Abstract
Background
Rheumatoid arthritis (RA) is a systemic autoimmune disease characterized by chronic inflammation of the joints, especially of the hands. The evaluation of handgrip strength (HS) and pinch strength can be useful to detect reduction in hand function in RA patients. The aim of the study was to compare HS and pinch strength between RA patients (RA Group - RAG) and a non-RA control group (CG) and to relate HS and pinch strength to functional capacity, duration and disease activity in the RAG.
Methods
A cross-sectional case control study. The RAG was assessed for disease activity by the Disease Activity Score (DAS-28); for functional capacity by the Health Assessment Questionnaire (HAQ), the Cochin Hand Functional Scale (CHFS) questionnaire, and the Disability of the Arm, Shoulder, and Hand (DASH) questionnaire; and for HS and pinch strength (2-point tip-to-tip, lateral or key, and 3-point) using Jamar® and pinch gauge dynamometers, respectively. Associations were analyzed by Pearson and Spearman tests, and groups were compared by the independent samples t test, with a significance level of P < 0.05.
Results
The convenience sample included 121 rheumatoid patients and a control group matched by age, sex, and body mass index. The RAG showed lower strength values compared with the CG in all measurements (P < 0.01, 95% CI) and these values were associated with worse performance in the functional questionnaires and greater disease activity and duration. There was a strong correlation among the functional assessment instruments.
Conclusions
The decrease in grip and pinch strength, easily measured by portable dynamometers, is a strong indicator of functional disability in RA patients.
Similar content being viewed by others
Background
Rheumatoid arthritis (RA) is a chronic inflammatory joint disease that preferentially affects the hands, resulting in reductions in muscle strength and mobility and deformities associated with considerable functional impairment [1, 2]. Loss of muscle strength, made worse by lack of use [3], can impair the basic grip and pinch functions of the hands. Some studies conducted with portable dynamometers have shown reductions in hand strength in patients with RA compared with healthy controls and correlated with functional ability [4,5,6,7,8]. However, such studies exhibit several limitations, such as small sample size, lack of control groups, and poor description of the measurement protocols.
The aims of the present study were to measure the hand grip strength (HS) and pinch strength of individuals with RA, compared with a control group, and to correlate hand strength with functional ability and length and activity of disease.
Methods
This cross-sectional, case-control study was conducted with individuals with RA (RA group - RAG) followed up at the rheumatology outpatient clinic, School of Medicine of Marilia, interior of the state of São Paulo, Brazil. Controls (Control group - CG), matched by sex, age, and body mass index (BMI), were selected among escorts of patients at the rheumatology outpatient clinic and at the internal medicine, obstetrics, and otorhinolaryngology outpatient clinics.
The Institutional Ethics Committee, under Certificate of Presentation for Ethical Appraisal (CAAE) 45,124,815.0000.5413, approved the study. Participants were included in the study after signing an informed consent form. The study was conducted from September 2015 to September 2016.
Sample size was calculated using a two-tailed test with the significance level set to 5, 90% power, standard deviation 9.8 kgf [9] for handgrip strength, and a clinically significant difference of 4.5 kgf. To compensate for eventual losses, the calculated sample size was increased by 20%, resulting in 121 participants per group.
Individuals 18 years old or older were included. RAG members had to meet the classification criteria formulated by the American College of Rheumatology in 1987 (ACR 1987) or the criteria formulated by the American College of Rheumatology and the European League Against Rheumatism in 2010 (ACR/ EULAR 2010) [10, 11]. Exclusion criteria for both groups were understanding, cognition, or sensory deficits hindering participation in interviews; skin or neurological lesions impairing the grip and pinch functions; and amputation of the upper limbs. Individuals with hand joint complaints were excluded from CG.
Patients with RA were subjected to assessment of activity of disease. All participants were subjected to measurements of body mass and height (Filizola mechanical scale with stadiometer, 100-g and 0.1-cm precision), functional ability questionnaires, and hand dynamometry.
