinely use the ICH score. Theoretically, the use of the ICH score might be more established in the United States. However, in the same German paper more than 80% of study participants stated to routinely use the GCS and the Hunt&Hess grading scales for subarachnoid hemorrhage. Both scores are frequently used in the United States, indicating that the near neglect of the ICH score among German study participants cannot simply be ascribed to an intercontinental difference in medical culture [5]. Barriers to using clinical scores may include lack of trust in the prognostication instrument or that score calculation may be too time-consuming.
Problems of current prognostic scores
Prior studies have questioned the clinical utility of ICH prediction scores altogether. In a head-to-head comparison with the GCS scale, the original ICH score and the ICH Grading Scale did not show a net clinical benefit regarding prediction of 30-day mortality [33]. One study in five US American tertiary care centers prospectively compared the accuracy of 3-months outcome predictions between clinicians on the one hand and the ICH and FUNC scores – two of the most frequently used prediction scores – on the other. In this study attending clinician judgment was superior to score predictions [6]. A possible interpretation of these study results is that the human mind integrates more information in its decision-making process than the comparatively simple information contained in the ICH and FUNC scores. For example, both ICH and FUNC score are lacking information on comorbidities, general appearance of the patient, information on code status etc.
The withdrawal of care bias
Another caveat of score-based predictions is the self-fulfilling prophecy bias [7, 33,34,35]. This bias, also called WOC bias, arises when the decision to withdraw care is based on the prediction that the patient’s outcome will likely be poor. If the WOC decision is based on data provided by a prediction model, the association between predicted and true outcome and thus the performance of the model is artificially strengthened. This in turn may strengthen the model’s influence on clinical decision-making (Fig. 3) [36].
The magnitude of the WOC bias and its effect on a prediction model are difficult to determine. This is because the decision to withdraw care can theoretically go against a model prediction and thus weaken rather than strengthen the performance of the model, for example if care is withdrawn in patients in whom the model predicts a favorable outcome. Furthermore, clinical anticipation of unfavorable outcome may in fact be a correct prediction of the disease course in which case there is no WOC bias [37].
Studies have shown that these considerations are not purely theoretical but that they impact clinical behavior and confound prediction models [38, 39].
The max-ICH score was the first ICH prediction score in which the WOC bias was addressed at the level of score creation. Max-ICH was developed in maximally treated patients excluding those with early care limitations. In the 583 patients included in the study conventional prognostication overestimated the observed mortality by 45% and overestimated the observed unfavorable outcome by 10% [27]. The max-ICH score is the only score that we are aware of that has been fully validated according to the criteria laid out in this review [29].
Whenever prognostic information is being made available to a physician who makes care decisions the WOC bias may continue to exert its influence, even after clinical implementation of a prediction model. Therefore, studying the impact of a prognostic model is difficult. Cluster-randomized controlled trials, comparing treatment outcomes in some centers that use a prediction model with outcomes in other centers that do not use the prediction model, are preferable over classic randomized controlled trials. This is because - by design - cluster randomized trials separate both patients and physicians into the two arms and thus reduce the WOC bias that originates from physicians [40].
The bias originating from the WOC practice is reflected in clinical care guidelines. It is recommended to refrain from early care limitations for at least the first two full days of hospitalization. This recommendation does not apply to patients who have a documented do-not-resuscitate or do-not-intubate or other care limiting orders [41, 42].
Simplicity, accuracy, and timing of score assessment
It seems counterintuitive that one prognostic score would meet the goals of both simplicity and prediction accuracy. However, these principles have guided the development of most ICH prediction scores to date. With more advanced technology such as smartphone apps, nowadays even complex prediction models can be easily implemented in clinical practice [43, 44]. However, to date, no smartphone app calculators are available for ICH prediction scores.
The timing of score assessment for most ICH scores is upon admission or briefly after, thereby accommodating the clinical necessity of early prognostication to inform early treatment decisions. Repeat score calculation 5 days into the hospital stay and score calculation using follow up imaging rather than admission imaging has been shown to improve prediction accuracy [45, 46]. In subarachnoid hemorrhage unfavorable long-term outcome despite favorable score prediction, can often be attributed to hospital complications [43]. In ICH, a study in the INTERACT 2 cohort showed that in 17% of patients, the hospital course was complicated by either early or delayed neurologic deterioration, with early worsening being defined as deterioration within 24 h and delayed worsening being defined as deterioration between 24 h and 7 days relative to the index ICH [47]. Imaging correlates of this clinical worsening may be intraparenchymal or intraventricular hemorrhage expansion which, if present, usually occur within 24 h of admission. Both processes have been linked to outcome [48,49,50,51]. Development of hydrocephalus and perihemorrhagic edema are examples of dynamic processes that impact outcome at even later time points. Hydrocephalus typically develops days to weeks after the index ICH, while perihemorrhagic edema volume peaks around 2 weeks into the hospital course [52,53,54]. This lends further support to the idea of repeat prognostication during and towards the end of the hospitalization.
