Abstract
Background
Implantable loop recorders (ILRs) can provide an enhanced possibility to detect atrial fibrillation (AF), but the accuracy, especially the positive predictive value (PPV), is controversial. This study aimed to evaluate the accuracy of ILRs for detecting AF through a comparison with Holter.
Method and results
Thirteen patients who underwent AF ablation were enrolled. ILRs were implanted in all patients, who were scheduled to have Holter monitorings after the procedure. The incidence of AF was compared between the two modalities and analyzed for any correlations. A total of 51 Holters (67,985.5 min) and concomitant ILRs were available for the comparison. The judgment of the presence of AF did not perfectly correlate between the ILR and Holter (Kappa = 0.866, P < 0.001). In the ILR data, the sensitivity of detecting AF on the Holter was 81.6% (95% confidence interval [CI] 0.812–0.820; P < 0.001). The specificity was 99.9% (95% CI 0.998–0.999; P < 0.001). When the ILR detected AF, the PPV was 99.5% (95% CI 0.994–0.995), but the ILR did not detect AF, and the negative predictive value was 94.2% (95% CI 0.941–0.944). A separate analysis of AF/atrial tachycardia (AT) showed that the AT detection rate of the ILR was 2.3%.
Conclusion
The ILR had a low false positive value and high PPV for AF events. However, it was limited in identifying AT.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most common arrhythmia, and the incidence increases exponentially with age [1]. AF is associated with an increased number of thromboembolic events, including strokes. Furthermore, it can lead to heart failure (HF) and results in an increased number of hospitalizations [2, 3]. Combined with lost productivity, the economic burden of the AF treatment cost is more than $26 billion a year [4]. The adverse events associated with AF are mainly correlated to the episode duration, frequency, and arrhythmia burden [5, 6]. Earlier detection of AF would enable the use of anticoagulation therapy known to mitigate the risk of a stroke and other thromboembolic complications [7,8,9,10,11,12,13]. However, since AF is often an asymptomatic episode and the initial presentation being either a thromboembolic event or HF, the diagnosis through observation of symptoms is bound to have a low sensitivity and specificity [14].
In patients with suspected or already diagnosed AF, it is very important to correctly detect the AF occurrence by ECG monitoring tools. A previous diagnosis of AF is usually based on the patient’s symptoms and clinical signs and is confirmed by external ECG monitoring tools. Intermittent and symptom-based monitoring is highly inaccurate for identifying patients with any or long durations of AF and for assessing the AF burden [15]. Long-term ECG monitoring with an implantable loop recorder (ILR) enhances the accuracy of identifying high-risk populations of patients suspected of having AF and increases the ability to characterize the AF burden and AF density. The improved detection of AF occurrence and AF characterization compared to intermittent ECG monitoring could significantly impact the clinical treatment decisions [16]. However, many studies on AF detection using ILRs have shown a lower-than-expected positive predictive value (PPV) due to a higher rate of false positive episodes [22,23,24,25].
The purpose of this study was to evaluate the AF detection performance of ILRs by comparing the ILR-based AF detection data with the external Holter ECG monitoring recordings during the blanking period after radiofrequency catheter ablation (RFCA) of AF, which has a high incidence of atrial tachyarrhythmias. Holter monitoring serves as the standard for determining the presence or absence of AF.
Methods
Study design
Between August 2016 and February 2017, 13 patients having undergone RFCA of AF were included from a single institution. The patients had scheduled 24-hour Holter monitorings at 48 h, and 4, 8, and 12 weeks after the procedure for detecting the AF recurrences. An ILR (Reveal XT™, Medtronic) was implanted in all patients immediately after the AF RFCA in the “AF only” mode on. The nominal settings for “AF only” detection ensure an optimal performance of AF detection in most patients. The clocks were synchronized with the Holter monitoring so that the electrocardiographic events could be simultaneously compared by the two systems. We interpreted all of the electrocardiograms stored in the Holter recordings of all patients involved in the study. The continuous Holter ECG data were interpreted to find and annotate the presence of any AF or other atrial tachyarrhythmias. The arrhythmic events detected by the ILR at the time of the Holter monitoring were checked via the stored EGMs or event log. The correlation of the arrhythmic events between the two systems was analyzed. The study was approved by the Keimyung University Dongsan Hospital Institutional Review Board.