Disease activity was assessed by means of the Disease Activity Score (DAS28) and the measurement of C-reactive protein (CRP; immunoturbidimetric method) [12,13,14]. The DAS28 final score was interpreted according to the following classification: remission ≤2.4; low disease activity ≤3.2; moderate activity ≤5.5; and high activity > 5.5, and according to the Boolean definition of remission (2010 ACR/EULAR remission criteria): tender and swollen joint count < 1, CRP ≤ 1 mg/dl, and visual analog scale (VAS) score ≤ 1 or Simplified Disease Activity Index (SDAI) ≤ 3 [15, 16].
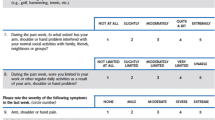
Functional ability was assessed by means of 3 questionnaires: a) the Health Assessment Questionnaire (HAQ), one of the most widely used for patients with RA and that was translated to and validated for the Portuguese language [17,18,19]; b) the Cochin Hand Functional Scale (CHFS), developed in France initially for assessment of patients with RA and then extended to other conditions, and translated and adapted for Brazilian populations [20, 21]; and c) the Disability of the Arm, Shoulder, and Hand (DASH) questionnaire, developed for assessment of the upper limb functional ability in various conditions and translated, validated, and adapted for the Portuguese language in 2005 [22, 23].
Hand strength was assessed with the participants sitting on an armless chair, with 90° elbow flexion, forearms in a neutral position, and 0 to 30° wrist extension. Maximum strength was assessed after a 3-s sustained contraction; the average of 3 attempts at 1-min intervals was considered for analysis. During the tests, all participants received verbal feedback by means of the sentence “strength, strength, strength” [24, 25]. Measurements included a) handgrip strength (HS) measured with a Jamar® hydraulic dynamometer at handle position 2, as established by the American Society of Hand Therapists (ASHT); results were recorded in kilogram-force (kgf) [24], and b) pinch strength measured using a B&L Engineering® PG-30 pinch gauge, including 2-point tip-to-tip pinch strength (classic, between the thumb and index finger), lateral or key pinch strength (between the pad of the thumb and the lateral surface of the middle phalanx of the index finger), and 3-point pinch strength (between the thumb, index, and middle fingers) [26].
The data were subjected to descriptive statistics; normality was assessed by means of the Kolmogorov-Smirnov test. Groups were matched 1:1 by sex, age, and BMI and were compared with the t-test. Correlations were investigated using Pearson’s and Spearman’s tests, and the strength of correlation was categorized as follows: 0.0 to 0.3, non-significant; 0.3 to 0.5 weak; 0.5 to 0.7 moderate; 0.7 to 0.9 strong; and 0.9 to 1.0 very strong [27]. Intergroup comparisons were performed by means of the independent t-test, with significance level P < 0.05. Analyses were performed with software Statistical Package for the Social Sciences (SPSS version 24) - US.
Results
Figure 1 most participants in the groups were female, married, and white (self-reported ethnicity) with a low educational level, reported arterial hypertension, and were right-handed for writing and performing activities of daily living (ADL). Details on the characteristics of the participants from both groups are described in (Tables 1 and 2).
Rheumatoid factor tested positive in 78.5% (n = 95) of participants in the RAG; data on anti-citrullinated protein antibodies (ACPAs) were missing for 43 patients. The drug most widely used by patients was methotrexate, 71.9% (n = 87), followed by leflunomide, 52.9% (n = 64), and hydroxychloroquine, 38% (n = 46) (Tables 3 and 4).
Length of disease did not exhibit any significant correlations with activity of disease, scores on questionnaires, or functional ability.
In a separate analysis by age range (10-year interval) in the RAG, we found that HS decreased after 35 years of age and was more accentuated after 65 years of age. In the CG, the highest strength level was exhibited by G2, with a gradual decline with age (Table 5).
The scores on the functional ability scales showed strong mutual correlations: HAQ and CHFS 0.789 (P < 0.01), HAQ and DASH 0.825 (P < 0.01), and CHFS and DASH 0.820 (P < 0.01), but weak correlations with activity of disease.
