Abstract
Background
Previous studies have quantified repolarization variability using time-domain, frequency-domain and nonlinear analysis in mouse hearts. Here, we investigated the relationship between these parameters and ventricular arrhythmogenicity in a hypokalaemia model of acquired long QT syndrome.
Methods
Left ventricular monophasic action potentials (MAPs) were recorded during right ventricular regular 8 Hz pacing during normokalaemia (5.2 mM [K+]), hypokalaemia modeling LQTS (3 mM [K+]) or hypokalaemia with 0.1 mM heptanol in Langendorff-perfused mouse hearts.
Results
During normokalaemia, mean APD was 33.5 ± 3.7 ms. Standard deviation (SD) of APDs was 0.63 ± 0.33 ms, coefficient of variation was 1.9 ± 1.0% and the root mean square (RMS) of successive differences in APDs was 0.3 ± 0.1 ms. Low- and high-frequency peaks were 0.6 ± 0.5 and 2.3 ± 0.7 Hz, respectively, with percentage powers of 38 ± 22 and 61 ± 23%. Poincaré plots of APDn+1 against APDn revealed ellipsoid morphologies with SD along the line-of-identity (SD2) to SD perpendicular to the line-of-identity (SD1) ratio of 4.6 ± 1.1. Approximate and sample entropy were 0.49 ± 0.12 and 0.64 ± 0.29, respectively. Detrended fluctuation analysis revealed short- and long-term fluctuation slopes of 1.62 ± 0.27 and 0.60 ± 0.18, respectively. Hypokalaemia provoked ventricular tachycardia in six of seven hearts, prolonged APDs (51.2 ± 7.9 ms), decreased SD2/SD1 ratio (3.1 ± 1.0), increased approximate and sample entropy (0.68 ± 0.08 and 1.02 ± 0.33) and decreased short-term fluctuation slope (1.23 ± 0.20) (ANOVA, P < 0.05). Heptanol prevented VT in all hearts studied without further altering the above repolarization parameters observed during hypokalaemia.
Conclusion
Reduced SD2/SD1, increased entropy and decreased short-term fluctuation slope may reflect arrhythmic risk in hypokalaemia. Heptanol exerts anti-arrhythmic effects without affecting repolarization variability.
Similar content being viewed by others
Introduction
Long QT syndrome (LQTS) is an important clinical condition predisposing to the occurrence of ventricular tachyarrhythmias, which can lead to sudden cardiac death. It can have congenital or acquired causes, the latter reflected by electrolyte disturbances such as hypokalemia or certain drugs that block potassium channels. Of these, hypokalaemia is the commonest electrolyte abnormality observed in patients who are admitted to the hospital [1] and is an important cause of arrhythmias and associated mortality clinically [2]. It is frequently observed in patients with pre-existing heart conditions [3,4,5]. Previously, several important re-entrant substrates of hypokalaemia have been identified using pre-clinical models [6,7,8,9]. These include repolarization abnormalities in the form of action potential prolongation, increased transmural dispersion of repolarization, reduced refractoriness, steep restitution gradients and increased amplitude of repolarization alternans [10, 11].
Moreover, altered beat-to-beat variations in the repolarization time-course have been associated with arrhythmogenesis in other pharmacological or disease models [12, 13]. For example, higher degrees of short-term repolarization variability using Poincaré plot analysis were associated with the development of ventricular arrhythmias in dogs [14]. Moreover, a combined experimental and computational approach associated higher repolarization variability with pro-arrhythmic abnormalities [15]. Finally, high entropy was shown to predict arrhythmic outcomes following gap junction and sodium channel inhibition in a mouse model [16]. However, whether variability or complexity of beat-to-beat repolarization variability plays a role in hypokalaemia modeling LQTS has never been studied. We hypothesized that increased repolarization variability contributes to arrhythmic substrate in an experimental mouse model of LQTS using hypokalaemia.
Materials and methods
This study received approval from the University of Cambridge (Approval Number: BB/G017565/1). The methodology used in this study has previously been described by us in detail. The reader is directed to this publication for further details [16]. Langendorff-perfused mouse hearts were used for the experiments, as described previously [17,18,19]. Monophasic action potential (MAP) waveforms were obtained from the left ventricular epicardium during right ventricular stimulation. MAP waveforms must have met established criteria for MAP signals and those that did not were rejected [20, 21]. They must have stable baselines, fast upstrokes, with no inflections or negative spikes, and a rapid first phase of repolarization. 0% repolarization was measured at the peak of the MAP and 100% repolarization was measured at the point of return of the potential to baseline [20, 22, 23].