Implanted device characteristics and implantation
The ILR was equipped with an AF detection algorithm that was designed to detect the presence of AF episodes and to quantify the AF burden. Physiological sinus rhythm and AF each have a unique R–R interval pattern. The dedicated AF detection algorithm uses various regularity and coherence factors of the R–R intervals to identify and classify the patterns of the ventricular conduction. The R–R intervals are analyzed within each 2-min periods of time, and the difference in the duration between consecutive R–R intervals (ΔR–R) is calculated. Subsequently, the variability of these ΔR–R intervals is calculated, similar to constructing a Lorenz plot. When the R–R intervals within the 2-min interval show a certain pattern of uncorrelated irregularity or regularly irregularity, and a regular ventricular response, the heart rhythm in this interval is classified as AF. If the R–R intervals are regular with some sinus node modulations, the interval is defined as normal sinus rhythm [17].
The Reveal XT™, Medtronic ILR can store up to 49.5 min of recorded ECGs, which are allocated to 27 min of automatically activated events and 22.5 min of patient-activated events. In addition, the ILR has an episode log that can catalog 30 automatically detected AF episodes and up to ten patient-activated episodes. When the memory is full, an additional episode will overwrite the oldest stored episode [18]. All ILRs were implanted subcutaneously under local anesthesia immediately after the RFCA, and the atrial arrhythmic episode detection parameters remained in the nominal “AF only” settings. The nominal settings for “AF only” detection ensure the optimal performance of the AF detection in most patients [18]. The sensing threshold of R wave amplitude at ILR implantation, which ensures the adequate implantation, is at least 0.2 millivolts (mV). All data in this report were based on the current detection algorithm.
Holter recordings and episode definitions
Two cardiologists interpreted all of the electrocardiogram data stored in the Holter devices from all patients. The recorded electrograms from the Holter monitoring were printed in a 30-s segment format and analyzed manually. The presence of AF or atrial tachycardia (AT) lasting more than 2 min was annotated. Since it may recur as AT rather than AF after RFCA, an obvious AT was read separately and stated separately. The segments with non-interpretable Holter ECGs due to noise or artifact were excluded. The reviewers defined AF as irregularly irregular R wave to R wave intervals, with no visible P waves. Further, AT was defined as more than 100 beats per minute with a non-sinus origin P wave running regardless of the regularity of the R–R interval. Because the ILR algorithm classifies the rhythm for each subsequent time interval of 2 min, only episodes with a duration of at least 2 min were included in the analysis.
Statistical analysis
Each event from the ILR could be classified as true positive (TP), true negative (TN), false positive (FP), or false negative (FN) episodes. A Holter AF episode coincident with an ILR AF episode was classified as a TP, while a Holter recording with no AF period coincident with the ILR was classified as a TN. A Holter AF episode without a concomitant ILR AF episode was classified as an FN, and conversely, an ILR AF event occurring without a concomitant Holter AF episode was classified as an FP. Through the time sum of each of the four classifications presented, we analyzed the sensitivity and specificity of the ILR. The sensitivity was calculated by calculating the positive result ratios between the ILR and Holter. The specificity was calculated by calculating the negative result ratios between the ILR and Holter. The McNemar and binomial testing method was used to compare the sensitivity and specificity. The PPV and negative predictive value (NPV) were also calculated (Fig. 1). The consistency between the ILR results and Holter results was calculated by a Kappa test. All statistical analyses were performed using the SPSS software version 20.0 for Windows (SPSS Inc, Chicago, IL, USA).