There was no correlation of hand strength and functional ability with RA Boolean remission (Table 6).
Discussion
The handgrip strength and pinch strength were lower among the patients with RA compared with the controls. Handgrip strength and pinch strength were lower among patients with poorer functional ability but showed weak correlations with activity and length of disease.
The average age of the participants was 58 years; age did not exhibit a correlation with HS, as has been described in the literature [1, 18, 28,29,30,31].
A study conducted with healthy individuals found that the peak HS occurred in the age range of 25 to 39 years; pinch strength remained stable until age 59 years, followed by a gradual decline together with age [32]. In another study performed with healthy Brazilians, peak HS occurred in the age range of 35 to 39 years, followed by a gradual decline with age [33]. A study that analyzed patients with RA did not find a difference in 2-point pinch after 5-year follow up [34]. However, the meta-analysis conducted by Beenakker et al. [31] showed a decline of HS before age 50 years, suggesting that the disease might cause premature aging. In our study, we did not find a clear-cut strength reduction gradient, but strength declined in the groups with patients older than 35 years, similar to previous studies; this variation might be attributed to the expected loss of muscle mass and strength that occurs after age 40. The group with patients older than 65 years old showed additional HS reduction, which is consistent with the frailty developed by older seniors [35].
There is controversy regarding hand strength and dominance. Some studies conducted with healthy individuals found significant differences, with the dominant hand being the strongest [36]. Two studies simultaneously analyzed patients with RA and healthy individuals. In one study, the dominant hand was 20% weaker than the non-dominant one among patients with RA and 8% stronger among healthy individuals [37]. The other study found differences among the healthy participants only [38]. In our study, we did not find a correlation between strength and dominance in either group; in addition, dominance might be influenced by several factors, such as work and leisure demands [39].
Regarding associated diseases, systemic arterial hypertension was the most prevalent in the analyzed sample. Use of cardiovascular medications has been associated with HS reduction in a cohort of older adults [40]. In our study, neither hypertension nor use of medications – with similar prevalence rates in both groups – showed a relationship with hand strength.
There was no difference in hand strength according to the use of synthetic drugs for disease control. An isolated correlation was detected between pinch strength and the use of a biological agent, without sufficient consistency to infer a causal relationship.
Rheumatoid factor – related to poor prognosis in RA – tested positive in 78.5% of the RAG, somewhat above the average of 70% reported in the literature [18]; however, positive rheumatoid factor was not associated with hand strength. Data on ACPAs were missing for 43 patients; therefore, we did not investigate their correlation with hand strength.
A meta-analysis performed in 2010 [31] found that the average HS of patients with RA was 17.68 kgf. Although the analyzed studies had excluded individuals with diabetes mellitus, chronic obstructive pulmonary disease, and testosterone and/or growth hormone deficiencies, the abovementioned value is similar to the one we found in the present study, in which patients with such conditions were not excluded. Alomari et al. [41] found a 30% reduction in HS among patients with RA compared with healthy individuals recruited from the local community without ischemia, systemic arterial hypertension, angina, diabetes mellitus, anemia, dyslipidemia, kidney failure, obesity, or higher cardiovascular risk and who were nonsmokers. Even without excluding participants with any of these conditions, in our study, we found a similar difference between patients and controls.
The study by Dedeoğlu et al., which correlated hand strength with pain, activity of disease, functional ability, and joint lesions in RA, found average values of 24.6 kgf for HS, 4.4 kgf for tip-to-tip pinch strength, 5.65 kgf for 3-point pinch strength, and 6.65 kgf for lateral pinch strength. These values are higher than those found in the present study; however, Dedeoğlu et al. excluded individuals with diabetes mellitus, hypo- or hyperthyroidism, and cervical disc disease [9], constituting a sample with a profile different from the one met in clinical practice. In addition, their study did not include a control group.
The data described above show that there is wide variability among studies, with the issue of the inclusion of control groups being crucial. When designing our study, we took special care to include a control group with a profile similar to the one of patients seen in clinical practice, who have several associated diseases, and to match the groups according to variables with potentially strong influences on hand strength. We believe that one strength of our study is that it has satisfactory internal quality without any impairment of its external validity.
