Abstract
Background
Coexisting pathologies is not a new phenomenon and can cause diagnostic difficulties when they overshadow one another. They may alter the cytomorphology of cells and the machine readings to an extent that the actual diagnosis is missed. One such scenario is created by coexisting megaloblastic anemia and beta-thalassemia trait where the RBC indices and the hemoglobin chromatogram findings conform to neither of the two.
Case presentation
We present two cases of anemia presenting with normocytic normochromic indices, increased red cell distribution width (RDW), elevated HbA2 levels and moderately high HbF levels in both of them and an additional low HbA1c in case 2. Upon evaluation of peripheral smear and biochemical tests, a non-immune hemolytic component was also identified with deficient Vit B12 levels in case 1 and highly elevated levels post-supplementation in case 2.
Conclusions
Taking together the peripheral smear, erythrogram, chromatogram and biochemical findings, it was deduced that the alterations were caused by coexisting beta-thalassemia trait and megaloblastic anemia. Vit B12 deficiency was the cause behind hemolysis owing to intramedullary destruction of abnormal precursors. Upon supplementation in case 2, the immediate reticulocyte response was the reason behind spuriously low HbA1c.
Similar content being viewed by others
Introduction
Beta-thalassemia is an inherited blood disorder in which there is insufficient synthesis of beta-globin chains. The degree of impairment determines the phenotypic severity of disease. Individuals with beta-thalassemia trait (BTT) have one unaffected beta-globin gene which produces sufficient hemoglobin to fulfill general body needs. Reduced β-chain synthesis is compensated by a relative increase in the number of δ-chains which bind with α-chains to form HbA2 tetramers. An uncomplicated BTT is characterized by microcytic hypochromic RBCs on peripheral smear and mildly elevated HbA2 levels on Hb electrophoresis or chromatography (HPLC) (Needs Gonzalez-Mosquera Lynch 2022).
Deficiency of Vitamin B12 impacts the nuclear maturation and division of hematological precursors in the bone marrow resulting in an increase in the number of large dyspoietic red blood cell precursor forms also called as megaloblasts. At times, these abnormal forms undergo intramedullary hemolysis causing ineffective erythropoiesis (Wu et al. 2021). The end result is a low RBC count followed by low Hb levels, with evidence of macrocytosis with macro-ovalocytes, high RDW and hypersegmented polymorphs on peripheral smear. Additional findings supportive of hemolysis (indirect hyperbilirubinemia and elevated LDH levels) can also be seen.
When BTT coexists with Vit B12 deficiency, the low MCV in BTT is balanced by a high MCV in Vit B12 deficiency resulting in normalization of MCV. If peripheral smear examination and Hb electrophoresis are skipped, such cases can be easily mistaken for any normocytic normochromic anemia with a high RDW. The first differential being a hemolytic anemia in this scenario. This can cause unnecessary indulgence in other investigations such as autoimmune workup, bone marrow examination, etc., thereby delaying the diagnosis. To further elaborate on this, we would like to present two cases where the coexistence of BTT and Vit B12 deficiency posed a diagnostic dilemma.
Case presentation
Case 1
A 17-year-old female presented with the complaints of weakness, fatigue and difficulty in breathing. Her Hb was found to be low (6.4 g/dl). The complete erythrogram and chromatogram are displayed in Table 1 and Fig. 1a. Additionally, she had indirect hyperbilirubinemia (4.4 mg/ml), low Vitamin B12 levels (44 pg/ml), normal serum iron levels and negative Coomb’s test. Peripheral smear (PS) revealed a mixed population of macrocytic and normocytic normochromic RBCs with macro-ovalocytes (Fig. 2a). Total leukocyte count (TLC) and differential leukocyte count (DLC) were normal. Few hypersegmented neutrophils were noted. Platelets were adequate. The corrected reticulocyte count was low (1.6%).