Classification of AF episodes. The definitions of the sensitivity, specificity, positive predictive value, and negative predictive value were based on the sum of the episodes. AF atrial fibrillation, ILR implantable loop recorder, TP true positive, FP false positive; TN true negative, FN false negative
Results
Recording event and AF detection
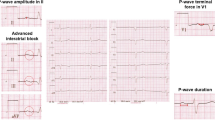
The study enrolled a total of 13 patients. The mean age of the patients was 69 ± 5.6 years, and 53.8% were male. Six of the 13 patients had paroxysmal AF and the rest persistent AF. Four Holter monitorings were conducted in most enrolled patients, and in only one patient was one set of Holter data lost. A total of 51 Holter recordings and concomitant ILR recordings were available for the comparison. The sensing threshold of R wave amplitude at ILR implantation was 0.734 ± 0.332 mV. A total of 67,985.5 min of valid recordings from 13 patients were analyzed, yielding a mean valid recording time of 5230 min per patient. AF or AT recurrence was observed in seven of the 13 patients, and the number of event episodes was 24 of AF and nine of AT events, yielding a total of 17,249 min of true AF episodes of ≥ 2 min and 2979 min of true AT episodes of ≥ 2 min. On the other hand, the period of time that the Holter monitoring identified an event as true AF but the ILR did not was 3166.5 min. Figure 2 presents some examples of ECG that was judged to be an AT or AF by the Holter, but was not detected as any atrial tachyarrhythmia event on the ILR. Both the Holter monitoring and ILR recordings were interpreted as AF in 14,082.5 min. In fact, during the period when there was no AF in the Holter monitoring, the period that the ILR judged there not to be AF was 50,662 min. On the other hand, it took only 74.5 min for the ILR to incorrectly determine when there was no AF on Holter monitoring (Table 1).
Example of AF or AT surface ECGs recorded by the Holter. a–d A surface ECG that was judged to be an AT or AF by the Holter, but was not detected as any atrial tachyarrhythmia event on the ILR. e, f A surface ECG that was considered to be an AT on the Holter, but was read as AF by the ILR. AF atrial fibrillation, AT atrial tachycardia, ILR implantable loop recorder
Episode detection performance of ILRs
In the ILR data, the sensitivity for detecting AF on the Holter was 81.6% (95% confidence interval [CI] 0.812–0.820; P < 0.001). The specificity was 99.9% (95% CI 0.998–0.999; P < 0.001). The PPV of the ILR was 99.5% (95% CI 0.994–0.995), but the NPV was 94.2% (95% CI 0.941–0.944). The results of the ILR and Holter monitoring were not perfectly correlated regarding their judgment about the presence of AF (Kappa = 0.866, P < 0.001). During the 50,736.5 min of no AF on the Holter recordings, the recurrence of AT accounted for 2979 min, while the remaining 47,757.5 min were a pure atrial tachyarrhythmia free state. Of the 2979 min of all AT recorded on the Holter, the ILR detected 70 min as AF during that period (detection rate = 2.3%). Further, among the other 2909 min of AT, the ILR did not detect the AT in the remaining 2909 min as an event at all (Table 1).
Discussion
The main findings of this study were that the sensitivity of the ILR in detecting AF was 81.6% for the Medtronic Reveal XT™. However, the specificity, PPV, and NPV were excellent. The ability to detect AT was not promising.
The current classification of the pattern of AF as paroxysmal, persistent, and long-standing persistent AF does not reflect well the actual time persistence of AF [19, 20]. The correct characterization of patients with AF based on the burden and density of AF will result in a decreased patient variability, reduced potential study biases, and more consistent clinical results [16]. In addition, the current guidelines urge investigators to clarify the duration of time that patients have been in continuous AF as well as the overall AF burden. This information can only be obtained through an implantable device [21]. Long-term monitoring using an ILR will be able to determine the AF patterns, number of episodes, AF burden, and AF density as well as provide an early diagnosis of AF. This can have a significant impact on the clinical treatment decisions, such as the need for ongoing oral anticoagulation treatment to prevent strokes [16].
