Abstract
Background
The extra-musculoskeletal manifestations (EMMs) such as recurrent acute anterior uveitis (rAAU), psoriasis (Ps), and inflammatory bowel disease (IBD), are related to the Spondyloarthritis (SpA), as well as they are associated with disease activity and poor prognosis. However, there are no data addressing its relevance regarding therapeutic decision-making in clinical practice.
Objective
To evaluate the impact of EMMs to drive the treatment decision-making in patients with SpA in a 12-month follow-up.
Patients and methods
SpA patients, according to the axial and peripheral ASAS classification criteria, as well as CASPAR criteria, with any active EMM, defined as main entry criteria, were included in this longitudinal cohort study. Individuals with a history of any disease or condition that could be associated with some of the studied endpoints, including neoplasms and infectious diseases, were excluded. Specific tools related to each EMM, including Psoriasis Area Severity Index (PASI), ophthalmologic evaluation, according to the Standardization of Uveitis Nomenclature (SUN) criteria, and gut complaints were used at baseline and during the 3-, 6- and 12-month of follow-up as outcomes measures over time. Descriptive and inferential analyses were used appropriately, including Pearson’s correlation test, chi-squared test, and ANOVA. P value less than 0.05 was considered as significant.
Results
A total of 560 patients were enrolled, of whom 472 meet the eligibility criteria. The majority (N = 274; 59.6%) had one or more EMM related to SpA umbrella concept. Among the EMM, the one that most influenced therapeutic decision-making was psoriasis (28.5%), followed by uveitis (17.5%) and IBD (5.5%), regardless of musculoskeletal manifestations. Clinical improvement of EMMs outcomes was observed in most patients over 12-month follow-up, especially in those with rAAU and IBD (P < 0.001).
Conclusion
Our results showed that EMMs guided the therapeutic decision-making in half of SpA patients, regardless of musculoskeletal condition, suggesting the inter-disciplinarity among the rheumatologist, ophthalmologist, dermatologist, and gastroenterologist plays a crucial role to manage them.
Similar content being viewed by others
Introduction
Spondyloarthritis (SpA) is a group of distinct chronic inflammatory diseases that share the enthesis involvement, as well as a genetic association with HLA-B27 and extra-musculoskeletal manifestations (EMM), including psoriasis (Ps), recurrent acute anterior uveitis (rAAU), and inflammatory bowel disease (IBD). They can affect 30–50% of patients during SpA course and are included in the axial and peripheral Assessment of Spondyloartrhitis (ASAS) classification criteria [1,2,3]. In addition, all of them may contribute to increase pre-test probability for SpA and are associated with higher costs and quality of life impairment [4,5,6,7,8,9,10,11,12,13,14].
Although no randomized clinical trial has evaluated the EMMs as primary outcome nor they are clearly indicated in most international guidelines [15,16,17,18,19] or included in SpA disease-activity instruments, such as Ankylosing Spondylitis Disease Activity Score (ASDAS) and Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) [20, 21], they have been used to guide treatment decisions in a real-life setting. In addition, it is common that patients with EMMs require a multidisciplinary and interdisciplinary approach involving the participation of rheumatologists, ophthalmologists, dermatologists, and gastroenterologists.
Thus, our main objectives were to evaluate the EMMs’ role regarding the therapeutical decision-making in patients with axial or peripheral SpA [22, 23], as well as to verify the main joint outcomes, including data on efficacy and safety after treatment, in a 12-month follow-up.
Patients and methods
This cohort study enrolled outpatients with SpA from the Spondyloarthritis Service of Rheumatology Division of Federal University of São Paulo (UNIFESP). Adult patients with axial SpA [1,2,3, 22], psoriatic arthritis (PsA) [23] and IBD-related arthritis [3, 24] were included if they had any active EMM that determined the therapeutic decision-making (defined as main entry criteria and major target during all follow-up), regardless of axial or peripheral arthritis at baseline, according to the overall opinion of rheumatologist. All patients who had the EMM as decisive to perform the therapeutic decision-making were included in the study and were followed-up of at least 12 months after that.
Individuals with a history of any condition that could be associated or cause misinterpretation or diagnostic confusion with any of the studied outcomes were excluded such as neoplasia, active infection by Human Immunodeficiency Virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV), active tuberculosis, Hansen’s disease, sarcoidosis, infectious uveitis, sexually transmitted diseases, demyelinating diseases, changes in bowel habits of other etiologies (such as lactose intolerance, celiac disease, or irritable bowel syndrome), pregnancy, and dermatoses of other etiologies. Patients with juvenile-onset SpA, overlap with other chronic inflammatory arthritis, or undifferentiated conditions were not eligible to participate in the study.