Beyond the acute hospitalization patients with ICH are at increased risk for ischemic stroke as well which may impact long-term outcomes [55, 56]. Current ICH scores do not fully capture the disease and complication burden, which constitutes a potential source of false predictions.
Timing of outcome assessment is not standardized in current prediction scores ranging from in-hospital events to up to 1 year after the index ICH (Table 2). Performance measures cannot be compared between scores if they predict different disease states in time. To clinicians and patient families, three outcome time points seem to be most relevant: the first 7 days (here especially risk of death by the end of the first week), “post-acute” outcome at 90 days (used in most randomized controlled trials), and long-term outcome at 1 year. Early prediction (e.g. within 48 h) is warranted for 7-day mortality risk, while for the 90-days and 1-year time points more input variables across the hospital stay can be gathered. This approach takes advantage of longitudinally updated prognostic information that would otherwise be lost. Similar recommendations have been made for outcome assessment after subarachnoid hemorrhage [57]. Further sources of loss of prognostic information include the common practice of dichotomizing outcome scales (discussed below), and the creation of a prediction score itself. Not only are final score numbers usually the result of rounding, which sacrifices information. They also encode different risk constellations by assigning them identical numbers. For example, on the ICH score an 81-year-old with a 5 ml ICH gets 1 point for his age (> = 80) and no points for his relatively small ICH volume while a 25-year-old with a 35 ml ICH gets 1 point as well (no points for age, 1 point for ICH volume). This assignment of identical scores for likely very different risk constellations can be prevented by the use of continuous scales, where the distance between numbers is equal and proportionally reflects risk.
Framework for future ICH prediction scores
A 2019-analysis, conducted jointly by members of the US American and German Neurocritical Care Societies, identified gaps of prognostication in neurocritical care. Gaps in ICH outcomes research include the determination of the best timing of score assessment, addressing the WOC bias as it may confound score derivation, and integration of new predictor variables in future scores [58]. Future scores should thus be derived in maximally treated patient cohorts [27, 59]. Patients with very early care limitations, e.g. patients with DNR/DNI status upon arrival in the emergency room, must be excluded from future score derivation cohorts as aggressive care in these patients would be unethical [59].
Quality measures for score development and validation
Both the American Heart Association (AHA) and the Neurocritical Care Society (NCS) have emphasized the importance of standardized development and reporting of high-quality prediction models for stroke and neurocritical care [58]. The Progress Study Group has outlined quality measures regarding identification of prognostication endpoints, the factors that are associated with these endpoints and creation of prognostic models. Complete validation of prediction models is an indispensable part of score development [40]. The validation of the Essen score described in the results section of this article may serve as an example of a complete score validation, including quantification of discrimination, calibration and net benefit.
Integration of new predictor variables
Table 3 provides an overview on candidate variables described in the literature for future prediction scores, based on studies linking these variables to outcome after ICH. Of note, these studies may be subject to publication bias [72]. Moreover, an association of a variable with clinical outcome, even if reproducible across multiple studies, does not guarantee that the variable will improve the performance of a prediction model.
Beyond binary outcomes: modified Rankin scale and patient-reported outcomes
The mRS is the most frequently used outcome measure in stroke trials. It has been criticized for being poorly reproducible, for having score grades that are not in proportion with each other, for not distributing patients normally among its score values, and for being heavily focused on mobility rather than cognitive or social functioning [73, 74]. Furthermore, dichotomization – which is also common practice in current ICH prediction scores – leads to loss of prognostic information (Table 2). Its use has been fueled by statistical packages which often contain logistic regression for binary outcomes. Both statistically and clinically, dichotomization is an unhelpful over-simplification.
Toward the goal of patient-centered outcomes quantification, PROMs have been proposed. The patient reported outcomes information system (PROMIS) is one example of a detailed assessment tool, designed for multiple disease entities. It includes domains such as physical function, social roles, pain, fatigue, anxiety and sleep [75]. A similar tool, specifically for the use in neurological disorders, is the Quality of Life in Neurological disorders (NeuroQuol) tool set, consisting of brief PROM surveys across 13 domains [76]. Further frequently used PROM scales include the EQ-5D, the Sickness Impact Profile, the Telephone Interview for Cognitive Status (TICS) and the SF-36. The prospective Patient Reported Outcomes in Stroke Care (EPOS, NCT03795948) study as well as the coordinated treatment of stroke patients with patient-orientated outcome measurement (StroCare, NCT04159324) study will hopefully further characterize the role PROMs in stroke-related outcomes research [77, 78]
Pragmatic prognostication in clinical practice
The 2015 AHA guidelines on the management of ICH recommend the use of a severity score at the time of presentation, such as the NIHSS or ICH score. However, basing the prognosis on a single scoring system is discouraged [41]. The NCS, and the American Academy of Neurology affirm the AHA guideline, but neither these two societies nor the Society of Critical Care Medicine provide their own dedicated ICH guidelines.
Despite the above-mentioned shortcomings of available ICH outcome prediction scores, it may be reasonable to approach the prognosis using one of the current scores, ideally one that underwent the most thorough testing over the years, i.e. the ICH score or the Essen score. As a principle, it is recommended to never base the prognosis on one score result alone [41] but rather to consider all information relevant to the patient’s best interest (Table 4).