There have been many studies that have evaluated the AF detection performance through long-term monitoring using ILRs. As in this study, most of the studies were conducted using external Holter monitoring as a criterion standard for the presence or absence of AF. Biotronik ILRs have evaluated the performance of AF algorithms through two separate studies [22, 23]. As most of the AF episodes confirmed on the Holter were detected on the ILR, they showed a high sensitivity of more than 90%. Both studies, however, showed that more than half of all AF episodes recorded on the ILR were false positives episodes, which resulted in a low positive predictive value. The DETECT-AF study evaluated the performance of the St. Jude Medical Confirm DM2102 ILR using the 48-hour Holter recording as a criterion standard [24]. There were no instances where the patients had an AF episode that was recorded by the Holter but missed by the ILR. In contrast, there were several patients in whom the ILR detected AF but the Holter showed no arrhythmia. The PPV for AF detection was 64%. There was also a study comparing the sensitivity and specificity of the ILR arrhythmia detection with a dual-chamber pacemaker [25]. Paroxysmal AF patients were randomized to be assigned either a dual-chamber pacemaker or Reveal XT ILR, and all patients also received an external Holter ECG recording for at least 7 days. The PPV of the AF episodes detected by the ILR was significantly lower than the events detected by the pacemaker (55% vs. 97%, respectively; P < 0.001). In comparison with the external Holter monitor records, both the ILR and pacemaker had an excellent NPV. However, the PPV for AF of the ILR was much lower than that of the pacemaker. What the aforementioned studies have in common is that the ILR showed a high sensitivity for AF detection while also a reduced PPV due to high false positive events. The propensity of false positive episodes is the major limitation in tracking the AF burden using an ILR. However, in this study, when the ILR ECG data alone were analyzed, 14,157 min of AF episodes were detected in the patients. Only 74.5 min of those episodes (0.53%) were “false” AF and the false positive rate of the AF detection of the ILR was less than 0.01% (Table 1). In addition, of those false positive events, 70 min were AT. Perhaps, a somewhat irregular AT rhythm was classified as AF (Fig. 2). According to this study’s results, the AF episodes detected by the ILR were considered to be quite reliable and helpful in measuring the AF burden, and that differed from the previous ILR performance in the AF detection studies. It is not clear why the results of the previous studies and the results of this study differed. However, one characteristic of this study was that the episodes had a rather long continuity. Of the total 51 Holter events, 44 Holter events were either entirely AF or entirely no AF for each Holter monitoring period. In addition, a total of 24 AF episodes were observed in the Holter data, only seven of which were less than 10 min, while the mean duration of the remaining AF episodes was 1008 ± 483 min. The performance of the ILR improved as the duration of the AF episode improved. The “gross” episode PPV for AF episodes of > 10–20 min was > 90% [24].
The clinical interrelationship between AF and atrial flutter (AFL) has long been appreciated. The support of this concept comes from the report by Ellis et al., in which they found that of 363 patients who presented with only cavotricuspid isthmus (CTI)-dependent AFL and who underwent a CTI ablation, the long-term follow-up demonstrated newly recognized AF in 82% [26]. In addition, class IC and IA antiarrhythmic drugs and amiodarone used to suppress AF commonly promote sustained AFL [27, 28]. Further, also, some patients develop recurrences of an organized AT rather than a typical AF after RFCA of AF [29, 30]. In addition, the recurrence of AF after AF ablation as defined in the guidelines is an atrial tachyarrhythmia, including AFL and AT that last for more than 30 s [21]. However, as in this study, few AT events were detected when monitored with nominal settings that showed an optimal performance for AF detection. Therefore, the ILR seems to have a limitation in evaluating the outcome of AF ablation. By design, all ILRs use an R–R variability-based detection algorithm, which is an unreliable method for the detection of an AT. The AT detection algorithm generates so many false positive episodes (most commonly due to sinus tachycardia) that we no longer program the device to detect AT episodes [16]. Therefore, for the ILR, it will be necessary to develop algorithms that can find atrial tachyarrhythmias, including AT. One approach to solving this problem is to identify periods when there is a large discrepancy between the patient’s heart rate and the activity level using the accelerometer incorporated in the device and to determine the exact AT [16].