The electronic medical records were revised to obtain all clinical manifestations, comorbidities, and treatment data. The articular and EMMs were evaluated at baseline, as well as throughout the follow-up (3, 6, and 12 months), to determine the impact of the decision on the response to treatment (complete or incomplete response or remission), according to rheumatologist’s overall evaluation. If the patient had more than one EMM, it was chosen the one that has been more determinant for therapeutic decision-making, according to the rheumatologist’s global opinion.
For the specific evaluation of the activity and severity of articular and EMMs, specific instruments to each one of them were used, including the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) [21], Ankylosing Spondylitis Disease Activity Score (ASDAS) [20], and Psoriasis Area and Severity Index (PASI) [25].
The ASDAS was used to define joint disease activity (ASDAS < 1.3 was considered as remission, ASDAS ≥ 1.3 and < 2.1 was considered as low joint activity, and ASDAS ≥ 2.1 was considered as high or very high activity) [20]. Ps activity was defined according to PASI (active if ≥ 1 and inactive when < 1), and dermatologist and rheumatologist’s overall opinion. rAAU was defined as active or inactive according to the ophthalmologic evaluation, which was based on the Standardization of Uveitis Nomenclature (SUN) Working Group criteria [26]. Improvement, worsening, or unchanged outcomes (active or inactive) were assigned according to the ophthalmologist’s opinion. Measurements of inflammatory bowel disease activity were based on signs and symptoms, such as abdominal pain and bowel habits changes (number of episodes of diarrhea per day, presence of blood or mucus in stool). Patients who presented one or more symptoms different from the usual pattern were characterized as having active IBD if confirmed by colonoscopy. from the time when the digestive condition was responsible for guiding the treatment throughout the following 12 months. The intestinal involvement (IBD) was confirmed by colonoscopy or biopsy previously and current gut activity was defined as clinically active or inactive, according to both gastroenterologist and rheumatologist’s overall opinion.
In addition, all patients included in this cohort had previous diagnosis of psoriasis, recurrent anterior uveitis, and inflammatory bowel disease, according to the dermatologist, ophthalmologist, and gastroenterologist, respectively. Also, the current skin lesions, eye and gut complaints were confirmed by these specialists. However, the final therapeutic decision-making was performed by rheumatologist based on multidisciplinary to manage them.
The therapeutic approach was based on the Brazilian and the international guidelines [15,16,17,18,19], using the treat to target (T2T) strategy. The options for pharmacological strategies were:
- Non-steroidal anti-inflammatory drugs (NSAIDs): initiation or dosage adjustments (full- or half-dose, continuum, or intermittent use), considering previous usage and safety profile of each patient.
- Conventional synthetic Disease-modifying antirheumatic drugs (csDMARDs): Initiation, maintenance or change of agents (methotrexate, leflunomide, cyclosporine, sulfasalazine, azathioprine) or dosage adjustments or combination among them, according to the response, compliance, and tolerability.
- Biologic DMARDs, such as TNFα inhibitors (infliximab, adalimumab, certolizumab, golimumab and etanercept): Initiating, maintaining, or switching among them and no-TNF blockers, including IL17, IL23 or IL12-23 inhibitors and abatacept. Combination among biologicals was not allowed. No patient used targeted synthetic DMARDs, as JAK inhibitors.
Topic glucocorticosteroids (GCs) were added in patients with mild episodes of psoriatic skin lesions or AAU, according to the dermatologist and ophthalmologist, respectively. Systemic GCs were used in patients with moderate-severe or refractory colitis or AAU, according to the gastroenterologist or ophthalmologist, respectively, and they were not prescribed for skin lesions.
Statistical analysis
The quantitative variables are described as the mean, median, standard deviation, minimum, and maximum values. The qualitative variables are described as absolute and relative frequencies (%). Fisher's exact test or the chi-squared test was used to assess the association among the qualitative variables in the different groups of EMMs. In case of a normal distribution, according to the Shapiro–Wilk test, and the homogeneity among the variables, the quantitative variables were compared over time by repeated-measures analysis of variance (ANOVA), and the original group was set as the fixed factor using an intention-to-treat (ITT) analysis. In the case non-normality or non-homogeneity, the non-parametric Kruskal–Wallis test was applied. In situations of significant differences between the variables, the multiple comparison test with Bonferroni correction was used.
Using the approach that most of EMMs may improve after synthetic or biologic DMARDs used to treat the joint complaints, we explored if the articular endpoints could also improve when the therapeutic option had been defined based on just EMMs as decision-making.
To evaluate the distribution of data over time for quantitative variables, such as PASI, the non-parametric Friedman test was applied. For qualitative variables, especially medications, Cochran’s Q test was performed to compare different proportions over time. All data were analyzed using SPSS version 24.0 and P value below 5% was set as significant.