Limitations
This review has limitations. First, the reader should be aware that, using only pubmed as a data source and conducting the literature search over a limited time period, our review can be considered a rapid review but does not fulfill all criteria required for a systematic review. Second, scores developed in other disease entities and then used for ICH prediction are not included in our paper. This is also true for clinical scales such as the GCS or the NIHSS which have been used in some publications to predict outcome after ICH. These publications are partially referenced here but are not included in the literature review portion. Third, when demonstrating score validation using the Essen ICH score, the endpoint (Barthel Index) that the Essen score was developed for was not available in the validation cohort. Strictly speaking, we did not validate the original Essen score but a variation of the Essen score using the mRS instead of the Barthel index as outcome. Therefore further validation of the original score would be needed if the Essen score were to be used for clinical decision making.
Conclusion
Despite prediction score fatigue among clinicians, prognostication in patients with ICH remains crucially important. It may improve clinical care by providing information on the most probable outcome, which can then be aligned with what is medically feasible and what the patient wants. Prediction models may also be used to risk-stratify participants of clinical trials, which may ultimately facilitate implementation of new therapies. Currently available prediction scores do not have a unified modeling approach or type or timing of outcome assessment. In this article we describe necessary premises for the development of more reliable ICH prediction scores. Future scores need to be developed in maximally treated patient cohorts to ameliorate the WOC bias. The timing of score and outcome assessments needs to be standardized: we propose capturing predictors within 24 h after the index bleed for in-hospital prognostication, and re-capturing information at 7 days to determine prognosis at 90 days. We propose to consistently use the mRS as a disability scale, and to add PROMs to obtain a complete picture of outcomes that matter to patients and families. Lastly, score development requires rigorous validation including discrimination, calibration and net benefit analyses. Until improved prognostic scores are available, we encourage clinicians to learn about the shortcomings of current ICH scores and use them with these caveats in mind.
Availability of data and materials
The dataset analyzed during the current study is not publicly available. Upon reasonable request questions regarding the current analysis will be answered in detail by the corresponding author.
References
Group, G. B. D. N. D. C (2017). Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurology, 16(11), 877–897 https://doi.org/10.1016/S1474-4422(17)30299-5.
Lioutas, V. A., Beiser, A. S., Aparicio, H. J., Himali, J. J., Selim, M. H., Romero, J. R., & Seshadri, S. (2020). Assessment of incidence and risk factors of intracerebral hemorrhage among participants in the Framingham heart study between 1948 and 2016. JAMA Neurology, 77(10), 1252 https://doi.org/10.1001/jamaneurol.2020.1512.
Chen, Y., Wright, N., Guo, Y., Turnbull, I., Kartsonaki, C., Yang, L., … China Kadoorie Biobank Collaborative, G. (2020). Mortality and recurrent vascular events after first incident stroke: a 9-year community-based study of 0.5 million Chinese adults. The Lancet Global Health, 8(4), e580–e590 https://doi.org/10.1016/S2214-109X(20)30069-3.
Katzan, I. L., Schuster, A., Newey, C., Uchino, K., & Lapin, B. (2018). Patient-reported outcomes across cerebrovascular event types: More similar than different. Neurology, 91(23), e2182–e2191 https://doi.org/10.1212/WNL.0000000000006626.
Bosel, J., Kowoll, C., Kahmann, J., Dziewas, R., Schirotzek, I., & Dohmen, C. (2012). Survey study: Update on neurological intensive care in Germany 2012: Structure, standards and scores in neurological intensive care units. Nervenarzt, 83(12), 1609–1618 https://doi.org/10.1007/s00115-012-3541-6.
Hwang, D. Y., Dell, C. A., Sparks, M. J., Watson, T. D., Langefeld, C. D., Comeau, M. E., … Sheth, K. N. (2016). Clinician judgment vs formal scales for predicting intracerebral hemorrhage outcomes. Neurology, 86(2), 126–133 https://doi.org/10.1212/wnl.0000000000002266.
McCracken, D. J., Lovasik, B. P., McCracken, C. E., Frerich, J. M., McDougal, M. E., Ratcliff, J. J., … Pradilla, G. (2019). The intracerebral hemorrhage score: A self-fulfilling prophecy? Neurosurgery, 84(3), 741–748 https://doi.org/10.1093/neuros/nyy193.
Moons, K. G., de Groot, J. A., Bouwmeester, W., Vergouwe, Y., Mallett, S., Altman, D. G., … Collins, G. S. (2014). Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Medicine, 11(10), e1001744 https://doi.org/10.1371/journal.pmed.1001744.
Weimar, C., Benemann, J., Diener, H. C., & German Stroke Study, C (2006). Development and validation of the Essen intracerebral haemorrhage score. Journal of Neurology, Neurosurgery, and Psychiatry, 77(5), 601–605 https://doi.org/10.1136/jnnp.2005.081117.