Study limitations
There were several limitations to this study. It was based on a small number of patients and events, and only one kind of ILR was used for the analysis. The ILR detection performance was evaluated by dividing AF and AT, but it was sometimes not able to correctly distinguish that. Some episodes were spontaneously transitioning from AF to AT or AT to AF, making it difficult to classify them separately. Therefore, only the rhythms, which were determined to be a clear AT, were classified as AT for the final analysis. It was very difficult to distinguish AF from AT through the surface ECG recorded on the Holter devices. In fact, many AF rhythms tended to interchange into a very natural flow, so that clearly distinguishing between those two rhythms would not have had much meaning. The ILR was also considered as a limitation. Unlike the XPECT trial [18], this study was conducted without a stabilization phase for 4–6 weeks after the ILR was inserted, which could also have been considered as a difference from the previous studies and a limitation. However, if there is any controversy over the reliability of the data during the stabilization period, it is also believed to be a limitation of the ILR device.
Conclusion
The ILR can be used as a method to measure the AF burden with low false positive and high PPV values. However, it seems to be insufficient to detect the recurrence of atrial tachyarrhythmias after AF ablation that often recur as an AT. It seems to be necessary to develop more sophisticated algorithms to detect ATs for a better usage of the ILR in the management of patients with AF.
Availability of data and materials
Not applicable.
Abbreviations
- AF:
-
Atrial fibrillation
- AFL:
-
Atrial flutter
- AT:
-
Atrial tachycardia
- mV:
-
Millivolt
- CI:
-
Confidence interval
- CTI:
-
Cavotricuspid isthmus
- FN:
-
False negative
- FP:
-
False positive
- HF:
-
Heart failure
- ILRs:
-
Implantable loop recorders
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- RFCA:
-
Radiofrequency catheter ablation
- TN:
-
True negative
- TP:
-
True positive
References
Wolf PA, Benjamin EJ, Belanger AJ, Kannel WB, Levy D, D’Agostino RB. Secular trends in the prevalence of atrial fibrillation: the Framingham study. Am Heart J. 1996;131:790–5.
Flaker GC, Belew K, Beckman K, Vidaillet H, Kron J, Safford R, et al. Asymptomatic atrial fibrillation: demographic features and prognostic information from the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study. Am Heart J. 2005;149:657–63.
Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2011;57:e101–98.
Kim MH, Johnston SS, Chu BC, Dalal MR, Schulman KL. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4:313–20.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–67.
Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–5.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130:e199–267.
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease, Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–236.
Santangeli P, Di Biase L, Bai R, Mohanty S, Pump A, Cereceda Brantes M, et al. Atrial fibrillation and the risk of incident dementia: a meta-analysis. Heart Rhythm. 2012;9(11):1761–8.
Kalantarian S, Stern TA, Mansour M, Ruskin JN. Cognitive impairment associated with atrial fibrillation: a meta-analysis. Ann Intern Med. 2013;158:338–46.
Bansal N, Fan D, Hsu CY, Ordonez JD, Marcus GM, Go AS. Incident atrial fibrillation and risk of end-stage renal disease in adults with chronic kidney disease. Circulation. 2013;127(5):569–74.
Soliman EZ, Safford MM, Muntner P, Khodneva Y, Dawood FZ, Zakai NA, et al. Atrial fibrillation and the risk of myocardial infarction. JAMA Intern Med. 2014;174(1):107–14.
Dukes JW, Marcus GM. Atrial fibrillation begets myocardial infarction. JAMA Intern Med. 2014;174(1):5–7.
Strickberger SA, Ip J, Saksena S, Curry K, Bahnson TD, Ziegler PD. Relationship between atrial tachyarrhythmias and symptoms. Heart Rhythm. 2005;2:125–31.
Ziegler PD, Koehler JL, Mehra R. Comparison of continuous versus intermittent monitoring of atrial arrhythmias. Heart Rhythm. 2006;3:1445–52.
Lee R, Mittal S. Utility and limitations of long-term monitoring of atrial fibrillation using an implantable loop recorder. Heart Rhythm. 2018;15(2):287–95.
Sarkar S, Ritscher D, Mehra R. A detector for a chronic implantable atrial tachyarrhythmia monitor. IEEE Trans Biomed Eng. 2008;55:1219–24.