Results
Action potential duration variability determined using time-domain methods
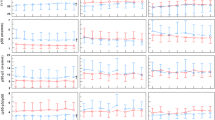
Our previous work has reported the pro-arrhythmic effects of hypokalaemia and anti-arrhythmic effects of 0.1 mM heptanol under hypokalaemic conditions [24] and also the time- and dose-dependent effects of heptanol between 0.1 and 2 mM [25, 26]. This is an extension of the previously work by examining the beat-to-beat variability in repolarization durations of monophasic action potential (MAP) time series data over 20-s periods. Typical examples of MAP waveforms, time series and histograms of action potential durations (APDs) at 90% repolarization for normokalaemia, hypokalemia alone or in the presence of 0.1 mM heptanol are shown in Fig. 1A–C, respectively. Time-domain analysis demonstrated a mean APD90 of 33.5 ± 3.7 ms (Fig. 2A), standard deviation (SD) of APDs of 0.63 ± 0.33 ms (Fig. 2B), coefficient of variation (CoV) of 1.9 ± 1.0% (Fig. 2C), and root mean square (RMS) of successive differences in APDs of 0.3 ± 0.1 ms (Fig. 2D). Hypokalemia prolonged APD90 to 51.2 ± 7.9 ms without significantly altering the remaining parameters (ANOVA, P > 0.05). After further treatment with heptanol, all of the above parameters remained unaltered (ANOVA, P > 0.05).
Action potential duration variability determined using frequency-domain methods
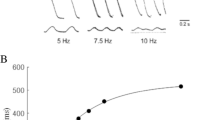
Fast Fourier Transform was used to generate frequency spectra, with examples obtained during normokalaemia, hypokalemia alone or in the presence of 0.1 mM heptanol are shown in Fig. 3A–C. Frequency-domain analysis revealed that the peaks for very low-, low- and high-frequency were 0.03 ± 0.01, 0.58 ± 0.46 and 2.30 ± 0.74 Hz, respectively (Fig. 4A–C). Their corresponding powers took values of 0.00 ± 0.01, 0.22 ± 0.28 and 0.23 ± 0.18 ms2, respectively (Fig. 4D–F). The low-frequency to high-frequency ratio was 0.95 ± 0.98 (Fig. 4G) and total power (in log units) was − 1.25 ± 1.11 (Fig. 4H). Their percentage powers were 1.2 ± 2.0, 38.3 ± 22.4 and 60.5 ± 23.5% (Fig. 4I–K). None of these parameters was altered by hypokalemia alone or in the presence of 0.1 mM heptanol (ANOVA, P > 0.05).
Action potential duration variability determined using nonlinear methods
Poincaré plots, which plotted APDn+1 against APDn, were generated (Fig. 5A–C). Ellipsoid shapes of the data points were observed for the different hearts studied. The SD1 (SD perpendicular to the line-of-identity), SD2 (SD along the line-of-identity) and SD2/SD1 ratio are shown in Fig. 6A–C, taking values of 0.19 ± 0.08, 0.87 ± 0.46 and 4.60 ± 1.07, respectively. Approximate and sample entropy were 0.49 ± 0.12 (Fig. 6D) and 0.64 ± 0.29, respectively (Fig. 6E). Detrended fluctuation analysis, which expressed the detrended fluctuations F(n) as a function of n in a logarithmic-logarithmic scale was conducted (Fig. 7A–C). This revealed short- and long-term fluctuation slopes of 1.62 ± 0.27 (Fig. 7D) and 0.60 ± 0.18 (Fig. 7E), respectively. Hypokalemia significantly decreased SD2/SD1 ratio to 3.1 ± 1.0, increased approximate and sample entropy to 0.68 ± 0.08 and 1.02 ± 0.33 and decreased short-term fluctuation slope to 1.23 ± 0.20 (ANOVA, P < 0.05). After treatment with heptanol, no further changes in the above parameters were observed (ANOVA, P > 0.05).
Discussion
In this study, we examined the effects of experimental hypokalemia modeling acquired long QT syndrome on beat-to-beat variability in APD using time-domain, frequency-domain and nonlinear analyses. Our main findings are that 1) increased arrhythmogenicity in hypokalemia was associated with prolonged APD, decreased SD2/SD1 ratio, increased approximate and sample entropy, and a decrease in short-term fluctuation slope; 2) heptanol exerted anti-arrhythmic effects despite leaving the hypokalemia-induced repolarization abnormalities unaltered.