Sprugel, M. I., Kuramatsu, J. B., Gerner, S. T., Sembill, J. A., Beuscher, V. D., Hagen, M., … Huttner, H. B. (2018). Antiplatelet therapy in primary spontaneous and oral anticoagulation-associated intracerebral hemorrhage. Stroke, 49(11), 2621–2629 https://doi.org/10.1161/strokeaha.118.021614.
Tuhrim, S., Dambrosia, J. M., Price, T. R., Mohr, J. P., Wolf, P. A., Heyman, A., & Kase, C. S. (1988). Prediction of intracerebral hemorrhage survival. Annals of Neurology, 24(2), 258–263 https://doi.org/10.1002/ana.410240213.
Tuhrim, S., Dambrosia, J. M., Price, T. R., Mohr, J. P., Wolf, P. A., Hier, D. B., & Kase, C. S. (1991). Intracerebral hemorrhage: External validation and extension of a model for prediction of 30-day survival. Annals of Neurology, 29(6), 658–663 https://doi.org/10.1002/ana.410290614.
Broderick, J. P., Brott, T. G., Duldner, J. E., Tomsick, T., & Huster, G. (1993). Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke, 24(7), 987–993 https://doi.org/10.1161/01.str.24.7.987.
Mase, G., Zorzon, M., Biasutti, E., Tasca, G., Vitrani, B., & Cazzato, G. (1995). Immediate prognosis of primary intracerebral hemorrhage using an easy model for the prediction of survival. Acta Neurologica Scandinavica, 91(4), 306–309 https://doi.org/10.1111/j.1600-0404.1995.tb07011.x.
Hemphill 3rd, J. C., Bonovich, D. C., Besmertis, L., Manley, G. T., & Johnston, S. C. (2001). The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke, 32(4), 891–897 https://doi.org/10.1161/01.STR.32.4.891.
Cheung, R. T., & Zou, L. Y. (2003). Use of the original, modified, or new intracerebral hemorrhage score to predict mortality and morbidity after intracerebral hemorrhage. Stroke, 34(7), 1717–1722 https://doi.org/10.1161/01.Str.0000078657.22835.B9.
Godoy, D. A., Pinero, G., & Di Napoli, M. (2006). Predicting mortality in spontaneous intracerebral hemorrhage: Can modification to original score improve the prediction? Stroke, 37(4), 1038–1044 https://doi.org/10.1161/01.Str.0000206441.79646.49.
Ruiz-Sandoval, J. L., Chiquete, E., Romero-Vargas, S., Padilla-Martinez, J. J., & Gonzalez-Cornejo, S. (2007). Grading scale for prediction of outcome in primary intracerebral hemorrhages. Stroke, 38(5), 1641–1644 https://doi.org/10.1161/strokeaha.106.478222.
Cho, D. Y., Chen, C. C., Lee, W. Y., Lee, H. C., & Ho, L. H. (2008). A new modified intracerebral hemorrhage score for treatment decisions in basal ganglia hemorrhage--a randomized trial. Critical Care Medicine, 36(7), 2151–2156 https://doi.org/10.1097/CCM.0b013e318173fc99.
Rost, N. S., Smith, E. E., Chang, Y., Snider, R. W., Chanderraj, R., Schwab, K., … Rosand, J. (2008). Prediction of functional outcome in patients with primary intracerebral hemorrhage: the FUNC score. Stroke, 39(8), 2304–2309 https://doi.org/10.1161/STROKEAHA.107.512202.
Chuang, Y. C., Chen, Y. M., Peng, S. K., & Peng, S. Y. (2009). Risk stratification for predicting 30-day mortality of intracerebral hemorrhage. International Journal for Quality in Health Care, 21(6), 441–447 https://doi.org/10.1093/intqhc/mzp041.
Li, Y. F., Luo, J., Li, Q., Jing, Y. J., Wang, R. Y., & Li, R. S. (2012). A new simple model for prediction of hospital mortality in patients with intracerebral hemorrhage. CNS Neuroscience & Therapeutics, 18(6), 482–486 https://doi.org/10.1111/j.1755-5949.2012.00320.x.
Ji, R., Shen, H., Pan, Y., Wang, P., Liu, G., Wang, Y., … Wang, Y. (2013). A novel risk score to predict 1-year functional outcome after intracerebral hemorrhage and comparison with existing scores. Critical Care, 17(6), R275 https://doi.org/10.1186/cc13130.
Romero, J. M., Brouwers, H. B., Lu, J., Delgado Almandoz, J. E., Kelly, H., Heit, J., … Gonzalez, R. G. (2013). Prospective validation of the computed tomographic angiography spot sign score for intracerebral hemorrhage. Stroke, 44(11), 3097–3102 https://doi.org/10.1161/strokeaha.113.002752.
Zis, P., Leivadeas, P., & Tavernarakis, A. (2015). EDICH; a novel grading scale for predicting the 30-day case fatality of primary inoperable intracerebral hemorrhage. Journal of Stroke and Cerebrovascular Diseases, 24(5), 1104–1105 https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.01.014.
