Abstract
Background
Schizophrenia, a chronic mental disorder, has been recognized as one of the heritable diseases with an increased level of dopamine neurotransmitter. Monoamine oxidase A (MAOA) plays a vital role in the catabolism of dopamine. It is a mitochondrial enzyme which is encoded by the MAOA gene located on the X chromosome. The aim of this study was to detect potential biomarker in order to diagnose schizophrenia. Hence, the association of uVNTR repetitions of the MAOA gene and Schizophrenia was investigated.
Method
Blood samples were collected from 102 schizophrenic patients (67 males and 35 females), and 103 volunteers with mental health (65 males and 38 females). Genomic DNA was extracted and the uVNTR polymorphisms were examined using specific primed PCR.
Results
The analysis indicated that genotype 3/3repetition (rep) showed the highest frequency in females. While genotype 4 and 3.5 reps revealed the highest frequencies among schizophrenic patients and healthy controls in men, respectively. There were no significant statistical differences in the number of uVNTR repeats of the MAOA gene between control and case individuals neither in women (OR = 0.35, 95% CI = 0.60–1.43 P = 0.845) nor in men (OR = 0.36, 95% CI = 0.80–1.64, P = 0.365).
Conclusion
In the current study, the number of uVNTR sequence repetitions located in the promoter of the MAOA gene was not associated with the risk of schizophrenia in Iranian patients.
Similar content being viewed by others
Background
Schizophrenia (MIM181500) is a psychotic disorder with specific symptoms such as a disability in speaking and mind arranging, and dismissing the difference between illusion and fact. The epidemiological evidence has indicated that 1% of the total world population are involved with this disorder, especially those who are between 15 and 30 years old. While, in males occurs in the lower ages compared to females (Saha et al. 24).
Schizophrenia is complex disorders with interaction between genes and environmental risk factors. The environmental risk factors such as urbanization, cannabis abuse, psychosocial factors, migration, viral infectious during pregnancy, preeclampsia and hypoxia during delivery have been reported by several authors (Allardyce and Boydell 1; Matheson et al. 16; Vigod et al. 30).
Several studies have been shown that genetic factors and positive family history might have the highest index, approximately 40–85%, in pathogenesis of the disease (McGuffin et al. 18, Cardno et al. 1998, Cardno and Gottesman 2000, Hosak 11, Ebdrup et al. 7). Moreover, based on the studies, molecular and cellular factors, and a single nucleotide polymorphism (SNP) can affect gene expression. Two different models: common disease-common allele and common disease-rare alleles could be attributed to the pathogenesis of the disease (Mitchell and Porteous 19).
Genome-wide association (GWAS) studies have reported more than 100 variants, including SNPs and Copy Number Variations (CNVs), which can be implicated in the occurrence of schizophrenia (Bigdeli et al. 2). However, several studies have confirmed the role of genes like DISC1 (dopamine active transporter 1), NRG1 (Neuregulin 1), RGS4 (Regulator of G protein signaling 4), DTNBP1 (Dystrobrevin Binding Protein 1) in the development of schizophrenia disorder (Sullivan 28). In addition, some variations in COMT (Catechol-O-methyltransferase), SLC6A4 (Solute Carrier Family 6 Member 4), DAT1 (dopamine active transporter 1), MAOA (Monoamine oxidase A) as candidate genes have been reported in association with schizophrenia (Mitchell and Porteous 19).
MAOA gene is recognized as the "Warrior Gene" and encodes the monoamine oxidase A-enzyme which is mainly expressed in catecholaminergic neurons and is involved in regulating the function of synaptic transmitters (McDermott et al. 17). MAOA gene is located on Xp11.3 that contains 15 exons and encodes a protein with a length of 527 amino acids (Shih et al. 25).
Monoamine oxidase enzyme has pivotal roles in monoamine metabolism pathways. In other words, monoamine neurotransmitters, such as norepinephrine, dopamine, and serotonin, are degraded by monoamine oxidase (MAO) in complex with aldehyde dehydrogenase (ALDH) and catecholamine O-methyltransferase (COMT, Kim et al. 13). Sabol et al. (23) suggested that the MAOA transcription of this gene could be affected by genetic variation in the MAOA gene. They demonstrated that a 30 bp repeat sequence, approximately 1.2 kb upstream of the transcription region of the MAOA gene, which is called upstream variable number tandem repeats (uVNTR) affects on expression of the enzyme (Sabel et al. 23). Longer sequences of uVNTR with 3.5 and 4 repeat alleles enhanced MAOA gene transcription compared to shorter alleles such as 2 and 3 repeat (Deckert et al. 6).