Beat-to-beat variability in repolarization time-courses is a normal physiological phenomenon reflecting stochastic fluctuations in ion channel gating. Previous reports demonstrate that this variability is altered in pro-arrhythmic states. For example, higher degree of short-term variability determined using the Poincaré method was detected before the occurrence of torsade de pointes with reduced intercellular coupling in a canine model [14]. Secondly, computational modeling efforts complemented by experimental data suggested that higher variability was associated with pro-arrhythmic abnormalities using similar Poincaré plots [15]. Such a temporal variability in repolarization provide incremental value for arrhythmic risk stratification in human subjects with non-ischemic heart failure [27]. Recently, our group reported the use of time-domain, frequency-domain and fractal complexity analysis for assessing repolarization variability of action potential waveforms recorded from mouse hearts [28]. This was subsequently extended to demonstrations that nonlinear measures of repolarization variability, such as SD2/SD1, entropy, and fluctuation slope can predict ventricular arrhythmogenesis in mouse hearts using the gap junction and sodium channel blocker, heptanol [16]. The present work extends these findings by demonstrating that such measures of repolarization variability can similarly reveal re-entrant substrate in the context of acquired LQTS and represent biomarkers that can improve risk stratification. These findings have clinical implications given recent demonstrations of the association between increased beat-to-beat variability in the electrocardiographic T-wave with sudden cardiac death [29], but it remains to be elucidated whether the nonlinear measures would predict ventricular arrhythmias or sudden cardiac death in the clinical setting [30].
Previous studies have reported alterations in beat-to-beat repolarization variability with differing degrees of gap junction coupling using time-domain methods. Thus, single ventricular cardiomyocytes isolated from canine hearts showed a baseline level of APD variability [31]. When two cardiomyocytes were electrically coupled, this variability was attenuated [31]. These experimental findings were supported of those from computational modeling studies, reporting higher repolarization variability with lower level of intercellular coupling [32]. In the present work, APD variability was not significantly higher after introduction of heptanol. Some possible reasons could explain the present findings. For example, heptanol has multiple targets, such as potassium and calcium channels [13]. It was previously demonstrated that beat-to-beat variability is affected by not only the mean APD but also the pacing rate [33]. Therefore, pacing rate was fixed in this study to exclude its possible effects on variability. Future studies should systematically explore the relationship between pacing rate and different measures of variability. The anti-arrhythmic effects of heptanol can be attributed to its actions in prolonging the ventricular effective refractory period, which would lead to increase in the excitation wavelength [24].
Our findings in the mouse are in keeping with those from clinical studies. In heart failure patients, higher approximate entropy of the interval between Rpeak and Tpeak were predictive of appropriate ICD shocks and death [34]. Moreover, in patients who have implantable cardioverter-defibrillator for primary prevention, high entropy of QT intervals also predicted ventricular arrhythmogenesis and mortality [35]. This study extends these findings by quantifying entropy using action potential time series data recorded from isolated hearts that are free from autonomic influence and associated increased entropy with ventricular arrhythmogenesis under hypokalaemic conditions. Interestingly, our study found that it was possible to reduce arrhythmogenicity in the presence of high variability in beat-to-beat repolarization. Instead, the anti-arrhythmic effects are instead attributed to increases in tissue refractoriness, which was initially reduced by hypokalemia [24]. These findings are in keeping with known effects of different anti-arrhythmic agents. For example, class III and class IV anti-arrhythmic agents inhibit potassium and calcium channels, respectively, yet they increase beat-to-beat variability for two reasons. Firstly, the inward calcium current has the highest amplitude at the beginning of the plateau phase of cardiac repolarization, and this is a powerful modulator of subsequent potassium channel activation [36]. Secondly, the membrane resistance is high during the late phase of repolarization [31], and any small increase in the net inward current (e.g., produced by potassium channel block) can lead to larger variation in APD [37, 38]. Together, these findings would suggest multiple interacting mechanisms that are important determinants of arrhythmogenesis. The implications are that patients who are suffering from hypokalaemia at an inpatient setting could benefit from not only continuous monitoring but its real-time quantification of repolarization variability and the QT intervals. This could theoretically provide warning messages for patients at immediate risks of developing ventricular arrhythmias [39]. A limitation is that the possible modifying effects of age on hypokalaemia-related electrophysiology and arrhythmogenicity were not explored. Given that there is an age-dependent increase in QT intervals [40], whether increasing age would interact with hypokalaemia to exacerbate arrhythmogenic or electrophysiological abnormalities remain to be elucidated. Finally, wild-type mice from the 129 genetic background were used. Previously studies have reported the differing effects of genetic background on electrophysiology [41, 42]. Future studies should therefore be conducted to explore the effects of hypokalaemia in different genetic strains.