Results
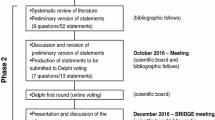
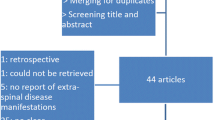
A total of 560 patients were evaluated, of whom 472 (84.3%) had a diagnosis of SpA, according to the ASAS classification criteria. Of these, 12 were excluded because they presented comorbidities that could influence the evaluation of disease activity (articular or extra-articular), such as infectious hepatitis (three patients with hepatitis C, one patient with hepatitis B), acquired immunodeficiency syndrome (AIDS) (N = 6), and neoplasms (one patient with bladder adenocarcinoma and one patient with chronic lymphoid leukemia) (Fig. 1).
Any EMM was observed in 274 (59.6%) patients at baseline, 141 (51.5%) of them had active Ps, AUU or IBD that defined the therapeutic decision-making (Ps in 78 patients [28.5%]; rAAU in 48 [17.5%]; and IBD in 15 [5.5%] (Fig. 1). Patients with Ps activity were predominantly male, older, with a longer disease duration, and higher prevalence of current smokers. Patients with active rAAU were younger and had higher frequency of SpA family history, axial involvement, and positivity for HLA-B27. Patients with IBD activity had significantly shorter diagnostic delay. All of them were predominantly White, but no significant difference regarding sex and fibromyalgia and low bone mass frequency (Table 1).
In a 12-month follow-up, there was a significant PASI reduction (Fig. 2a), as well as less mean daily episodes of diarrhea (Fig. 2b), less patients with abdominal pain and blood and mucus in stools or uveitis activity (Table 2). Although the therapeutic decision-making has been chosen according to current activity of EMM, there was a tendency toward an improvement of musculoskeletal complaints (low disease activity), especially in those with Ps (from 15.5 to 34%) and IBD (from 7.1 to 33.3%) over time (Table 3).
A 12-Month follow-up regarding skin and gut disease activity over time (At baseline, visits at 3, 6 and 12 months). a Patients with psoriasis and psoriasis area and severity index (PASI) after therapeutic decision-making. b Patients with inflammatory bowel disease and daily diarrhea episodes after therapeutic decision-making
The decision-making usefulness was significant over 12-month follow up in all groups, especially for rAAU, which was determinant for the management in more than 90% of patients who had it, and for Ps (in more than 50% of those who had it) (Table 4). No serious adverse events were observed in these patients during follow up.
Among the patients with active Ps, approximately 30% had not used any medication previously, and more than 50% were using some DMARD, especially methotrexate (MTX). At baseline, only 15% had already used some immunobiological agent. Plaque was the most frequent clinical presentation in patients with Ps (more than 90% of cases)—together with nail dystrophy (more than 70% of patients)—and it impacted regarding the treatment decision-making significantly. The other forms represented fewer than 10% of cases. The therapeutic decision-making significantly promoted the largest increases in the prescription of DMARDs, both alone (monotherapy) or in combination, especially regarding TNF inhibitors, followed by secukinumab. In addition, there was a non-significant reduction of using the systemic GCs, although they were using the same rate as topical formulations (Table 5).
Of those with active rAAU, half of them had not used any systemic medication before, fewer than 20% had used some DMARDs, and approximately 30% were using some biologic agent (Table 6). After 3 months, there was no significant reduction in the oral systemic use of GCs, although there was a significant increase in DMARDs prescriptions, especially MTX and monoclonal TNF-inhibitors over the 12 months.
Regarding patients with active IBD, approximately 30% had not previously used any medication. Approximately 20% were using some DMARDs or systemic GCs, and approximately 40% of them were on biologic DMARDs (Table 7). Over the 12-month follow-up, there was no reduction in oral systemic use of GCs, but there was a significant increase in DMARDs prescription, especially sulfasalazine and biologic agents. In addition, more than half of patients continued using these agents over 12 months.
Discussion
Our results showed that almost 60% of SpA patients had some active EMM and in about half of them it guided the current therapeutic decision-making in a real-life scenario. In addition, we observed a more specific approach focusing on them, including higher prescription rate in conventional DMARDs-naïve patients previously.
Although a large prospective cohort with 12 years of follow-up, the Outcome in Ankylosing Spondylitis International Study (OASIS), has not found any association among EMMs and physical disability, quality of life, or radiographic damage in 216 patients with AS [27], most studies have highlighted the relevance of them on the quality of life in SpA patients, as well as the association with direct and indirect costs and difficulties in clinical management [28, 29]. Nonetheless, no clinical trial has evaluated the EMMs as a central point of therapeutic decision-making. To the best of our knowledge, this is the first large study that addressed the efficacy and safety peculiarities of them in SpA patients over time in clinical practice, regardless of musculoskeletal axial or peripheral predominance, highlighting a relevant and current unmet need.