In current study, the association between uVNTR genetic variation in the MAOA gene and the risk of Schizophrenia was investigated.
Methods
Clinical study
The project proposal was reviewed by the Ethics Committee of the Islamic Azad University, Science and Research Branch, and was approved with the ID number IR.IAU.SRB.REC.1397.045. The informed consent was obtained from control and case groups or their supervisors.
In the present study, 102 schizophrenic patients who were referred to the psychiatric wards of Imam Hossein and 506 Artesh Hospitals were selected as the case group. Sampling numbers were calculated based on 95%confidence level, 9.5% margin of error, 50% of population proportion and 80 million population size of country. Their disorders were diagnosed by a psychiatrist using demographic questionnaires, clinical interviews based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), and the Positive and Negative Syndrome Scale (PANSS) test. The disorder was confirmed by a psychiatrist.
The criteria for excluding patients from the study included schizoaffective or any other psychiatric disorder, mental retardation, drug, and stimuli abuse. In order to observance ethical considerations, each patient and their supervisor received written consent.
Healthy individuals as the control group consisted of 103 volunteers whose were confirmed by the psychiatrist for mental health, lack of schizophrenia, severe psychiatric disorder or other physical illness, lack of family history of severe mental disorders, and non-use of drugs and stimuli. All participants provided a personal questionnaire including age, ethnic and educational status (Table1).
Molecular analysis
The peripheral blood was collected from each person and stored in tubes containing EDTA anticoagulant at − 80 °C. The Salting Out method was used to extract genomic DNA. The quantity and quality of DNA were checked by a Nanodrop spectrophotometer and 0.8% agarose gel electrophoresis, respectively.
The uVNTR polymorphism in the MAOA gene was amplified by forward primer 5'ACAGCCTGACCGTGGAGAAG3' and reverse primer 5'GAACGGACGCTCCATTCGGA 3'(15). PCR reaction performed by 2X buffer (CinnaGen, Iran), 0.4 μL of dNTP (10 pM, CinnaGen, Iran), 0.5 μL MgCl2 (1.5 mM, CinnaGen,Iran), 0.8 μL of each primer (10pMol, TAG Copenhagen, Denmark), 2 units Taq polymerase (CinnaGen, Iran) and 1 μL DNA (≤ 100 ng). PCR thermal program was 5 min at 94 °C as an initial denaturation, 94 °C for 30 s, following 32 cycles containing three steps, including 58 °C and 74 °C for 30 s and 10 min at 74 °C for the final extension. PCR products were then loaded on 8% polyacrylamide gel and visualized by Sybergreen dye. The Male is hemizygous for this locus (one band) with expected lengths of 294 bp, 324 bp, 339 bp, 354 bp, and 384 bp, while in female, these alleles in homozygous or heterozygous states are predicted. The bands were examined for repeats by sequencing PCR products.
Data analysis
The association of uVNTR and schizophrenia were analyzed using SPSS ver.21 software. The Chi-square and likelihood ratio tests were used for statistical analyses. All tests were analyzed at a probability value less than 0.05 (P < 0.05).
Results
Different alleles with sizes of 294 bp, 324 bp, 339 bp, 354 bp, and 384 bp were shown (Fig. 1), by which confirmed using sanger sequencing method as well (Fig. 2).
PCR products containing MAOA-uVNTR polymorphism fragments detected in 8% polyacrylamide gel electrophoresis (PAGE). Column A: 339 bp fragment (as males are hemizygous for this locus), B: 294 bp,C: 339 bp, M.1: 50 bp DNA Marker, D: 324 bp, E: 339 bp and 354 bp (heterozygote female), F: 324 bp, M.2: 100 bp DNA Marker,G:324 bp and 354 bp, H: 354 bp and 384 bp, N.: No DNA (control), I: 324 bp and 339 bp, J: 354 bp, K: 354 bp, M.3: 50 bp DNA Marker
Sequencing examination of MAOA-uVNTR polymorphism PCR products. a 3.5 repeat genotype sequenced by forward primer. A 30 bp "ACCGGCACCGGCACCAGTACCCGCACCAGT" sequence shows a complete repeat and "ACCGGCACCGGCACC" sequence depicts half of repeat. b 3 repeat genotype sequencing analysis performed by reverse primer. c 4 repeat genotype sequencing analysis performed by reverse primer
As shown in Fig. 2, each repeat contains ACCGGCACCGGCACCAGTACCCGCACCAGT bases, and each half repeat contains 15 bases of ACCGGCACCGGCACC. The sequence of 3.5 repeat genotype (Fig. 2-a) and 3 and 4 repeat genotypes (Fig. 2-b, c) are depicted in Fig. 2.