Gupta, V. P., Garton, A. L. A., Sisti, J. A., Christophe, B. R., Lord, A. S., Lewis, A. K., … Connolly Jr., E. S. (2017). Prognosticating functional outcome after intracerebral hemorrhage: The ICHOP score. World Neurosurgery, 101, 577–583 https://doi.org/10.1016/j.wneu.2017.02.082.
Sembill, J. A., Gerner, S. T., Volbers, B., Bobinger, T., Lucking, H., Kloska, S. P., … Kuramatsu, J. B. (2017). Severity assessment in maximally treated ICH patients: The max-ICH score. Neurology, 89(5), 423–431 https://doi.org/10.1212/WNL.0000000000004174.
Braksick, S. A., Hemphill 3rd, J. C., Mandrekar, J., Wijdicks, E. F. M., & Fugate, J. E. (2018). Application of the FOUR score in intracerebral hemorrhage risk analysis. Journal of Stroke and Cerebrovascular Diseases, 27(6), 1565–1569 https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.01.008.
Sembill, J. A., Castello, J. P., Sprugel, M. I., Gerner, S. T., Hoelter, P., Lucking, H., … Kuramatsu, J. B. (2021). Multicenter validation of the max-ICH score in intracerebral hemorrhage. Annals of Neurology, 89(3), 474–484 https://doi.org/10.1002/ana.25969.
Vickers, A. J., van Calster, B., & Steyerberg, E. W. (2019). A simple, step-by-step guide to interpreting decision curve analysis. Diagn Progn Res, 3(1), 18 https://doi.org/10.1186/s41512-019-0064-7.
Gregorio, T., Pipa, S., Cavaleiro, P., Atanasio, G., Albuquerque, I., Chaves, P. C., & Azevedo, L. (2018). Prognostic models for intracerebral hemorrhage: Systematic review and meta-analysis. BMC Medical Research Methodology, 18(1), 145 https://doi.org/10.1186/s12874-018-0613-8.
Hemphill 3rd, J. C., Farrant, M., & Neill Jr., T. A. (2009). Prospective validation of the ICH score for 12-month functional outcome. Neurology, 73(14), 1088–1094 https://doi.org/10.1212/WNL.0b013e3181b8b332.
Parry-Jones, A. R., Abid, K. A., Di Napoli, M., Smith, C. J., Vail, A., Patel, H. C., … Tyrrell, P. J. (2013). Accuracy and clinical usefulness of intracerebral hemorrhage grading scores: a direct comparison in a UK population. Stroke, 44(7), 1840–1845 https://doi.org/10.1161/strokeaha.113.001009.
Becker, K. J., Baxter, A. B., Cohen, W. A., Bybee, H. M., Tirschwell, D. L., Newell, D. W., … Longstreth Jr., W. T. (2001). Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology, 56(6), 766–772 https://doi.org/10.1212/WNL.56.6.766.
Reznik, M. E., Moody, S., Murray, K., Costa, S., Grory, B. M., Madsen, T. E., … Furie, K. L. (2020). The impact of delirium on withdrawal of life-sustaining treatment after intracerebral hemorrhage. Neurology, 95(20), e2727–e2735 https://doi.org/10.1212/WNL.0000000000010738.
Zahuranec, D. B., Morgenstern, L. B., Sanchez, B. N., Resnicow, K., White, D. B., & Hemphill 3rd., J. C. (2010). Do-not-resuscitate orders and predictive models after intracerebral hemorrhage. Neurology, 75(7), 626–633 https://doi.org/10.1212/WNL.0b013e3181ed9cc9.
Weimer, J. M., Nowacki, A. S., & Frontera, J. A. (2016). Withdrawal of life-sustaining therapy in patients with intracranial hemorrhage: Self-fulfilling prophecy or accurate prediction of outcome? Critical Care Medicine, 44(6), 1161–1172 https://doi.org/10.1097/ccm.0000000000001570.
Morgenstern, L. B., Zahuranec, D. B., Sanchez, B. N., Becker, K. J., Geraghty, M., Hughes, R., … Hemphill 3rd, J. C. (2015). Full medical support for intracerebral hemorrhage. Neurology, 84(17), 1739–1744 https://doi.org/10.1212/wnl.0000000000001525.
Zahuranec, D. B., Fagerlin, A., Sanchez, B. N., Roney, M. E., Thompson, B. B., Fuhrel-Forbis, A., & Morgenstern, L. B. (2016). Variability in physician prognosis and recommendations after intracerebral hemorrhage. Neurology, 86(20), 1864–1871 https://doi.org/10.1212/wnl.0000000000002676.
Steyerberg, E. W., Moons, K. G., van der Windt, D. A., Hayden, J. A., Perel, P., Schroter, S., … Group, P (2013). Prognosis research strategy (PROGRESS) 3: Prognostic model research. PLoS Medicine, 10(2), e1001381 https://doi.org/10.1371/journal.pmed.1001381.
Hemphill 3rd, J. C., Greenberg, S. M., Anderson, C. S., Becker, K., Bendok, B. R., Cushman, M., … Council on Clinical, C (2015). Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke, 46(7), 2032–2060 https://doi.org/10.1161/STR.0000000000000069.