In their study, Poole et al. [42] found that among patients with RA, HS, 2-point tip-to-tip, and 3-point pinch strength were lower with lower hand functional ability, as measured by means of the CHFS. Another study assessed HS, 2-point tip-to-tip, 3-point pinch strength, and lateral pinch strength and found the same correlations with functional ability [9]. Although utilizing a small sample of 36 patients with RA, Adams et al. [4] found that DASH showed a strong correlation with HS and 3-point pinch strength and suggested that DASH is the best instrument to discriminate the functional ability of the upper limbs. Similarly, the study by Nampei et al. [43] concluded that there were significant correlations of 2-point tip-to-tip, 3-point pinch strength, and lateral pinch strength with loss of hand function among patients with RA. This is the only study that also described associations with thumb and index deformities. In addition, our study showed associations with hand function, but we did not record deformities.
The DAS28 score (2.98 ± 1.32) showed a weak correlation with grip and pinch strength. A recent study found a moderate negative correlation between DAS28 score and grip and pinch strength, as measured with a dynamometer coupled to a smartphone; the authors concluded that HS might contribute to the assessment of disease activity in the outpatient setting [44]. In addition, a recent pilot study reported a reduction of HS among patients with RA and high disease activity and a negative correlation of HS with pain and swelling [38].
In contrast, in our study, we observed a weak correlation between strength and disease activity, which was not expected because the hand joints have considerable weight on the DAS28 scores. There were correlations for some of the hand strength parameters, but those correlations were below 0.3 in all cases, i.e., they were clinically insignificant.
There was not any significant difference between patients with Boolean remission and active RA; however, the low representation of the former, just 8 patients, makes drawing robust conclusions difficult [38, 45].
Like ours, one study observed a strong correlation between CHFS and HAQ [9], which reinforces the fact that RA hand involvement impairs functional ability in a global manner [46].
In the validation study of CHFS for the Brazilian population, it showed moderate correlation with DASH. Conversely, in our study, these two instruments showed a strong correlation, which might be accounted for by the fact that RA affects not only the small but also the large joints of the upper limbs. There is considerable overlap among the items assessed with the HAQ, CHFS, and DASH, rendering their simultaneous use unnecessary. However, there is a wide diversity of parameters cited in the literature; thus, we chose to apply all three instruments to enable comparisons with other studies.
Length of disease had a significant, albeit, weak correlation with functional activity, as was the case of the study by Dedeoğlu et al., who used CHFS [9], and Toyama et al. [34], who employed DASH, which must be quite variable as a function of disease aggressiveness, early diagnosis, and intensity of treatment in each patient.
We believe that our study provides a relevant reference for the measurement of hand strength in patients with RA, as the sample size was larger compared with the studies available in the literature [37, 38, 41, 45, 47]. In addition, we used a control group composed of individuals with sociocultural profiles similar to those of the RA patients and matched per sex, age, and BMI; therefore, both the internal and external validity are satisfactory. Nevertheless, we admit some limitations, such as not having recorded radiological deformities of the hands and fingers, which might be associated with measurements of strength.
Several issues still need to be elucidated. Our sample did not have a sufficient number of patients for assessment of the hand strength impairment at baseline, which might contribute to discriminating the roles that inflammation and sequelae play in loss of strength. The sample size was also restricted for the purpose of drawing conclusions on male patients. What is the correlation between hand strength and lower limb strength and risk of falls? What are the impacts of rehabilitation programs and physical exercise on hand strength among patients with RA? These data will contribute to elucidate the potential of hand strength measurement along the follow-up of patients with RA as an additional parameter for therapeutic decision-making to contribute to improve the functional ability and quality of life of patients and disease control.
We conclude that handgrip and pinch strength were lower in patients with RA compared with individuals without disease. Grip and pinch strength were inversely correlated with global functional ability and hand and upper limb function; however, they showed weak correlations with activity and length of disease.