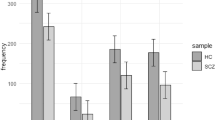
The genotype with 3/3.5 reps was the most frequent among woman group. The frequency of this genotype was 42.9% and 44.7% among the schizophrenic women (35 individuals) and healthy controls (38 individuals), respectively.
Genotype with 4 reps showed the highest frequency among schizophrenic male patients (67 individuals), and the 3.5 reps genotype had the highest frequency among male healthy controls (65 individuals).
No significant differences between the number of uVNTR repeats among female cases and control groups was observed (OR = 0.35, 95% CI = 0.60–1.43 P = 0.845). In addition, no significant difference was observed among males group (OR = 0.36, 95% CI = 0.80–1.64, P = 0.365, Table 2).
Data analyses of demographic traits including age, educational status and ethnics indicated that there was the significant difference (P = 0.001) between educational status of case and control groups. The most of schizophrenia patients were uneducated (Table 1). Meanwhile, analysis of age range and uVNTR repeats showed no significant difference (Additional file 1: Table S1).
Regarding to the ethnicity of the samples, no significant difference between case and control in different ethnicity was observed (Table 1). Based on uVNTR repeats and ethnicity, we found that there is significantly difference (P = 0.03) between frequency of repeats of uVNTR and ethnics in male samples (Additional file 1: Table S2).
Discussion
Schizophrenia a serious mental disorder. The causes of schizophrenia include genetic and environmental factors. Genetic factors include a variety of common and rare genetic variation. Numerous studies have focused on the association of polymorphisms of various genes involved in regulation of neurotransmitters and psychiatric disorders. Considerable evidence has showed that dopamine has an increased response in schizophrenia (Grace 9). Analysis of genome screening studies illustrated that the MAOA gene locus is one of the candidates in developing familial schizophrenia (Laval et al. 14; Bortolato et al. 3; Manca et al. 15). In current study, we selected the uVNTR region in the MAOA gene. The MAOA gene encodes a protein that is involved in oxidative deamination of neurotransmitters.
Clinical studies have examined the association of MAOA uVNTR polymorphism with schizophrenia and reported different results. Syagailo et al. (29) studied on German Caucasian population and they did not reveal any association between the number of uVNTR sequence repeats and schizophrenia. On the other hand, they found uVNTR sequence repeats can play a role in anxiety and aggression in schizophrenic patients (Syagailo et al. 29). Furthermore, studies on Welsh Caucasian (Norton et al. 20), Swedish population (Jönsson et al. 12) and Chinese population (Qiu et al. 22) reported no significant association between the uVNTR sequence of the MAOA gene and schizophrenia in neither males nor females. Moreover, Camarena et al. (4) investigated a significant correlation between uVNTR of the MAOA gene and affective flattening in Mexican female patients, but they found no association between the number of uVNTR sequence repeats and schizophrenia Camarena et al. (4).
Our results were in agreement with studies conducted on Welsh Caucasian (Norton et al. 20) (22), Swedish (Jönsson et al. 12), German Caucasian (Syagailo et al. 29) and Iranian population (Ghamari et al. 8) that revealed the frequency of longer alleles (contained 3.5, 4 and 5 repeat alleles) was higher in both males and females and there were not any significant differences between the case and control groups (Table 3). Meanwhile Hariri et al (10) reported MAOA uVNTR polymorphism in Croatian Schizophrenia. They found significant different number of repeats between case and control (Shumay et al. 27).
The current study revealed that in the female group, there were no significant statistical differences between the number of uVNTR repeats of the MAOA gene among schizophrenic patients, and healthy individuals (P = 0.845). Also, data showed that no significant differences in male group (P = 0.365).
Studies reported that regulatory factors like Non-coding RNAs (lncRNAs and microRNAs) can affect the expression level of the monoamine oxidase A. Furthermore, epigenetic factors can target the MAOA gene by deacetylation and methylation (Shumay et al. 27).
MAOA distal VNTR is located 500 bp upstream of our studied polymorphism and consists of two different types of decamers; Repeat A contains the CCCCTCCCCG sequence, and Repeat B contains the CTCCTCCCCG. These two sequences are alternated up to seven repetitions (ABABABA). Sequence A is added to the regular sequence repeated (ABABABAAAA). Among different populations, 9 and 10 repeat alleles have the highest frequency. Nine-repeat allele is associated with the highest level of transcription and expression of the MAOA gene and 10 repeat allele is associated with the lowest level of transcription. The repeat alleles (11, 8, and 12 reps) have a moderate effect on the transcription and expression of the MAOA gene (Philibert et al. 21).