Holloway, R. G., Arnold, R. M., Creutzfeldt, C. J., Lewis, E. F., Lutz, B. J., McCann, R. M., … Council on Clinical, C (2014). Palliative and end-of-life care in stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 45(6), 1887–1916 https://doi.org/10.1161/STR.0000000000000015.
Witsch, J., Frey, H. P., Patel, S., Park, S., Lahiri, S., Schmidt, J. M., … Claassen, J. (2016). Prognostication of long-term outcomes after subarachnoid hemorrhage: The FRESH score. Annals of Neurology, 80(1), 46–58 https://doi.org/10.1002/ana.24675.
Witsch, J., Kuohn, L., Hebert, R., Cord, B., Sansing, L., Gilmore, E. J., … Sheth, K. N. (2019b). Early prognostication of 1-year outcome after subarachnoid hemorrhage: The FRESH score validation. Journal of Stroke and Cerebrovascular Diseases, 28(10), 104280 https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.06.038.
Lun, R., Yogendrakumar, V., Demchuk, A. M., Aviv, R. I., Rodriguez-Luna, D., Molina, C. A., … Dowlatshahi, D. (2020). Calculation of prognostic scores, using delayed imaging, outperforms baseline assessments in acute intracerebral hemorrhage. Stroke, 51(4), 1107–1110 https://doi.org/10.1161/STROKEAHA.119.027119.
Maas, M. B., Francis, B. A., Sangha, R. S., Lizza, B. D., Liotta, E. M., & Naidech, A. M. (2017). Refining prognosis for intracerebral hemorrhage by early reassessment. Cerebrovascular Diseases, 43(3–4), 110–116 https://doi.org/10.1159/000452679.
You, S., Zheng, D., Delcourt, C., Sato, S., Cao, Y., Zhang, S., … Chalmers, J. (2019). Determinants of early versus delayed neurological deterioration in intracerebral hemorrhage. Stroke, 50(6), 1409–1414 https://doi.org/10.1161/strokeaha.118.024403.
Al-Shahi Salman, R., Frantzias, J., Lee, R. J., Lyden, P. D., Battey, T. W. K., Ayres, A. M., … Collaborators, I. C. H. G. I. P. D. M.-a (2018). Absolute risk and predictors of the growth of acute spontaneous intracerebral haemorrhage: a systematic review and meta-analysis of individual patient data. Lancet Neurology, 17(10), 885–894 https://doi.org/10.1016/S1474-4422(18)30253-9.
Li, Q., Li, R., Zhao, L. B., Yang, X. M., Yang, W. S., Deng, L., … Xie, P. (2020). Intraventricular Hemorrhage Growth: Definition, Prevalence and Association with Hematoma Expansion and Prognosis. Neurocrit Care https://doi.org/10.1007/s12028-020-00958-8.
Witsch, J., Bruce, E., Meyers, E., Velazquez, A., Schmidt, J. M., Suwatcharangkoon, S., … Claassen, J. (2015). Intraventricular hemorrhage expansion in patients with spontaneous intracerebral hemorrhage. Neurology, 84(10), 989–994 https://doi.org/10.1212/WNL.0000000000001344.
Yogendrakumar, V., Ramsay, T., Fergusson, D., Demchuk, A. M., Aviv, R. I., Rodriguez-Luna, D., … the, P. S. C. T. A. S. G (2019). New and expanding ventricular hemorrhage predicts poor outcome in acute intracerebral hemorrhage. Neurology, 93(9), e879–e888 https://doi.org/10.1212/WNL.0000000000008007.
Diringer, M. N., Edwards, D. F., & Zazulia, A. R. (1998). Hydrocephalus: a previously unrecognized predictor of poor outcome from supratentorial intracerebral hemorrhage. Stroke, 29(7), 1352–1357 https://doi.org/10.1161/01.str.29.7.1352.
Hu, R., Zhang, C., Xia, J., Ge, H., Zhong, J., Fang, X., … Feng, H. (2021). Long-term outcomes and risk factors related to hydrocephalus after intracerebral hemorrhage. Translational Stroke Research, 12(1), 31–38 https://doi.org/10.1007/s12975-020-00823-y.
Sprugel, M. I., Kuramatsu, J. B., Volbers, B., Gerner, S. T., Sembill, J. A., Madzar, D., … Huttner, H. B. (2019). Perihemorrhagic edema: Revisiting hematoma volume, location, and surface. Neurology, 93(12), e1159–e1170 https://doi.org/10.1212/wnl.0000000000008129.
Murthy, S. B., Diaz, I., Wu, X., Merkler, A. E., Iadecola, C., Safford, M. M., … Kamel, H. (2020). Risk of arterial ischemic events after intracerebral hemorrhage. Stroke, 51(1), 137–142 https://doi.org/10.1161/STROKEAHA.119.026207.