Conclusions
Reduced SD2/SD1 and increased entropy and decreased short-term fluctuation slope may reflect arrhythmic risk in hypokalaemia. Heptanol exerts anti-arrhythmic effects without significantly influencing repolarization variability.
Availability of data and materials
Raw data are available from the corresponding author without restriction.
Abbreviations
- APD:
-
Action potential duration
- ICD:
-
Implantable cardioverter-defibrillator
- LQTS:
-
Long QT syndrome
- VT:
-
Ventricular tachycardia
References
Rastegar A, Soleimani M. Hypokalaemia and hyperkalaemia. Postgrad Med J. 2001;77:759–64.
Soar J, Deakin CD, Nolan JP, Abbas G, Alfonzo A, Handley AJ, Lockey D, Perkins GD, Thies K and Council. ER. European Resuscitation Council guidelines for resuscitation 2005. Section 7. Cardiac arrest in special circumstances. Resuscitation. 2005;67:S135–S170.
Johansson BW, Dziamski R. Malignant arrhythmias in acute myocardial infarction. Relationship to serum potassium and effect of selective and non-selective beta-blockade. Drugs. 1984;28:77–85.
Solomon RJ, Cole AG. Importance of potassium in patients with acute myocardial infarction. Acta Med Scand Suppl. 1981;647:87–93.
Clausen TG, Brocks K, Ibsen H. Hypokalemia and ventricular arrhythmias in acute myocardial infarction. Acta Med Scand. 1988;224:531–7.
Tse G, Li KHC, Cheung CKY, Letsas KP, Bhardwaj A, Sawant AC, Liu T, Yan GX, Zhang H, Jeevaratnam K, Sayed N, Cheng SH, Wong WT. Arrhythmogenic mechanisms in hypokalaemia: insights from pre-clinical models. Front Cardiovasc Med. 2021;8: 620539.
Osadchii OE. Mechanisms of hypokalemia-induced ventricular arrhythmogenicity. Fundam Clin Pharmacol. 2010;24:547–59.
Weiss JN, Qu Z, Shivkumar K. Electrophysiology of hypokalemia and hyperkalemia. Circ Arrhythm Electrophysiol. 2017;10.
Gurung B, Tse G, Keung W, Li RA, Wong WT. Arrhythmic risk assessment of hypokalaemia using human pluripotent stem cell-derived cardiac anisotropic sheets. Front Cell Dev Biol. 2021;9: 681665.
Tse G, Wong ST, Tse V, Yeo JM. Restitution analysis of alternans using dynamic pacing and its comparison with S1S2 restitution in heptanol-treated, hypokalaemic Langendorff-perfused mouse hearts. Biomed Rep. 2016;4:673–80.
Osadchii OE. Effects of ventricular pacing protocol on electrical restitution assessments in guinea-pig heart. Exp Physiol. 2012;97:807–21.
Couderc JP. Cardiac regulation and electrocardiographic factors contributing to the measurement of repolarization variability. J Electrocardiol. 2009;42:494–9.
Nanasi PP, Magyar J, Varro A, Ordog B. Beat-to-beat variability of cardiac action potential duration: underlying mechanism and clinical implications. Can J Physiol Pharmacol. 2017;95:1230–5.
Thomsen MB, Verduyn SC, Stengl M, Beekman JD, de Pater G, van Opstal J, Volders PG, Vos MA. Increased short-term variability of repolarization predicts d-sotalol-induced torsades de pointes in dogs. Circulation. 2004;110:2453–9.
Pueyo E, Corrias A, Virag L, Jost N, Szel T, Varro A, Szentandrassy N, Nanasi PP, Burrage K, Rodriguez B. A multiscale investigation of repolarization variability and its role in cardiac arrhythmogenesis. Biophys J. 2011;101:2892–902.