In general, the EMMs had high prevalence in SpA patients, as demonstrated in a large British cohort involving more than 4000 AS patients and almost 29,000 healthy controls matched for age and sex (11.4% for rAAU, 4.4% for Ps and 3.7% for IBD). The overall incidence per 1000 patient-years, as well as the cumulative incidence in 20 years and the adjusted risk ratio (8.9, 24.5% and 15.5 for rAAU; 3.4, 10.1% and 1.5 for Ps and 2.4, 7.5% and 3.3 for IBD, respectively), demonstrated that the risks were higher in the first years for Ps and IBD but keep increasing over time for rAAU [7, 30, 31]. However, only 60% of European and Canadian rheumatologists routinely have evaluated them, even though they agree that the therapeutic strategy is different when musculoskeletal (MSK) complaints are concomitantly with EMMs in SpA patients [32]. According to our cohort, the Ps activity was the most frequent, but the active rAAU was the EMM with greater dissociation from joint disease activity and that was used as treatment strategy turning point in more than 90% of patients.
Another interesting approach is to screen the EMMs to reduce the diagnostic delay in SpA, especially for differential diagnosis with other inflammatory arthritis [33]. Recently, several strategies have been adopted for identifying them in patients with Ps [13, 22], such as the Psoriasis Arthritis Screening and Evaluation (PASE) [35], Psoriasis Epidemiology Screening Tool (PEST) [36, 37], and Early Psoriatic Arthritis Screening Questionnaire (EARP) [38]; uveitis, including the DUET [39], FOCUS Initiative [40], and Sentinel Collaborative Project [41]; and IBD (ASAS criteria [11] and the DETAIL questionnaire [42]). Although these strategies had not been evaluated in our study, we could realize that a driven sight to them would be important to integrate rheumatologists, dermatologists, ophthalmologists, and gastroenterologists for therapeutic decision-making as well. For instance, Ps patients had a longer delay until the appointment with the rheumatologist, emphasizing an important unmet need and the necessity the greater interaction with dermatologists. On the other hand, the access to and faster scheduling with the rheumatologist was more frequent for patients with IBD, although the time was more than 5 years, on average. Our data confirm the possibility of multidisciplinary assessment regarding EMMs in SpA patients [43, 44].
Comorbidities also represent relevant outcomes regarding clinical management of SpA patients, especially due to concomitant medications, increased risk of toxicity, and decision-making [45], and have been more valued recently [46, 47]. An interesting finding in our cohort was the lower prevalence of fibromyalgia (less than 15%), when considering only the current active EMMs, than that reported in patients with AS and non-radiographic axial SpA (around 20–25%) [8, 34, 48,49,50]. On the other hand, our data corroborate the higher rate of metabolic syndrome in Ps [51] and osteoporosis in patients with IBD, which may be associated with the longer systemic use of GCs, chronic inflammation and intestinal malabsorption of calcium, vitamin D, and other nutrients essential for bone health [52]. These three comorbidities are also important in a real-life study, especially related to need for using corticosteroid sparing drugs to minimize risk of weight increase, bone loss, hypertension, lipid and glucose changes, and non-alcoholic steatohepatitis (NASH), as well as to improve the interpretation of disease activity tools based on patient-reported outcomes (PROs) and to reduce confounders factors for the therapeutic decision-making.
By using EMMs in therapeutic decision-making, we observed significant clinical improvement in the three groups, especially in those with rAAU or IBD, with complete resolution in 85% or 75% of cases, respectively. Psoriasis lesions also improved overall, but there was greater difficulty in achieving complete and sustained remission during the first year, suggesting the greater complexity of psoriatic disease itself in despite of higher frequency of TNF inhibitors and wide care offered by dermatology and rheumatology combined approach. Moreover, it is worthy addressing that we used a stricter criterion for defining skin remission (PASI below 1). Although with several definitions regarding skin remission in patients with psoriatic arthritis and psoriasis, including PASI75, PASI90, PASI100, and BSA for instance, we decided to use the PASI as more trustworthy parameter based on the skin domain from the Minimal Disease Activity (MDA)’s definition [17, 58]. Also, it would be an endpoint easier for using in the clinical practice and might reflect better the “skin well-being” related to the patient-reported outcomes.
Interestingly, the improvement of musculoskeletal complaints was not as significant as the improvement of EMMs that motivated the therapeutic decision. Some hypotheses to explain this can be highlighted, such as a lower frequency of joint disease activity (remission or low disease activity in approximately 25 to 40% of patients with Ps and rAAU, respectively) and dissociation between articular and extra-articular involvement in patients with long-term disease.
Although the profile of biological agents, including first prescription and survival rate, may vary according to the EMM, the monoclonal TNF inhibitors were more prescribed for patients with rAAU and IBD, according to current recommendations [15,16,17,18,19]. In our cohort, these data are supported because more than half of the patients in IBD and rAAU groups required only one change in treatment, suggesting effectiveness of this strategy over time. Moreover, most of them had switched to another monoclonal TNF antagonist. However, SpA patients with Ps required more treatment changes demonstrating the difficulty of managing them.
