Abstract
Background
Microscopic abnormalities are common findings on routine urinalysis performed for various clinical reasons. As a small proportion of these may indicate an underlying malignancy, a large number of patients with these abnormalities are referred for further investigations, which includes a cystoscopy. We aim to investigate the diagnostic utility of cystoscopy in detecting malignancy in this group of patients.
Methods
A retrospective review of patients who underwent standard diagnostic workup for microscopic abnormalities of urinalysis (microscopic haematuria, sterile pyuria and bacteriuria) between January 2013 and December 2018 was performed. Patients with macroscopic haematuria, concurrent UTI, recent kidney stone passage, dysmorphic red cells, proteinuria and casts on urinalysis were excluded. Demographic information, age at diagnosis, smoking status and final diagnosis were extracted.
Results
In total, 552 patients identified. 58% of the patients are males (319 patients). The mean age was 61 years with 35% patients having a history of smoking. 94% of the patients underwent pre-cystoscopy imaging. Twelve (2%) patients had a final diagnosis of genitourinary malignancy. Out of the 12 patients diagnosed with malignancy, pre-cystoscopy imaging detected a bladder lesion in 11 (92%) patients.
Conclusions
The incidence of genitourinary malignancy in patients with persistent microscopic abnormalities of urinalysis is low at 2%. In our cohort, flexible cystoscopy demonstrated little additional diagnostic value with only 1 malignancy (0.2%) detected by flexible cystoscopy alone. Hence, we may have to reconsider our current threshold in investigating this group of patients.
Similar content being viewed by others
Background
Microscopic haematuria, sterile pyuria and bacteriuria are common findings on routine urinalysis performed in the community for various clinical indications with an estimated prevalence between 0.19% and 16% (Thompson 1987; Woolhandler 1989). Although the most common aetiology underlying these finding are benign, clinicians must be aware that persistent abnormalities in urinalysis may be a harbinger of malignant genitourinary disease. In 2006, Edwards et al. found that in patients with genitourinary malignancy, approximately 4.8% presented with microscopic haematuria (Edwards et al. 2006).
Annually a large numbers of patients are referred to urology clinics for further investigations. As part of their workup, patients usually undergo renal tract imaging, in the form of an ultrasound or a computed tomograhy (CT) urogram, as well cystoscopy. There are currently several guidelines on how best to investigate these patients. In 2012, the American Urology Association (AUA) published their latest best practice policy which states all patients with asymptomatic microscopic haematuria above the age of 35 should undergo a CT urogram as well as a cystoscopy (Davis et al. 2012). The National Institute for Health and Care Excellence (NICE) guidelines, in contrast, only suggested an urgent referral for microscopic haematuria for patients above the age of 60 and in the presence of dysuria or an elevated serum white cell count (Recommendations Organised by Site of Cancer 2020). The Canadian Urologic Association suggests mandatory cystoscopy in all patients with asymptomatic microscopic haematuria above the age of 40 (Wollin et al. 2013). Despite their differences, one common component in these guidelines is that the majority of patients should undergo cystoscopy as part of their workup.
Whilst cystoscopy is currently is a universal recommendation in the standard diagnostic workup for persistent microscopic abnormalities of urinalysis, there needs to be a balance between excessive usage of resources, potential harms from cystoscopy and the risk of missing a significant pathology. We hypothesises that a higher threshold for performing cystoscopy is possible without compromising the detection of malignancy. The aim of this study is to assess the diagnostic utility of cystoscopy in detecting genitourinary malignancy amongst patients who presents with persistent microscopic abnormalities of urinalysis.
Methods
We retrospectively reviewed the database at our tertiary urology referral centre for patients who underwent standard diagnostic workup for persistent microscopic urine abnormalities (microscopic haematuria, sterile pyuria and bacteriuria) between January 2013 and December 2018. A standard diagnostic workup includes imaging of the renal tract (ultrasound renal tract and/or CT urogram) followed by clinical assessment and a local anaesthetic flexible cystoscopy. All patients underwent urine microscopy to assess the presence of red blood cell and its characteristics. Patients with dysmorphic red cells, proteinuria or casts in their urinalysis were excluded from the study. Patients with recent kidney stone passage and concurrent urinary tract infection were also excluded from the study.
In this study, microscopic haematuria is defined as the presence of more than 20 × 106 per L red blood cells in a single urine sample, sterile pyuria is defined as the presence of elevated numbers of white cells (> 10 × 106 per L) in a urine sample that appears sterile using standard culture and contaminated urine is defined as the presence of more than 10 × 10 6 per L of epithelial cells. All the definitions were obtained from the local tertiary hospital guidelines. Bacteriuria, as the name implies, is the presence of bacteria in the urine. All patients with self-reported history of visible haematuria were excluded from the study. Demographic information, age at diagnosis, smoking history and final diagnosis were recorded for all patients.