Tse G, Hao G, Lee S, Zhou J, Zhang Q, Du Y, Liu T, Cheng SH, Wong WT. Measures of repolarization variability predict ventricular arrhythmogenesis in heptanol-treated Langendorff-perfused mouse hearts. Curr Res Physiol. 2021;4:125–34.
Tse G, Liu T, Li G, Keung W, Yeo JM, Fiona Chan YW, Yan BP, Chan YS, Wong SH, Li RA, Zhao J, Wu WKK, Wong WT. Effects of pharmacological gap junction and sodium channel blockade on S1S2 restitution properties in Langendorff-perfused mouse hearts. Oncotarget. 2017;8:85341–52.
Tse G, Tse V, Yeo JM, Sun B. Atrial anti-arrhythmic effects of heptanol in Langendorff-perfused mouse hearts. PLoS ONE. 2016;11: e0148858.
Yeo JM, Tse V, Kung J, Lin HY, Lee YT, Kwan J, Yan BP, Tse G. Isolated heart models for studying cardiac electrophysiology: a historical perspective and recent advances. J Basic Clin Physiol Pharmacol. 2017;28:191–200.
Knollmann BC, Katchman AN, Franz MR. Monophasic action potential recordings from intact mouse heart: validation, regional heterogeneity, and relation to refractoriness. J Cardiovasc Electrophysiol. 2001;12:1286–94.
Tse G, Wong ST, Tse V, Yeo JM. Monophasic action potential recordings: which is the recording electrode? J Basic Clin Physiol Pharmacol. 2016.
Gussak I, Chaitman BR, Kopecky SL, Nerbonne JM. Rapid ventricular repolarization in rodents: electrocardiographic manifestations, molecular mechanisms, and clinical insights. J Electrocardiol. 2000;33:159–70.
Fabritz L, Kirchhof P, Franz MR, Eckardt L, Mönnig G, Milberg P, Breithardt G, Haverkamp W. Prolonged action potential durations, increased dispersion of repolarization, and polymorphic ventricular tachycardia in a mouse model of proarrhythmia. Basic Res Cardiol. 2003;98:25–32.
Tse G, Tse V, Yeo JM. Ventricular anti-arrhythmic effects of heptanol in hypokalaemic, Langendorff-perfused mouse hearts. Biomed Rep. 2016;4:313–24.
Tse G, Hothi SS, Grace AA, Huang CL. Ventricular arrhythmogenesis following slowed conduction in heptanol-treated, Langendorff-perfused mouse hearts. J Physiol Sci. 2012;62:79–92.
Tse G, Yeo JM, Tse V, Kwan J, Sun B. Gap junction inhibition by heptanol increases ventricular arrhythmogenicity by reducing conduction velocity without affecting repolarization properties or myocardial refractoriness in Langendorff-perfused mouse hearts. Mol Med Rep. 2016;14:4069–74.
Hinterseer M, Beckmann BM, Thomsen MB, Pfeufer A, Ulbrich M, Sinner MF, Perz S, Wichmann HE, Lengyel C, Schimpf R, Maier SK, Varro A, Vos MA, Steinbeck G, Kaab S. Usefulness of short-term variability of QT intervals as a predictor for electrical remodeling and proarrhythmia in patients with nonischemic heart failure. Am J Cardiol. 2010;106:216–20.
Tse G, Du Y, Hao G, Li KHC, Chan FYW, Liu T, Li G, Bazoukis G, Letsas KP, Wu WKK, Cheng SH, Wong WT. Quantification of beat-to-beat variability of action potential durations in Langendorff-perfused mouse hearts. Front Physiol. 2018;9:1578.
Hekkanen JJ, Kentta TV, Haukilahti MAE, Rahola JT, Holmstrom L, Vahatalo J, Tulppo MP, Kiviniemi AM, Pakanen L, Ukkola OH, Junttila MJ, Huikuri HV, Perkiomaki JS. Increased beat-to-beat variability of T-wave heterogeneity measured from standard 12-lead electrocardiogram is associated with sudden cardiac death: a case-control study. Front Physiol. 2020;11:1045.
Varkevisser R, Wijers SC, van der Heyden MA, Beekman JD, Meine M, Vos MA. Beat-to-beat variability of repolarization as a new biomarker for proarrhythmia in vivo. Heart Rhythm. 2012;9:1718–26.
Zaniboni M, Pollard AE, Yang L, Spitzer KW. Beat-to-beat repolarization variability in ventricular myocytes and its suppression by electrical coupling. Am J Physiol Heart Circ Physiol. 2000;278:H677–87.