Case 2
A 32-year-old female presented with extreme weakness, generalized pallor and a Hb of 7.4 g/dl. Table 1 and Fig. 1b show the erythrogram and chromatogram of this case. She had indirect hyperbilirubinemia (4.7 mg/ml), hyperferritinemia (> 1500 mg/dl) and elevated serum iron levels (147 mg/ml). Lactate dehydrogenase (LDH) levels were high (523 IU/L). Vitamin B12 levels were > 1500 pg/ml. Coomb’s test was negative. PS revealed macro-ovalocytes, nucleated RBCs (nRBCs) and polychromatic macrocytes (Fig. 2b). TLC, DLC and platelets were within normal limits. Hypersegmented neutrophils were seen. The corrected reticulocyte count was 5.2%.
Tables 2 and 3 summarize the similarities and differences in the finding between the two cases.
Though the chromatograms in both these cases were consistent with a diagnosis of BTT, the RBC indices were those of a normocytic normochromic anemia. To further confirm the diagnosis of BTT, the parental chromatograms were examined. The results were compatible with BTT in the samples drawn from the mother in both cases. Genetic studies were not done due to financial constraints.
In case 1, low Vit B12 levels with evidence of macro-ovalocytes and hypersegmented neutrophils on PS confirmed the coexistence of a megaloblastic anemia which had altered the erythrogram findings.
Case 2 was different because the patient had been injected with Vit B12 supplements in some other center where he was admitted for complaints of extreme weakness and anemia. Because of this reason, the Vit B12 levels were found to be very high at the time of presentation. Despite this, the chromatogram was not much different from case 1 except for extremely low HbA1c values. The presence of nRBCs and a high reticulocyte count was consistent with an accelerated marrow response post-supplementation. Since reticulocytes are nascent immature RBCs which are yet to undergo enzymatic glycation, the HbA1c values can be spuriously low in cases where there is spurt in erythropoiesis like this case where the Vit B12 deficiency was met by supplementation.
Discussion
Coexistence of microcytic hypochromic RBCs in conditions such as iron deficiency or BTT with other types of anemias can mask either of them by altering the RBC indices and chromatogram findings. There are case reports like ours where the low MCV in BTT was obscured by a high MCV of megaloblastic anemia (You et al. 2002; Chan et al. 2007). In contrast with this, Lardhi et al. (Lardhi et al. 2018) reported a microcytic hypochromic blood picture in a patient with combined BTT and MA. The plausible explanation for this can that there was no associated component of hemolysis. Hence, there was no anemia, and the Vit B12 levels were only mildly low at the time of presentation (152 pg/ml). This enabled the abnormal erythroid precursors to escape intramedullary destruction.
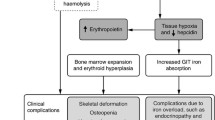
Secondly, though it is not uncommon to have high HbF levels in BTT, the values in our cases were higher (> 4%) than that expected of BTT. It has been reported that HbF levels are elevated in a case of hemolytic anemia (Mandal and Kartthik 2019; Parikh et al. 2005). In fact, HbF is considered an indicator of stress erythropoiesis (Mandal and Kartthik 2019). In simple words, an event-like hemolysis stresses the bone marrow to compensate for the loss of RBCs and in an attempt to do so, there is a predilection for ℽ-chain or HbF synthesis because of its higher oxygen affinity and increased oxygen delivery to tissues in hypoxic conditions (Feng et al. 2022; Schaeffer et al. 2014). This happens because the expression of erythropoietin receptors (EpoR) on erythroid precursors decreases with maturation. EpO acts on EpOR on the early precursors to stimulate erythropoiesis which are more in number and have a higher affinity (Table 4). EpO stimulates Y-globin gene expression and increases HbF levels. As maturation proceeds, ꞵ-chain expression takes over ℽ-chain expression to an extent that the mature RBCs have predominantly HbA. In an event of hemolysis, marrow attempts regeneration by accelerating erythropoiesis thereby shortening the time required for erythroid maturation. As a result, the ℽ- to ꞵ-chain transition is prolonged resulting in relatively elevated HbF levels as also observed in both of our cases. After 15 days on follow-up, their chromatogram revealed normal HbF levels and mildly elevated HbA2 levels consistent with BTT. There was complete resolution of symptoms after Vit B12 supplementation. The post-supplementation erythrograms for the two cases are shared in Table 1.