Another interesting finding in our cohort was the lack of combined medication before the EMM comes up to provide a decision-making (30% in Ps and IBD, 50% in rAAU), as well as the low baseline prescription rates of DMARDs (20% in rAAU and IBD patients, and 50% for Ps patients) and biological agents (15% in Ps, 30% in AAUr, 40% in IBD), which suggests that extra-muskuloskeletal involvement was recent and relevant for clinical management, regardless of joint complaints [53].
MTX was the anchor drug more used in SpA patients with current active and concomitant rAAU and Ps, but it was not the main therapeutic strategy chosen by Rheumatologist because it was already being used by more than 50% of patients with Ps. The most important strategy involving synthetic or conventional DMARDs, as the first therapeutic approach, was a combination of DMARDs, such as leflunomide or cyclosporin, although this strategy has not been sustained over 12 months, suggesting lower efficacy or higher toxicity. In cases of current active IBD in SpA patients, sulfasalazine was used as an anchor medication, as it saw a threefold increase in its prescription in the first 3 months.
The EMMs were decisive for the DMARDs prescription, with a frequency of approximately 30% in Ps, 40% in IBD, and 60% in rAAU. In addition, they were responsible by higher prescription of biological agents (fourfold increase for TNF inhibitors in the first 6 months and an 15% increment considering other mechanisms of action in patients with Ps activity after 12 months).
In SpA patients with active rAAU and IBD, there was a 2- to threefold increase of using monoclonal TNFi, especially adalimumab and infliximab, and the need to maintain them over the 12 months, with a low likely of switching. In addition, they were important for reducing the systemic use of GCs, especially in patients with active Ps, but they were not significant in those with rAAU (15%) or IBD (25%). Around 10–20% of patients with Ps and rAAU persisted using topical formulations of GCs, highlighting a severity of these cases and difficulty to control the extra-articular disease activity even using other systemic drugs concomitantly.
Considering all 3 EMMs related to the SpA concept, rAAU was characterized by greater axial involvement (higher frequency of positivity for HLA-B27, earlier disease onset, younger age, a higher rate of syndesmophytes as evaluated by the modified Stoke Ankylosing Spondylitis Spine Score [mSASSS], more stablished impairment on radiographic sacroiliac joints [8], and a higher likelihood of a family history. On the other hand, the peripheral involvement can also occur in 30% of axial cases and it is an important aspect for therapeutic decision-making, especially in patients with Ps and IBD [54]. As it occurred in a large portion of our sample (50–70%), we cannot rule out the possibility of it having also been considered in the decision-making along with the respective extra-articular manifestation, especially in those with psoriasis [55], and it may have determined the worst efficacy and lower survival rate of TNFi [56].
Our study has some limitations, such as the measurement of adherence to treatment and the lack of use of specific instruments for each EMM that are often used in randomized clinical trials (SUN criteria for rAAU, PASI 75 and 90 for Ps, and CDAI for IBD). On the other hand, it has many strengths, including real-life data and incorporation of simpler outcomes, such as complete resolution or not of the EMM, allowing the therapeutic strategy could have had a greater impact on the quality of life of patients and a lower rate of loss to follow-up over 12 months. However, more randomized, and controlled studies are needed to determine the role of EMMs regarding the therapeutic decision-making in SpA patients, as well as an economic resource-use analysis [57].
We found a high prevalence of EMM (50%) that were used to guide treatment decision-making in patients with SpA, regardless of musculoskeletal condition. Therapeutic decision-making based on EMMs could promote a change in behavior and achievement of better overall disease activity control, especially in patients with rAAU and IBD15−8. In addition, the first management strategy was effective in most patients and no serious adverse events were observed after the decision had been made.
In conclusion, our results emphasize the relevance of considering the EMMs in the clinical and epidemiological context of SpA, especially regarding decision-making in clinical practice, as well as to evaluate the therapeutic response and to be added to the treat-to-target approach. In addition, they emphasize the need to consider instruments that can assess the global disease activity and the relevance for a multidisciplinary in SpA patients [15,16,17,18,19]. More recently, minimal disease activity has incorporated the PASI or BSA data for a more complete evaluation of patients with PsA [58]. Similarly, these strategies should be also used for the rAAU and IBD.
Availability of data and materials
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Sieper J, Rudwaleit M, Baraliakos X, Brandt J, Braun J, Burgos-Vargas R, et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis. 2009;68(Suppl 2):ii1-44.
Poddubnyy D, van Tubergen A, Landewé R, Sieper J, van der Heijde D, Assessment of SpondyloArthritis international Society (ASAS). Development of an ASAS-endorsed recommendation for the early referral of patients with a suspicion of axial spondyloarthritis. Ann Rheum Dis. 2015;74(8):1483–7.
Rudwaleit M, van der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68(6):777–83.