References
Louzada-Júnior P, Souza BDB, Toledo RA, Ciconelli RM. Análise descritiva das características demográficas e clínicas de pacientes com artrite reumatóide no estado de São Paulo. Brazil Rev Bras Reumatol. 2007;47(2):84–90.
Sociedade Brasileira de Reumatologia. Artrite reumatoide: diagnóstico e tratamento. In: Associação Médica Brasileira e Comissão Federal. São Paulo: Projeto Diretrizes; 2002.
Helliwell PS, Jackson S. Relationship between weakness and muscle wasting in rheumatoid arthritis. Ann Rheum Dis. 1994;53(11):726–8.
Vargas A, Chiapas-Gasca K, Hernández-Díaz C, Canoso JJ, Saavedra MÁ, Navarro-Zarza JE, et al. Clinical anatomy of the hand. Reumatol Clin. 2013;8(2):25–32.
Bodur H, Yilmaz O, Keskin D. Hand disability and related variables in patients with rheumatoid arthritis. Rheumatol Int. 2006;26(6):541–4.
Adams J, Burridge J, Mullee M, Hammond A, Cooper C. Correlation between upper limb functional ability and structural hand impairment in an early rheumatoid population. Clin Rehabil. 2004;18(4):405–13.
Santana FS, Nascimento DC, Freitas JPM, Miranda RF, Muniz LF, Santos Neto L, et al. Avaliação da capacidade funcional em pacientes com artrite reumatoide: implicações para a recomendação de exercícios físicos. Rev Bras Reumatol. 2014;54(5):378–85.
Oku EC, Pinheiro GRC, Araújo PMP. Hand functional assessment in patients with rheumatoid arthritis. Fisioter Mov. 2009;22(2):221–8.
Dedeoğlu M, Gafuroğlu Ŭ, Yilmaz Ö, Bodur H. The relationship between hand grip and pinch strengths and disease activity, articular damage, pain and disability in patients with rheumatoid arthritis. Turk J Rheumatol. 2013;28(2):69–77.
Villeneuve E, Nam J, Emery P. ACR-EULAR classification criteria for rheumatoid arthritis. Rev Bras Reumatol. 2010;50(5):481–3.
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European league against rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–81.
Wells G, Becker JC, Teng J, Dougados M, Schiff M, Smolen J, et al. Validation of the 28-joint disease activity score (DAS28) and European league against rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythrythrocyte sedimentation rate. Ann Rheum Dis. 2009;68(6):954–60.
Pinheiro GRC. Instrumentos de medida da atividade da artrite reumatóide - Por que e como empregá-los. Rev Bras Reumatol. 2007;47(5):362–5.
Prevoo ML, Van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, Van RP. Modified disease activity scores that include twenty-eight-joint development and validation in a prospective longitudinal study of patients with arthritis, rheumatoid. Arthritis Rheum. 1995;38(1):44–8.
Felson DT, Smolen JS, Wells G, Zhang B, Van LHD, Funovits J, et al. American College of Rheumatology / European league against rheumatism provisional Defi nition of remission in rheumatoid arthritis for clinical trials. Ann Rheum Dis [Internet]. 2011;70(3):404–13.
Bykerk VP, Massarotti EM. The new ACR/EULAR remission criteria: rationale for developing new criteria for remission. Rheumatol (United Kingdom). 2012;51(SUPPL. 6):16–20.
Corbacho MI, Dapueto JJ. Avaliação da capacidade funcional e da qualidade de vida de pacientes com artrite reumatoide. Rev Bras Reum. 2010;50(1):31–43.
Mota LMH, Cruz BA, Brenol CV, Pereira IA, Fronza LSR, Bertolo MB, et al. Consenso da Sociedade Brasileira de Reumatologia 2011 para o diagnóstico e avaliação inicial da artrite reumatoide. Rev Bras Reumatol. 2011;51(3):199–219.
Bruce B, Fries JF. The health assessment questionnaire (HAQ). Clin Exp Rheumatol. 2005;23(5 Suppl 39):S14–8.