Results
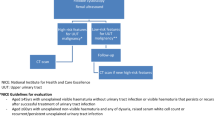
From January 2013 to December 2018, a total of 552 patients completed standard diagnostic workup and met the inclusion criteria. Figure 1 illustrates the patient selection algorithm. The cohort was made up of 319 male (58%) patients and 233 female (42%) patients. The mean age of this cohort was 61 years, with 35% of the patients having a history of smoking. The majority of patients were asymptomatic (77%) and the remaining 127 (23%) patients had a documented history of lower urinary tract symptoms around the time of their presentation. Majority of the patients underwent pre-cystoscopy imaging (94%). Ultrasound was performed in 360 patients, CT urogram in 77 patients and 87 patients underwent both forms of imaging. New Zealand European were the largest ethnic group (40%) followed by Pacific Islander (20%) and Maori (14%). A summary of the demographics is illustrated in Table 1.
Urinalysis
A total of 1156 urinalysis was performed prior to Urology referral. In total, 208 patients had 3 urinalysis performed, 190 patients had 2 urinalysis performed and 151 patients had 1 urinalysis performed. Three patients had no evidence of urinalysis performed. The results of the each urinalysis are as illustrated in Table 2. A total of 268 patients had at least one urinalysis revealing microscopic haematuria. The rest of the patients have at least one urinalysis showing sterile pyuria, bacteriuria or sterile pyuria and microscopic haematuria.
Outcome
Flexible cystoscopy identified 13 patients with bladder lesion. Twelve of these patients were subsequently confirmed to have a malignant lesion, and the remaining patient was diagnosed with cystitis cystica. The rate of bladder cancer was 3.1% and 0.9% in males and females, respectively. The youngest male and female diagnosed with bladder cancer were 52 and 60 years old, respectively. A total of 5 patients (42%) were either current or ex-smokers. All the patients diagnosed with malignancy had no urinary symptoms on their initial referral.
The final histology for the 12 patients was non-muscle invasive bladder cancer (7 pTa high grade, 3 pTa low grade, one died from a presumed unrelated malignancy whilst awaiting resection) and one was diagnosed with prostate cancer. Of the 12 patients, 3 had at least one urine sample showing microscopic haematuria, 6 had microscopic haematuria and sterile pyuria, 2 had sterile pyuria and 1 had bacteriuria. Overall 3.4% (9/262) of patients with MH and 1% (3/290) of patients with other microscopic abnormalities of urinalysis were diagnosed with a malignancy.
Out of the 12 patients diagnosed with malignancy, pre-cystoscopy imaging detected a bladder lesion in 11 (92%) patients. Four of these patients underwent an ultrasound, 1 patient underwent a CT and 6 patients underwent both forms of imaging. Flexible cystoscopy only identified one additional case of malignancy (0.2%) which was not picked up on pre-cystoscopy imaging and this patient had a low-grade pTa lesion. The data for patients diagnosed with malignancy are summarised in Table 3. Although the number of malignancies were very low, men were more likely to be diagnosed with malignancy (p = 0.06); however, there was no difference between malignancy rates for older patients or those with history of smoking.
Discussion
Microscopic haematuria and other microscopic abnormalities of urine are common findings on routine urinalysis performed in the community for various clinical indications. Most current guidelines suggest relatively resource intensive secondary investigations. Our study suggests that in majority of the patients a more truncated approach may be safe and efficacious.
Our retrospective review has revealed a low rate of malignancy in patients with microscopic haematuria (2%) in line with recent publications (Jung et al. 2010; Samson et al. 2018). In their retrospective review of patients undergoing standard diagnostic workup for asymptomatic microscopic haematuria, Gonzalez et al. identified 25 patients with bladder cancer (1.2%) (Gonzalez et al. 2019). The final pathology for all patients was non-muscle invasive bladder cancer. Samson et al. in 2017 conducted a retrospective analysis on 1049 patients with asymptomatic haematuria and this revealed 6 patients all with non-muscle invasive bladder cancer (0.57%) (Samson et al. 2018). Similarly the final pathology report for all the patients diagnosed with malignancy in our cohort was non-muscle invasive bladder cancer. A recent prospective study of 3556 patients by Tan et al. has revealed similar rates of diagnosis of genitourinary malignancy in patients with microscopic haematuria (3.1%) (Tan et al. 2018a). Interestingly this particular cohort has a significant number of patients diagnosed with muscle invasive bladder cancer (31.3%) amongst patients with microscopic haematuria, and of these patients, one was below the age of 60. The stated studies above have not reported whether cystoscopy led to additional findings beyond what pre-cystoscopy imaging had identified. This is the main point of difference in our study.