Elewaut D, Matucci-Cerinic M. Treatment of ankylosing spondylitis and extra-articular manifestations in everyday rheumatology practice. Rheumatology Oxford. 2009;48(9):1029–35.
Mitulescu TC, Popescu C, Naie A, Predeţeanu D, Popescu V, Alexandrescu C, et al. Acute anterior uveitis and other extra-articular manifestations of spondyloarthritis. J Med Life. 2015;8(3):319–25.
Stolwijk C, Essers I, van Tubergen A, Boonen A, Bazelier MT, De Bruin ML, et al. The epidemiology of extra-articular manifestations in ankylosing spondylitis: a population-based matched cohort study. Ann Rheum Dis. 2015;74(7):1373–8.
Braun J, Baraliakos X, Listing J, Sieper J. Decreased incidence of anterior uveitis in patients with ankylosing spondylitis treated with the anti-tumor necrosis factor agents infliximab and etanercept. Arthritis Rheum. 2005;52(8):2447–51.
Oliveira TL, Maksymowych WP, Lambert RGW, Muccioli C, Fernandes ARC, Pinheiro MM. Sacroiliac joint magnetic resonance imaging in asymptomatic patients with recurrent acute anterior uveitis: a proof-of-concept study. J Rheumatol. 2017;44(12):1833–40.
Martin TM, Rosenbaum JT. An update on the genetics of HLA B27-associated acute anterior uveitis. Ocul Immunol Inflamm. 2011;19(2):108–14.
Karreman MC, Luime JJ, Hazes JMW, Weel AEAM. The Prevalence and Incidence of Axial and Peripheral Spondyloarthritis in Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. J Crohns Colitis. 2017;11(5):631–42.
Stolwijk C, Pierik M, Landewé R, Masclee A, van Tubergen A. Prevalence of self-reported spondyloarthritis features in a cohort of patients with inflammatory bowel disease. Can J Gastroenterol J Can Gastroenterol. 2013;27(4):199–205.
Fragoulis GE, Liava C, Daoussis D, Akriviadis E, Garyfallos A, Dimitroulas T. Inflammatory bowel diseases and spondyloarthropathies: From pathogenesis to treatment. World J Gastroenterol. 2019;25(18):2162–76.
Ranza R, Carneiro S, Qureshi AA, Martins G, Rodrigues JJ, Romiti R, et al. Prevalence of psoriatic arthritis in a large cohort of Brazilian patients with psoriasis. J Rheumatol. 2015;42(5):829–34.
Carron P, Van Praet L, Van den Bosch F. Peripheral manifestations in spondyloarthritis: relevance for diagnosis, classification and follow-up. Curr Opin Rheumatol. 2012;24(4):370–4.
Resende GG, Meirelles E de S, Marques CDL, Chiereghin A, Lyrio AM, Ximenes AC, et al. The Brazilian Society of Rheumatology guidelines for axial spondyloarthritis - 2019. Adv Rheumatol. 2020;60(1):19.
van der Heijde D, Ramiro S, Landewé R, Baraliakos X, Van den Bosch F, Sepriano A, et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis. 2017;76(6):978–91.
Coates LC, Gossec L, Ramiro S, Mease P, van der Heijde D, Smolen JS, et al. New GRAPPA and EULAR recommendations for the management of psoriatic arthritis. Rheumatol Oxford. 2017;56(8):1251–3.
Ward MM, Deodhar A, Gensler LS, Dubreuil M, Yu D, Khan MA, et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol Hoboken. 2019;71(10):1599–613.
Ramiro S, Nikiphorou E, Sepriano A, Ortolan A, Webers C, Baraliakos X, et al. ASAS-EULAR recommendations for the management of axial spondyloarthritis: 2022 update. Ann Rheum Dis. 2023;82(1):19–34.
Machado PM, Landewé R, Heijde D van der, Assessment of SpondyloArthritis international Society (ASAS). Ankylosing Spondylitis Disease Activity Score (ASDAS): 2018 update of the nomenclature for disease activity states. Ann Rheum Dis. 2018;77(10):1539–40.
Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994;21(12):2286–91.
van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984;27(4):361–8.
Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H, et al. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum. 2006;54(8):2665–73.
Rudwaleit M, van der Heijde D, Landewé R, Akkoc N, Brandt J, Chou CT, et al. The Assessment of SpondyloArthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis. 2011;70(1):25–31.
Schmitt J, Wozel G. The psoriasis area and severity index is the adequate criterion to define severity in chronic plaque-type psoriasis. Dermatol Basel Switz. 2005;210(3):194–9.
Jabs DA, Nussenblatt RB, Rosenbaum JT, Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509–16.
Essers I, Ramiro S, Stolwijk C, Blaauw M, Landewé R, van der Heijde D, et al. Do extra-articular manifestations influence outcome in ankylosing spondylitis? 12-year results from OASIS. Clin Exp Rheumatol. 2016;34(2):214–21.