Witsch, J., Merkler, A. E., Chen, M. L., Navi, B. B., Sheth, K. N., Freedman, B., … Kamel, H. (2018). Incidence of atrial fibrillation in patients with recent ischemic stroke versus matched controls. Stroke, 49(10), 2529–2531 https://doi.org/10.1161/STROKEAHA.118.022826.
Stienen, M. N., Visser-Meily, J. M., Schweizer, T. A., Hanggi, D., Macdonald, R. L., Vergouwen, M. D. I., … Investigators, S. C. P. (2019). Prioritization and timing of outcomes and endpoints after aneurysmal subarachnoid hemorrhage in clinical trials and observational studies: Proposal of a multidisciplinary research group. Neurocritical Care, 30(Suppl 1), 102–113 https://doi.org/10.1007/s12028-019-00737-0.
Wartenberg, K. E., Hwang, D. Y., Haeusler, K. G., Muehlschlegel, S., Sakowitz, O. W., Madzar, D., … Varelas, P. N. (2019). Gap analysis regarding prognostication in neurocritical care: A joint statement from the German Neurocritical Care Society and the Neurocritical Care Society. Neurocritical Care, 31(2), 231–244 https://doi.org/10.1007/s12028-019-00769-6.
Parry-Jones, A. R., Sammut-Powell, C., Paroutoglou, K., Birleson, E., Rowland, J., Lee, S., … Patel, H. (2019). An intracerebral hemorrhage care bundle is associated with lower case fatality. Annals of Neurology, 86(4), 495–503 https://doi.org/10.1002/ana.25546.
Huang, Y., Chen, J., Zhong, S., & Yuan, J. (2016). Role of APACHE II scoring system in the prediction of severity and outcome of acute intracerebral hemorrhage. The International Journal of Neuroscience, 126(11), 1020–1024 https://doi.org/10.3109/00207454.2015.1099099.
Roh, D. J., Albers, D. J., Magid-Bernstein, J., Doyle, K., Hod, E., Eisenberger, A., … Claassen, J. (2019). Low hemoglobin and hematoma expansion after intracerebral hemorrhage. Neurology, 93(4), e372–e380 https://doi.org/10.1212/WNL.0000000000007820.
Lattanzi, S., Cagnetti, C., Rinaldi, C., Angelocola, S., Provinciali, L., & Silvestrini, M. (2018). Neutrophil-to-lymphocyte ratio improves outcome prediction of acute intracerebral hemorrhage. Journal of the Neurological Sciences, 387, 98–102 https://doi.org/10.1016/j.jns.2018.01.038.
Wan, J., Wang, X., Zhen, Y., Chen, X., Yao, P., Liu, W., … Zhao, S. (2020). The predictive role of the neutrophil-lymphocyte ratio in the prognosis of adult patients with stroke. Chinese Neurosurgical Journal, 6(1), 22 https://doi.org/10.1186/s41016-020-00201-5.
Ko, S. B., Choi, H. A., Parikh, G., Helbok, R., Schmidt, J. M., Lee, K., … Mayer, S. A. (2011). Multimodality monitoring for cerebral perfusion pressure optimization in comatose patients with intracerebral hemorrhage. Stroke, 42(11), 3087–3092 https://doi.org/10.1161/strokeaha.111.623165.
Yang, G., Hu, R., Zhang, C., Qian, C., Luo, Q. Q., Yung, W. H., … Qian, Z. M. (2016). A combination of serum iron, ferritin and transferrin predicts outcome in patients with intracerebral hemorrhage. Scientific Reports, 6(1), 21970 https://doi.org/10.1038/srep21970.
Beuscher, V. D., Sprugel, M. I., Gerner, S. T., Sembill, J. A., Madzar, D., Reindl, C., … Huttner, H. B. (2020). Chronic kidney disease and clinical outcomes in patients with intracerebral hemorrhage. Journal of Stroke and Cerebrovascular Diseases, 29(8), 104802 https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104802.
Witsch, J., Falcone, G. J., Leasure, A. C., Matouk, C., Endres, M., Sansing, L., … Sheth, K. N. (2021). Intracerebral hemorrhage with Intraventricular extension associated with loss of consciousness at symptom onset. Neurocritical Care. https://doi.org/10.1007/s12028-020-01180-2.
Volbers, B., Giede-Jeppe, A., Gerner, S. T., Sembill, J. A., Kuramatsu, J. B., Lang, S., … Huttner, H. B. (2018). Peak perihemorrhagic edema correlates with functional outcome in intracerebral hemorrhage. Neurology, 90(12), e1005–e1012 https://doi.org/10.1212/WNL.0000000000005167.
Sporns, P. B., Kemmling, A., Schwake, M., Minnerup, J., Nawabi, J., Broocks, G., … Hanning, U. (2018). Triage of 5 noncontrast computed tomography markers and spot sign for outcome prediction after intracerebral hemorrhage. Stroke, 49(10), 2317–2322 https://doi.org/10.1161/STROKEAHA.118.021625.