The regulatory region of the MAOA gene has two CpG islands; one overlapping the promoter and the other is located upstream of the promoter. Hence, an increase in the number of repeats in uVNTR sequence because of increase of methylate cytosines numbers may led to a decrease in the transcription level of the MAOA enzyme (Shumay and Fowler 26). Therefore, it is suggested that polymorphic sequence affects on the activity of the MAOA enzyme and epigenetically control of dopamine levels. Consequently, it seems there are several factors in dopamine control level and uVNTR of MAOA gene could not lonely affect the monoamine oxidase activity.
Conclusions
In conclusion, our data found no significant association of number of repeats in uVNTR region of MAOA gene between schizophrenia patients and controls. The age and ethnicity factors also showed no significantly differences between these two groups, although number of repeats varied in different traits. However, differences in research findings comes from genetic structure of populations and sampling. Polymorphism of different SNPs may affect on MAOA enzyme and further studies are suggested.
Availability of data and material
The current study is not publicly available due personal documents confidentiality. Data are available from corresponding author on request.
Abbreviations
- CI:
-
Confidence interval
- MAOA:
-
Monoamine oxidase A
- OR:
-
Odd ratio
- uVNTR:
-
Upstream variable number tandem repeats
References
Allardyce J, Boydell J (2006) Environment and schizophrenia: review: the wider social environment and schizophrenia. Schizophr Bull 32(4):592–598
Bigdeli TB, Ripke S, Bacanu SA, Lee SH, Wray NR, Gejman PV et al (2016) Genome-wide association study reveals greater polygenic loading for schizophrenia in cases with a family history of illness. Am J Med Genet B Neuropsychiatr Genet 171(2):276–289
Bortolato M, Chen K, Shih JC (2008) Monoamine oxidase inactivation: from pathophysiology to therapeutics. Adv Drug Deliv Rev 60(13–14):1527–1533
Camarena B, Fresán A, Aguilar A, Escamilla R, Saracco R, Palacios J et al (2012) Monoamine oxidase a and B gene polymorphisms and negative and positive symptoms in schizophrenia. ISRN Psychiatry. https://doi.org/10.5402/2012/852949
Cardno AG, Gottesman II (2000) Twin studies of schizophrenia: from bow-and-arrow concordances to star wars Mx and functional genomics. Am J Med Genet 97(1):12–17
Cardno AG, Jones LA, Murphy KC, Sanders RD, Asherson P, Owen MJ, McGuffin P (1998) Sibling pairs with schizophrenia or schizoaffective disorder: Associations of subtypes, symptoms and demographic variables. Psychol Med 28(4):815–823. https://doi.org/10.1017/S0033291798006783
Deckert J, Catalano M, Syagailo YV, Bosi M, Okladnova O, Di Bella D et al (1999) Excess of high activity monoamine oxidase a gene promoter alleles in female patients with panic disorder. Hum Mol Genet 8(4):621–624
Ebdrup B (2018) Schizophrenia is a clinically and biologically heterogeneous syndrome. Ugeskrift Laeger. 180(6).