Conclusions
Coexisting pathologies can sometimes mask the obvious findings and mislead the diagnosis. One such event has been described above. It is important to review the peripheral smear and hemogram along with HPLC before arriving at a conclusion because though HPLC is the gold standard in diagnosing hemoglobinopathies, the morphological changes in RBCs can only be ascertained on PS. For example, microspherocytosis in autoimmune hemolytic anemia, macro-ovalocytes in MA, etc. The PS when correlated with the biochemical findings can be of immense help in identifying the coexisting pathology.
The approach to diagnosis has been presented in the form of a flowchart in Table 5.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- RBCs:
-
Red blood cells
- BTT:
-
Beta-thalassemia trait
- Hb:
-
Hemoglobin
- PS:
-
Peripheral smear
- TLC:
-
Total leukocyte count
- DLC:
-
Differential leukocyte count
- HPLC:
-
High-performance liquid chromatography
- LDH:
-
Lactate dehydrogenase
- nRBCs:
-
Nucleated red blood cells
- RDW:
-
Red cell distribution width
- MCV:
-
Mean corpuscular volume
- MCH:
-
Mean corpuscular hemoglobin
- IDA:
-
Iron deficiency anemia
- MA:
-
Megaloblastic anemia
- EpO:
-
Erythropoietin
- EpOR:
-
Erythropoietin receptor
References
Chan CW, Liu SY, Kho CS, Lau KH, Liang YS, Chu WR, Ma SK (2007) Diagnostic clues to megaloblastic anemia without macrocytosis. Int J Lab Hematol 29:163–171
Feng R, Mayuranathan T, Huang P, Doerfler PA, Li Y, Yao Y, Zhang J, Palmer LE, Mayberry K, Christakopoulos GE, Xu P, Li C, Cheng Y, Blobel GA, Simon MC, Weiss MJ (2022) Activation of γ-globin expression by hypoxia-inducible factor 1α. Nature 610:783–790
Lardhi A, Ali RA, Ali R, Mohammed T (2018) Thalassemia minor presenting with vitamin B12 deficiency, paraparesis, and microcytosis. J Blood Med 9:141–144
Mandal PK, Kartthik S (2019) Autoimmune hemolytic anemia: an uncommon cause of elevated fetal hemoglobin. J Hematopathol 12:19–20
Needs T, Gonzalez-Mosquera LF, Lynch DT (eds) (2022) Beta thalassemia. StatPearls Publishing, StatPearls
Parikh NS, Hoyer JD, Cripe TP (2005) A young girl with hemolytic anemia and elevated hemoglobin F. Pediatr Blood Cancer 44:264–266
Schaeffer EK, West RJ, Conine SJ, Lowrey CH (2014) Multiple physical stresses induce γ-globin gene expression and fetal hemoglobin production in erythroid cells. Blood Cells Mol Dis 52:214–224
Wu Q, Liu J, Xu X, Huang B, Zheng D, Li J (2021) Mechanism of megaloblastic anemia combined with hemolysis. Bioengineered 12:6703–6712
You JU, Chen CC, Lin EK, Ho CH (2002) The characteristics of megaloblastic anemia associated with thalassemia. Haematologica 87:550–551
Acknowledgements
The authors are extremely thankful to the staff of the hematology department for their assistance in gathering the patient files and sparing us the time to conduct this study.
Funding
No funds, grants or any other support were received.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study, conception and design. Material preparation, data collection and analysis were performed by KC. The first draft of the manuscript was written by KC and NS commented on the previous versions of the manuscript. All authors read and approved of the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is an observational study. The head of the department has certified that the study was performed in accordance with the ethical standards as laid down in 1864 declaration.
Consent for publication
Informed consent was obtained from all individuals included in the study.
Competing interests
The authors declare that they have no competing interests in this section.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chauhan, K., Shandilya, N. Two cases of vitamin B12 deficiency in patients with beta-thalassemia trait: lessons in diagnosis. Bull Natl Res Cent 47, 175 (2023). https://doi.org/10.1186/s42269-023-01150-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-023-01150-6