Chiari A, Sardim CC, Natour J. Translation, cultural adaptation and reproducibility of the cochin hand functional scale questionnaire for Brazil. Clinics (Sao Paulo). 2011;66(5):731–6.
Lefevre-Colau MM, Poiraudeau S, Fermanian J, Etchepare F, Alnot JY, Le Viet D, et al. Responsiveness of the cochin rheumatoid hand disability scale after surgery. Rheumatology. 2001;40(8):843–50.
Aktekin LA, Eser F, Başkan BM, Sivas F, Malhan S, Öksüz E, et al. Disability of arm shoulder and hand questionnaire in rheumatoid arthritis patients: relationship with disease activity, HAQ, SF-36. Rheumatol Int. 2011;31(6):823–6.
Orfale AG, Araújo PMP, Ferraz MB, Natour J. Translation into Brazilian Portuguese, cultural adaptation and evaluation of the reliability of the disabilities of the arm, shoulder and hand questionnaire. Brazilian J Med Biol Res. 2005;38(2):293–302.
Shiratori AP, Iop R, Borges Júnior NG, Domenech SC, Gevaerd MS. Protocolos de avaliação da força de preensão manual em indivíduos com artrite reumatoide: uma revisão sistemática. Rev Bras Reum. 2014;54(2):140–7.
Kapandji AI. Fisiologia articular: esquemas comentados de mecânica humana: membro superior. 5 ed. Panamericana São Paulo. 2000;1:140–298.
Häkkinen A, Kautiainen H, Hannonen P, Ylinen J, Mäkinen H, Sokka T. Muscle strength, pain, and disease activity explain individual subdimensions of the health assessment questionnaire disability index, especially in women with rheumatoid arthritis. Ann Rheum Dis. 2006;65(1):30–4.
Mukaka MM. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24(3):69–71.
Vaz AE. Perfil epidemiológico e clínico de pacientes portadores de artrite reumatóide em um hospital escola de medicina em Goiânia, Goiás, Brasil. Med (Ribeirão Preto). 2013;46(2):141–53.
Alamanos Y, Drosos AA. Epidemiology of adult rheumatoid arthritis. Autoimmun Rev. 2005;4(3):130–6.
Goeldner I, Skare T, Reason I, Utiyama S. Artrite reumatoide: uma visão atual. J Bras Patol Med Lab. 2011:495–503. [cited 2015 Feb 9]; Available from: http://www.scielo.br/pdf/jbpml/v47n5/v47n5a02.pdf
Beenakker KG, Ling CH, Meskers CG, de Craen AJ, Stijnen T. Westendorp RGet al. Patterns of muscle strength loss with age in the general population and patients with a chronic inflammatory state. Ageing Res Rev. 2010;9(4):431–6.
Mathiowetz V, Kashman N, Volland G, Weber K, Dowe M, Rogers S. Grip and pinch strength: normative data for adults. Arch Phys Med Rehabil. 1985;66(2):69–74.
Caporrino FA, Faloppa F, Santos JBG, Réssio C, Soares FHC, Nakachima LR, et al. Estudo populacional da força de preensão palmar com dinamômetro Jamar. Rev Bras Ortop. 1998;33(2):150–4.
Toyama S, Tokunaga D, Fujiwara H, Oda R, Kobashi H, Okumura H, et al. Rheumatoid arthritis of the hand: a five-year longitudinal analysis of clinical and radiographic findings. Mod Rheumatol. 2014;24(1):69–77.
Lenardt MH, Binotto MA, Carneiro NHK, Cechinel C, Betiolli SE, Lourenço TM. Handgrip strength and physical activity in frail elderly. Rev Esc Enferm USP. 2016;50(1):86–92. https://doi.org/10.1590/S0080-623420160000100012.
Nicolay CW, Walker AL. Grip strength and endurance: influences of anthropometric variation, hand dominance, and gender. Int J Ind Ergon. 2005;35(7):605–18.