Ghamari R, Yazarlou F, Khosravizadeh Z et al (2022) Serotonin transporter functional polymorphisms potentially increase risk of schizophrenia separately and as a haplotype. Sci Rep 12:1336. https://doi.org/10.1038/s41598-022-05206-x
Grace AA (2016) Dysregulation of the dopamine system in the pathophysiology of schizophrenia and depression. Nat Rev Neurosci 17(8):524
Hariri A, Mattay VS, Tessitore A, Kolachana B, Fera F, Goldman D et al (2002) Serotonin transporter genetic variation and the response of the human amygdala. Science 297:400–403
Hosak L (2013) New findings in the genetics of schizophrenia. World J Psychiatry 3(3):57
Jönsson EG, Norton N, Forslund K, Mattila-Evenden M, Rylander G, Åsberg M et al (2003) Association between a promoter variant in the monoamine oxidase a gene and schizophrenia. Schizophr Res 61(1):31–37
Kim SK, Park HJ, Seok H, Jeon HS, Chung J-H, Kang WS et al (2014) Association study between monoamine oxidase A (MAOA) gene polymorphisms and schizophrenia: lack of association with schizophrenia and possible association with affective disturbances of schizophrenia. Mol Biol Rep 41(5):3457–3464
Laval S, Dann J, Butler R, Loftus J, Rue J, Leask S et al (1998) Evidence for linkage to psychosis and cerebral asymmetry (relative hand skill) on the X chromosome. Am J Med Genet 81(5):420–427
Manca M, Pessoa V, Lopez AI, Harrison PT, Miyajima F, Sharp H et al (2018) The regulation of monoamine oxidase a gene expression by distinct variable number tandem repeats. J Mol Neurosci 64(3):459–470
Matheson SL, Shepherd AM, Laurens KR, Carr VJ (2011) A systematic meta-review grading the evidence for non-genetic risk factors and putative antecedents of schizophrenia. Schizophr Res 133(1–3):133–142
McDermott R, Dawes C, Prom-Wormley E, Eaves L, Hatemi PK (2013) MAOA and aggression: a gene–environment interaction in two populations. J Confl Resolut 57(6):1043–1064
McGuffin P, Owen MJ, O’Donovan MC, Thapar A, Gottesman I (1994) Seminars in psychiatric genetics. BMJ 309(6957):818
Mitchell KJ, Porteous DJ (2011) Rethinking the genetic architecture of schizophrenia. Psychol Med 41(1):19–32
Norton N, Kirov G, Zammit S, Jones G, Jones S, Owen R et al (2002) Schizophrenia and functional polymorphisms in the MAOA and COMT genes: no evidence for association or epistasis. Am J Med Genet 114(5):491–496
Philibert RA, Wernett P, Plume J, Packer H, Brody GH, Beach SR (2011) Gene environment interactions with a novel variable monoamine oxidase a transcriptional enhancer are associated with antisocial personality disorder. Biol Psychol 87(3):366–371
Qiu HT, Meng HQ, Song C, Xiu MH, Zhu FY, Wu GY et al (2009) Association between monoamine oxidase (MAO)-A gene variants and schizophrenia in a Chinese population. Brain Res 1287:67–73
Sabol SZ, Hu S, Hamer D (1998) A functional polymorphism in the monoamine oxidase a gene promoter. Hum Genet 103(3):273–279
Saha S, Chant D, Welham J, McGrath J (2005) A systematic review of the prevalence of schizophrenia. PLoS Med 2(5):e141
Shih J, Chen K, Ridd M (1999) Monoamine oxidase: from genes to behavior. Annu Rev Neurosci 22(1):197–217
Shumay E, Fowler JS (2010) Identification and characterization of putative methylation targets in the MAOA locus using bioinformatic approaches. Epigenetics 5(4):325–342
Shumay E, Logan J, Volkow ND, Fowler JS (2012) Evidence that the methylation state of the monoamine oxidase A (MAOA) gene predicts brain activity of MAO A enzyme in healthy men. Epigenetics 7(10):1151–1160
Sullivan PF (2005) The genetics of schizophrenia. PLoS Med 2(7):e212
Syagailo YV, Stöber G, Gräßle M, Reimer E, Knapp M, Jungkunz G et al (2001) Association analysis of the functional monoamine oxidase a gene promoter polymorphism in psychiatric disorders. Am J Med Genet 105(2):168–171
Vigod S, Kurdyak P, Dennis C, Gruneir A, Newman A, Seeman M et al (2014) Maternal and newborn outcomes among women with schizophrenia: a retrospective population-based cohort study. BJOG Int J Obstet Gynaecol 121(5):566–574
Acknowledgements
We thank patients for their help. We also acknowledge Science and Research Branch, Islamic Azad University, for providing laboratory.
Funding
There was no funding to support this study.
Author information
Authors and Affiliations
Contributions
MMM contributed to laboratory work and sample collection, ZN contributed to conceptualization and design of project and data analysis, IS contributed to data analysis, NMH contributed to psychiatric examination. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethic approval and consent to participate
The project proposal was reviewed by the Ethics Committee of the Islamic Azad University, Science and Research Branch, and was approved with the ID number IR.IAU.SRB.REC.1397.045. The informed consent was obtained from control and case groups or their supervisors.
Consent for publication
Not applicable.
Competing interests
There is no competing of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Chi square analysis based on age and uVNTR repeats in two gender groups. Table S2. Chi square analysis based on ethnics and uVNTR repeats in two gender groups.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mardani Moghanaki, M., Noormohammadi, Z., Salahshourifar, I. et al. MAOA-uVNTR variations in schizophrenia: case and control study. Bull Natl Res Cent 46, 262 (2022). https://doi.org/10.1186/s42269-022-00951-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-022-00951-5