Heijman J, Zaza A, Johnson DM, Rudy Y, Peeters RL, Volders PG, Westra RL. Determinants of beat-to-beat variability of repolarization duration in the canine ventricular myocyte: a computational analysis. PLoS Comput Biol. 2013;9: e1003202.
Zaniboni M, Cacciani F, Salvarani N. Temporal variability of repolarization in rat ventricular myocytes paced with time-varying frequencies. Exp Physiol. 2007;92:859–69.
Perkiomaki JS, Couderc JP, Daubert JP, Zareba W. Temporal complexity of repolarization and mortality in patients with implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2003;26:1931–6.
DeMazumder D, Limpitikul WB, Dorante M, Dey S, Mukhopadhyay B, Zhang Y, Moorman JR, Cheng A, Berger RD, Guallar E, Jones SR, Tomaselli GF. Entropy of cardiac repolarization predicts ventricular arrhythmias and mortality in patients receiving an implantable cardioverter-defibrillator for primary prevention of sudden death. Europace. 2016;18:1818–28.
Banyasz T, Fulop L, Magyar J, Szentandrassy N, Varro A, Nanasi PP. Endocardial versus epicardial differences in L-type calcium current in canine ventricular myocytes studied by action potential voltage clamp. Cardiovasc Res. 2003;58:66–75.
Barandi L, Virag L, Jost N, Horvath Z, Koncz I, Papp R, Harmati G, Horvath B, Szentandrassy N, Banyasz T, Magyar J, Zaza A, Varro A, Nanasi PP. Reverse rate-dependent changes are determined by baseline action potential duration in mammalian and human ventricular preparations. Basic Res Cardiol. 2010;105:315–23.
Banyasz T, Horvath B, Virag L, Barandi L, Szentandrassy N, Harmati G, Magyar J, Marangoni S, Zaza A, Varro A, Nanasi PP. Reverse rate dependency is an intrinsic property of canine cardiac preparations. Cardiovasc Res. 2009;84:237–44.
Walia R, Prabhakaran N, Kodliwadmath A, Singh OBC, Mahala P, Kaeley N. Seven day continuous ambulatory electrocardiographic telemetric study with pocket electrocardiographic recording device for detecting hydroxychloroquine induced arrhythmias. J Fam Med Prim Care 2022;11.
Rabkin SW, Cheng XJ, Thompson DJ. Detailed analysis of the impact of age on the QT interval. J Geriatr Cardiol. 2016;13:740–8.
Obergassel J, O’Reilly M, Sommerfeld LC, Kabir SN, O’Shea C, Syeda F, Eckardt L, Kirchhof P, Fabritz L. Effects of genetic background, sex, and age on murine atrial electrophysiology. Europace. 2021;23:958–69.
Jelinek M, Wallach C, Ehmke H, Schwoerer AP. Genetic background dominates the susceptibility to ventricular arrhythmias in a murine model of beta-adrenergic stimulation. Sci Rep. 2018;8:2312.
Acknowledgments
None.
Funding
GT received research funding from the BBSRC from the UK for this research.
Author information
Authors and Affiliations
Contributions
GT contributed to data acquisition, statistical analysis, manuscript drafting, critical revision of manuscript. JZ contributed to statistical analysis, data interpretation, critical revision of manuscript. XD contributed to statistical analysis, data interpretation, manuscript drafting, critical revision of manuscript. GH contributed to statistical analysis, data interpretation, manuscript drafting, critical revision of manuscript. SL contributed to statistical analysis, data interpretation, manuscript drafting, critical revision of manuscript. KSKL contributed to statistical analysis, data interpretation, manuscript drafting, critical revision of manuscript. TL contributed to data interpretation, critical revision of manuscript, study supervision. YD contributed to data interpretation, critical revision of manuscript, study supervision. SHC contributed to data interpretation, critical revision of manuscript, study supervision. WTW contributed to data interpretation, critical revision of manuscript, study supervision.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the University’s Animal Ethics Committee.
Consent for publication
All authors consent to publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tse, G., Zhou, J., Dong, X. et al. Nonlinear analysis of beat-to-beat variability of action potential time series data identifies dynamic re-entrant substrates in a hypokalaemic mouse model of acquired long QT syndrome. Int J Arrhythm 24, 2 (2023). https://doi.org/10.1186/s42444-023-00084-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42444-023-00084-4