Carron P, Van Praet L, Jacques P, Elewaut D, Van den Bosch F. Therapy for spondyloarthritis: the role of extra-articular manifestations (eye, skin). Rheum Dis Clin North Am. 2012;38(3):583–600.
Garg N, van den Bosch F, Deodhar A. The concept of spondyloarthritis: where are we now? Best Pract Res Clin Rheumatol. 2014;28(5):663–72.
Stolwijk C, van Tubergen A, Castillo-Ortiz JD, Boonen A. Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74(1):65–73.
de Winter JJ, van Mens LJ, van der Heijde D, Landewé R, Baeten DL. Prevalence of peripheral and extra-articular disease in ankylosing spondylitis versus non-radiographic axial spondyloarthritis: a meta-analysis. Arthritis Res Ther. 2016;18:196.
Van den Bosch F. A survey of European and Canadian rheumatologists regarding the treatment of patients with ankylosing spondylitis and extra-articular manifestations. Clin Rheumatol. 2010;29(3):281–8.
Khan MA, Haroon M, Rosenbaum JT. Acute anterior uveitis and spondyloarthritis: more than meets the eye. Curr Rheumatol Rep. 2015;17(9):59.
Mease PJ, Karki C, Palmer JB, Etzel CJ, Kavanaugh A, Ritchlin CT, et al. Clinical characteristics, disease activity, and patient-reported outcomes in psoriatic arthritis patients with dactylitis or enthesitis: results from the corrona psoriatic arthritis/spondyloarthritis registry. Arthritis Care Res. 2017;69(11):1692–9.
Qureshi AA, Dominguez P, Duffin KC, Gladman DD, Helliwell P, Mease PJ, et al. Psoriatic arthritis screening tools. J Rheumatol. 2008;35(7):1423–5.
Ibrahim GH, Buch MH, Lawson C, Waxman R, Helliwell PS. Evaluation of an existing screening tool for psoriatic arthritis in people with psoriasis and the development of a new instrument: the Psoriasis Epidemiology Screening Tool (PEST) questionnaire. Clin Exp Rheumatol. 2009;27(3):469–74.
Mease PJ, Palmer JB, Hur P, Strober BE, Lebwohl M, Karki C, et al. Utilization of the validated Psoriasis Epidemiology Screening Tool to identify signs and symptoms of psoriatic arthritis among those with psoriasis: a cross-sectional analysis from the US-based Corrona Psoriasis Registry. J Eur Acad Dermatol Venereol JEADV. 2019;33(5):886–92.
Tinazzi I, Adami S, Zanolin EM, Caimmi C, Confente S, Girolomoni G, et al. The early psoriatic arthritis screening questionnaire: a simple and fast method for the identification of arthritis in patients with psoriasis. Rheumatol Oxford. 2012;51(11):2058–63.
Haroon M, O’Rourke M, Ramasamy P, Murphy CC, FitzGerald O. A novel evidence-based detection of undiagnosed spondyloarthritis in patients presenting with acute anterior uveitis: the DUET (Dublin Uveitis Evaluation Tool). Ann Rheum Dis. 2015;74(11):1990–5.
Dick AD, Rosenbaum JT, Al-Dhibi HA, Belfort R, Brézin AP, Chee SP, et al. Guidance on noncorticosteroid systemic immunomodulatory therapy in noninfectious uveitis: Fundamentals Of Care for UveitiS (FOCUS) Initiative. Ophthalmology. 2018;125(5):757–73.
Juanola X, Loza Santamaría E, Cordero-Coma M, SENTINEL Working Group. Description and Prevalence of Spondyloarthritis in Patients with Anterior Uveitis: The SENTINEL Interdisciplinary Collaborative Project. Ophthalmology. 2016;123(8):1632–6.
Di Carlo M, Luchetti MM, Benfaremo D, Di Donato E, Mosca P, Maltoni S, et al. The DETection of Arthritis in Inflammatory boweL diseases (DETAIL) questionnaire: development and preliminary testing of a new tool to screen patients with inflammatory bowel disease for the presence of spondyloarthritis. Clin Rheumatol. 2018;37(4):1037–44.
Felice C, Leccese P, Scudeller L, Lubrano E, Cantini F, Castiglione F, et al. Red flags for appropriate referral to the gastroenterologist and the rheumatologist of patients with inflammatory bowel disease and spondyloarthritis. Clin Exp Immunol. 2019;196(1):123–38.
Redeker I, Callhoff J, Hoffmann F, Haibel H, Sieper J, Zink A, et al. Determinants of diagnostic delay in axial spondyloarthritis: an analysis based on linked claims and patient-reported survey data. Rheumatology Oxford. 2019;58(9):1634–8.