Fraser A, Vallow J, Preston A, Cooper RG. Predicting’normal’ grip strength for rheumatoid arthritis patients. Rheumatology. 1999;38(6):521–8.
Iop RR, Shiratori AP, Ferreira L. Borges Júnior, Domenech SC, Gevaerd MS. Capacidade de produção de força de preensão isométrica máxima em mulheres com artrite reumatoide : um estudo piloto. Fisioter Pesq. 2015;22(1):11–6.
Figueiredo IM, Sampaio RF, Mancini MC, Silva FCM, Jamar SMAPT d f d p u o d. Acta Fisiátrica. 2007;14:104–10.
Ashfield TA, Syddall HE, Martin HJ, Dennison EM, Cooper C, Aihie Sayer A. Grip strength and cardiovascular drug use in older people: findings from the Hertfordshire cohort study. Age Ageing. 2009;39(2):185–91.
Alomari MA, Keewan EF, Shammaa RA, Alawneh K, Khatib SY, Welsch MA. Vascular function and handgrip strength in rheumatoid arthritis patients. Sci World J. 2012;2012:1–6.
Poole JL, Santhanam DD, Latham AL. Hand impairment and activity limitations in four chronic diseases. J Hand Ther. 2013;26(3):232–6.
Nampei A, Shi K, Hirao M, Murase T, Yoshikawa H, Hashimoto J. Association of pinch strength with hand dysfunction, finger deformities and contact points in patients with rheumatoid arthritis. Clin Exp Rheumatol. 2011;29(6):1061.
Espinoza F, Le Blay P, Coulon D, Lieu S, Munro J, Jorgensen C, et al. Handgrip strength measured by a dynamometer connected to a smartphone: a new applied health technology solution for the self-assessment of rheumatoid arthritis disease activity. Rheumatology. 2016;55(5):897–901.
Sheehy C, Gaffney K, Mukhtyar C. Standardized grip strength as an outcome measure in early rheumatoid arthritis. Scand J Rheumatol. 2013;42(4):289–93.
Birtane M, Kabayel DD, Uzunca K, Unlu E, Tastekin N. The relation of hand functions with radiological damage and disease activity in rheumatoid arthritis. Rheumatol Int. 2008;28(5):407–12.
Cima SR, Barone A, Porto JM, de Abreu DC. Strengthening exercises to improve hand strength and functionality in rheumatoid arthritis with hand deformities: a randomized, controlled trial. Rheumatol Int. 2013;33(3):725–32.
Acknowledgements
Jamil Natour and Anamaria Jones from the Spine, Procedures, and Rehabilitation in Rheumatology Sector at Rheumatology Division, UNIFESP, Brazil for their support and for making dynamometers available.
Funding
To the Coordination for the Improvement of Higher Education Personnel (CAPES) for the assistance of research through the scholarship awarded.
Author information
Authors and Affiliations
Contributions
GSS: Main author and acted in data collection, literature review and author of the manuscript. MAL: Acted in data collection. MRA: He acted as counselor and critically reviewed the manuscript for key intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Authors’ information
Graziela Sferra da Silva.
Specialization in physiology of physical exercise and resitance training in health, disease and aging. Main author and acted in data collection, literature review and author of the manuscript.
Mariana de Almeida Lourenço.
PhD stundent in the Human Development and Technologies Program at Unesp Rio Claro Campus, MSc in Health and Aging at Marilia School of Medicine (Famema). Acted in data colletion.
Marcos Renato de Assis.
PhD in Sciences by the Rehabilitation Program. He acted as advisor and reviewer of the manuscript.
Ethics approval and consent to participate
All participants received verbal and written guidance and were included after signing the Free and Informed Consent Term. The study was approved by the Research Ethics Committee of the School of Medicine of Marília, opinion number 1,470,862.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sferra da Silva, G., de Almeida Lourenço, M. & de Assis, M.R. Hand strength in patients with RA correlates strongly with function but not with activity of disease. Adv Rheumatol 58, 20 (2018). https://doi.org/10.1186/s42358-018-0020-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-018-0020-1