Hindricks G, Pokushalov E, Urban L, et al. Performance of a new leadless implantable cardiac monitor in detecting and quantifying atrial fibrillation results of the XPECT trial. Circ Arrhythm Electrophysiol. 2010;3:141–7.
Charitos EI, Purerfellner H, Glotzer TV, Ziegler PD. Clinical classifications of atrial fibrillation poorly reflect its temporal persistence: insights from 1,195 patients continuously monitored with implantable devices. J Am Coll Cardiol. 2014;63:2840–8.
Mittal S. Differentiating paroxysmal from persistent atrial fibrillation: long-term ECG monitoring is mightier than the clinician. J Am Coll Cardiol. 2014;63:2849–50.
Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14:e275–444.
Lauschke J, Busch M, Haverkamp W, Bulava A, Schneider R, Andresen D, et al. New implantable cardiac monitor with three-lead ECG and active noise detection [published online ahead of print October 28, 2016]. Herz. 2017;42(6):585–92.
Ciconte G, Saviano M, Gianelli L, Calovic Z, Baldi M, Ciaccio C, et al. Atrial fibrillation detection using a novel three-vector cardiac implantable monitor: the atrial fibrillation detect study. Europace. 2017;19:1101–8.
Nolker G, Mayer J, Boldt LH, Seidl K, Van Driel V, Massa T, et al. Performance of an implantable cardiac monitor to detect atrial fibrillation: results of the DETECT AF study. J Cardiovasc Electrophysiol. 2016;27:1403–10.
Podd SJ, Sugihara C, Furniss SS, Sulke N. Are implantable cardiac monitors the “gold standard” for atrial fibrillation detection? A prospective randomized trial comparing atrial fibrillation monitoring using implantable cardiac monitors and DDDRP permanent pacemakers in post fibrillation ablation patients. Europace. 2016;18:1000–5.
Ellis K, Wazni O, Marrouche N, Martin D, Gillinov M, McCarthy P, et al. Incidence of atrial fibrillation post-cavotricuspid isthmus ablation in patients with typical atrial flutter: left-atrial size as an independent predictor of atrial fibrillation recurrence. J Cardiovasc Electrophysiol. 2007;18:799–802.
Waldo AL. Atrial flutter: from mechanism to treatment. In: Camm AJ, editor. Clinical approaches to tachyarrhythmias, vol. 14. Armonk: Futura Publishing Co.; 2001. p. 1–64.
Huang DT, Monahan KM, Zimetbaum P, Papageorgiou P, Epstein LM, Josephson ME. Hybrid pharmacologic and ablative therapy: a novel and effective approach for the management of atrial fibrillation. J Cardiovasc Electrophysiol. 1998;9:462–7.
Patel AM, d’Avila A, Neuzil P, Kim SJ, Mela T, Singh JP, et al. Atrial tachycardia after ablation of persistent atrial fibrillation: identification of the critical isthmus with a combination of multielectrode activation mapping and targeted entrainment mapping. Circ Arrhythm Electrophysiol. 2008;1:14–22.
Veenhuyzen GD, Knecht S, O’Neill MD, Phil D, Wright M, Nault I, et al. Atrial tachycardias encountered during and after catheter ablation for atrial fibrillation: part I: classification, incidence, management. Pacing Clin Electrophysiol. 2009;32:393–8.
Acknowledgements
We thank Mr. John Martin for his linguistic assistance.
Funding
The research was supported by the Ministry of Science, ICT and Future Planning Through the Development for IT•SW industrial convergence original technology (ID: R0101-15-0147).
Author information
Authors and Affiliations
Contributions
All coauthors have read the final version of the manuscript and approved its submission to your esteemed journal. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was approved by the Keimyung University Dongsan Hospital Institutional Review Board.
Consent for publication
The paper has not been published and is not being considered for publication elsewhere in whole or in part in any language.
Competing interests
None of the authors has any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cho, H.J., Lee, C.H., Hwang, J. et al. Accuracy of implantable loop recorders for detecting atrial tachyarrhythmias after atrial fibrillation catheter ablation. Int J Arrhythm 21, 6 (2020). https://doi.org/10.1186/s42444-020-00013-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42444-020-00013-9