Scriffignano S, Perrotta FM, De Socio A, Lubrano E. Role of comorbidities in spondyloarthritis including psoriatic arthritis. Clin Rheumatol. 2019;38(1):3–10.
Walsh JA, Song X, Kim G, Park Y. Evaluation of the comorbidity burden in patients with ankylosing spondylitis using a large US administrative claims data set. Clin Rheumatol. 2018;37(7):1869–78.
Validation of the self-administered comorbidity questionnaire adjusted for spondyloarthritis: results from the ASAS-COMOSPA study - PubMed [Internet]. https://pubmed.ncbi.nlm.nih.gov/31665462/
Azevedo VF, Paiva E dos S, Felippe LRH, Moreira RA. Occurrence of fibromyalgia in patients with ankylosing spondylitis. Rev Bras Reumatol. 2010;50(6):646–50.
Bello N, Etcheto A, Béal C, Dougados M, Moltó A. Evaluation of the impact of fibromyalgia in disease activity and treatment effect in spondyloarthritis. Arthritis Res Ther. 2016;18:42.
Palm O, Moum B, Jahnsen J, Gran JT. Fibromyalgia and chronic widespread pain in patients with inflammatory bowel disease: a cross sectional population survey. J Rheumatol. 2001;28(3):590–4.
Choudhary S, Pradhan D, Pandey A, Khan MK, Lall R, Ramesh V, et al. The association of metabolic syndrome and psoriasis: a systematic review and meta-analysis of observational study. Endocr Metab Immune Disord Drug Targets. 2020;20(5):703–17.
Szafors P, Che H, Barnetche T, Morel J, Gaujoux-Viala C, Combe B, et al. Risk of fracture and low bone mineral density in adults with inflammatory bowel diseases. A systematic literature review with meta-analysis. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2018;29(11):2389–97.
García-Vicuña R, Zarco P, González CM, Vanaclocha F, Marín-Jiménez I, Cea-Calvo L. Two-year incidence of psoriasis, uveitis and inflammatory bowel disease in patients with spondyloarthritis: A study in the AQUILES cohort. Reumatol Clin. 2016;12(1):22–6.
Molto A, Sieper J. Peripheral spondyloarthritis: Concept, diagnosis and treatment. Best Pract Res Clin Rheumatol. 2018;32(3):357–68.
de Winter JJ, Paramarta JE, de Jong HM, van de Sande MG, Baeten DL. Peripheral disease contributes significantly to the level of disease activity in axial spondyloarthritis. RMD Open. 2019;5(1):e000802.
Kim Y, Park S, Kim H-S. The effect of extra-articular manifestations on tumor necrosis factor-α inhibitor treatment duration in patients with ankylosing spondylitis: nationwide data from the Korean College of Rheumatology BIOlogics (KOBIO) registry. Clin Rheumatol. 2018;37(12):3275–84.
Gao X, Wendling D, Botteman MF, Carter JA, Rao S, Cifaldi M. Clinical and economic burden of extra-articular manifestations in ankylosing spondylitis patients treated with anti-tumor necrosis factor agents. J Med Econ. 2012;15(6):1054–63.
Coates LC, Fransen J, Helliwell PS. Defining minimal disease activity in psoriatic arthritis: a proposed objective target for treatment. Ann Rheum Dis. 2010;69(1):48–53.
Acknowledgements
To Spondyloarthritis Session, Rheumatology Division, UNIFESP/EPM, for support in the recruitment of patients as well as by performing all measurements in different times.
Funding
This research was funded by authors' own resources and the patients were provided from Hospital São Paulo – Federal University of Sao Paulo (Unifesp/ EPM).
Author information
Authors and Affiliations
Contributions
DRA: Data acquisition, patient recruitment, database review, data analysis, results interpretation, manuscript writing. TLO: Patient care, rheumatology outpatient appointment, writing and critical review. VOM: Patient care, rheumatology outpatient appointment. MMP: Conception and study design, research leadership, rheumatology outpatient appointment, data analysis, results interpretation, manuscript writing and final critical revising for intellectual content. All authors approved the final version of manuscript and Agreement in ensuring that questions related to the data accuracy and integrity are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Research at the Federal University of Sao Paulo (CAAE: 73705317.3.0000.5505). Subjects were included in the study after signing an informed consent form.
Consent for publication
We assure that the data presented here was not published elsewhere and the article has not been submitted to any other journal. We give our consent for the publication of the manuscript “Extra-musculoskeletal manifestations driving the therapeutic decision-making in patients with Spondyloarthritis: a 12-month follow-up cohort”.
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
dos Reis Annunciato, D., Oliveira, T.L., Magalhães, V.O. et al. Extra-musculoskeletal manifestations driving the therapeutic decision-making in patients with Spondyloarthritis: a 12-month follow-up prospective cohort study. Adv Rheumatol 63, 44 (2023). https://doi.org/10.1186/s42358-023-00324-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-023-00324-0