Boulouis, G., Morotti, A., Brouwers, H. B., Charidimou, A., Jessel, M. J., Auriel, E., … Goldstein, J. N. (2016). Noncontrast computed tomography hypodensities predict poor outcome in intracerebral hemorrhage patients. Stroke, 47(10), 2511–2516 https://doi.org/10.1161/strokeaha.116.014425.
Claassen, J., Jette, N., Chum, F., Green, R., Schmidt, M., Choi, H., … Hirsch, L. J. (2007). Electrographic seizures and periodic discharges after intracerebral hemorrhage. Neurology, 69(13), 1356–1365 https://doi.org/10.1212/01.wnl.0000281664.02615.6c.
Witsch, J., Al-Mufti, F., Connolly, E. S., Agarwal, S., Melmed, K., Roh, D. J., … Park, S. (2019a). Statins and perihemorrhagic edema in patients with spontaneous intracerebral hemorrhage. Neurology. https://doi.org/10.1212/WNL.0000000000006931.
Naidech, A. M., Beaumont, J. L., Berman, M., Francis, B., Liotta, E., Maas, M. B., … Cella, D. (2015). Dichotomous “good outcome” indicates mobility more than cognitive or social quality of life. Critical Care Medicine, 43(8), 1654–1659 https://doi.org/10.1097/ccm.0000000000001082.
Quinn, T. J., Dawson, J., Walters, M. R., & Lees, K. R. (2007). Reliability of the modified Rankin scale. Stroke, 38(11), e144; author reply e145 https://doi.org/10.1161/STROKEAHA.107.490110.
Broderick, J. E., DeWitt, E. M., Rothrock, N., Crane, P. K., & Forrest, C. B. (2013). Advances in patient-reported outcomes: The NIH PROMIS((R)) Measures. EGEMS (Wash DC), 1(1), 1015 https://doi.org/10.13063/2327-9214.1015.
Cella, D., Lai, J. S., Nowinski, C. J., Victorson, D., Peterman, A., Miller, D., … Moy, C. (2012). Neuro-QOL: Brief measures of health-related quality of life for clinical research in neurology. Neurology, 78(23), 1860–1867 https://doi.org/10.1212/WNL.0b013e318258f744.
Rimmele, D. L., Lebherz, L., Frese, M., Appelbohm, H., Bartz, H. J., Kriston, L., … Thomalla, G. (2019). Outcome evaluation by patient reported outcome measures in stroke clinical practice (EPOS) protocol for a prospective observation and implementation study. Neurological Research and Practice, 1(1), 28 https://doi.org/10.1186/s42466-019-0034-0.
Rimmele, D. L., Schrage, T., Brettschneider, C., Engels, A., Gerloff, C., Harter, M., … Thomalla, G. (2021). Rationale and design of an interventional study of cross-sectoral, coordinated treatment of stroke patients with patient-orientated outcome measurement (StroCare). Neurological Research and Practice, 3(1), 7 https://doi.org/10.1186/s42466-021-00107-2.
Acknowledgements
None.
Funding
There was no targeted funding for this study.
Author information
Authors and Affiliations
Contributions
Jens Witsch designed and conceptualized the study, analyzed the data, and drafted and revised the manuscript for intellectual content. Bob Siegerink designed and conceptualized the study, conducted the statistical analysis, and partially drafted and revised the manuscript for intellectual content. Christian Nolte conceptualized the study and revised the manuscript for intellectual content. Maximilian Sprügel had a major role in the acquisition of data. Thorsten Steiner conceptualized the study and revised the manuscript for intellectual content. Matthias Endres conceptualized the study and revised the manuscript for intellectual content. Hagen B. Huttner had a major role in the acquisition of the data, analyzed the data, and revised the manuscript for intellectual content. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The UKER ICH-cohort study was approved by the ethics committees and institutional review boards based on the central vote from Friedrich-Alexander-University Erlangen-Nuremberg, Germany.
Consent for publication
Not applicable.
Competing interests
Dr. Witsch is an editorial team member of the Resident & Fellow section of Neurology. Dr. Siegerink reports no disclosures. Dr. Nolte received research grants from German Ministry of Research and Education, German Center for Neurodegenerative Diseases, German Center for cardiovascular Research, and speaker and/or consultation fees from Boehringer Ingelheim, Bristol-Myers Squibb, Pfizer Pharma, Portola and Abbott. Dr. Sprügel reports no disclosures. Dr. Steiner reports no disclosures. Dr. Endres reports grant support from Bayer, the German Research Foundation (DFG), the German Federal Ministry of Education and Research (BMBF), the German Center for Neurodegenerative Diseases (DZNE), the German Center for Cardiovascular Research (DZHK), the European Union, Corona Foundation, and Fondation Leducq; and fees paid to the Charité from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Pfizer, Daiichi Sankyo, Amgen, GlaxoSmithKline, Sanofi, Covidien, Novartis, all outside the submitted work. Dr. Huttner reports no disclosures.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Witsch, J., Siegerink, B., Nolte, C.H. et al. Prognostication after intracerebral hemorrhage: a review. Neurol. Res. Pract. 3, 22 (2021). https://doi.org/10.1186/s42466-021-00120-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42466-021-00120-5