One unique feature of our study is that secondary to our outpatient triage protocols, all patients will undergo radiological imaging prior to clinic assessment and cystoscopy. Our retrospective analysis has revealed that coupled with renal tract imaging, cystoscopy provided little additional diagnostic utility with only 1 malignancy (0.2%) detected by flexible cystoscopy alone. Although easy to perform, cystoscopy is invasive, uncomfortable, expensive and consumes significant amount of clinical resources. Issues such as lethargy, dysuria, haematuria and suprapubic pain were common post-cystoscopy (Erkal 2007). Complications such as UTIs can also be significant. The previous literature has published rates of UTI between 2 and 7.5% (Herr 2015; Clark and Higgs 1990). This is further highlighted in the AUA best practice guidelines, in which patients with risk factors for a UTI are recommended to have prophylaxis antibiotics (Wolf et al. 2008). Another important consideration regarding cystoscopy is that it is costly. Halpern et al. in 2017 illustrated this in their decision analytic model to determine the most cost-effective method in investigation asymptomatic haematuria (Halpern et al. 2017). Based on the Medicare Physician Fee Schedule, the cost of cystoscopy alone from the payer’s perspective ranged from $166-$285. The incremental cost of cancer detected for cystoscopy alone was $10 287 (Halpern et al. 2017).
Apart from deciding who needs to be investigated, another issue that faces many urologist is how best to image the renal tract. The recent AUA guidelines suggested the use of CT Urogram as a first line imaging of choice for microscopic haematuria (Davis et al. 2012). Patients who have absolute or relative contraindication to a CT Urogram can be imaged with either a magnetic resonance Urogram or an Ultrasound, in descending order of preference (Davis et al. 2012). In our cohort, 10 out of the 12 patients with malignancy had bladder mass picked up on pre-cystoscopy ultrasound. Only one patient with a normal ultrasound was subsequently diagnosed with pTa bladder malignancy. CT only detected one additional case of malignancy in our cohort. In 2011, Cauberg et al. conducted a prospective review on types of renal tract imaging and found that ultrasound is sufficient to exclude significant upper tract disease in patients with microscopic haematuria (Cauberg et al. 2011). Lisanti et al. has also previously shown that CT Urogram provided no additional benefit over non-enhanced CT in evaluating the upper renal tract in patients with microscopic haematuria (Lisanti et al. 2014). Additionally, previous studies have highlighted the implications of non-urologic CT findings such as added cost and morbidity from invasive tests and treatments (Morgan et al. 2015; Lai et al. 2016).
More recently, the usage of novel urinary biomarkers has been reported to have a high sensitivity and negative predictive value (Tan et al. 2018b). However, to date, these markers are not considered to be a first line investigation tool and are not to be used without cystoscopy (Tan et al. 2018b). Apart from that, the emerging use of CxBladder may offer an alternative in investigating microscopic haematuria. A recent study has revealed a high negative predictive value of 97.4% and 35% of patients avoided cystoscopy (Konety et al. 2019).
Whilst there is ongoing debate regarding the gold standard workup, our results suggests that not all patients with persistent microscopic abnormalities of urinalysis necessarily need to undergo cystoscopy. In our cohort of 552 patients who completed workup, 3.4% of those with microscopic haematuria and 1% of those with other urinalysis abnormalities were diagnosed with malignancy. This is similar to the DETECT I reports with a rate of malignancy of 3.1% amongst patients with microscopic haematuria (Tan et al. 2018a). Although the variables that we analysed (age, smoking status, gender) did not reach any statistically significant results, this may be explained due to our small patient number. This is supported by the fact that multiple reviews has previously shown that older age, male gender and positive smoking status are significantly associated with the risk of underlying malignancy (Davis et al. 2012; Samson et al. 2018; Gonzalez et al. 2019). Based on the literature, a cystoscopy should strongly be considered in elderly male with a history of smoking. Younger patients may not need to undergo a cystoscopy; however, decision should be made after reviewing the presence of other symptoms as well as risk factors. For instance, there might be a benefit in performing a cystoscopy in low risk populations to assist the diagnosis of non-malignant pathology such as benign prostatic enlargement or urethral stricture (Gonzalez et al. 2019). Ultimately, the decision of who should undergo a cystoscopy should be individualised and this needs to be discussed between the treating physician and patient. Our study does not mean that we do not advocate for investigation of urinalysis abnormalities; however, we suggest that with improved contemporary imaging there may be less need to for routine cystoscopy as a diagnostic tool. Furthermore, by only utilising cystoscopy on selected patients and cases, this will render it to be more cost-effective.
Our analysis has several limitations that should be mentioned. Our data collection was limited to a single tertiary referral centre; hence, our results may not be generalisable to the wider population. Additionally, our review was a cross-sectional study; no long-term follow-up was performed. This is crucial as patients with microscopic haematuria with initial negative evaluation still have a 1–3% of developing cancer over time (Wieder 2010).
Conclusions
As expected the incidence of malignancy in patients who presents with persistent abnormality in urinalysis is low at 2%. In our cohort, flexible cystoscopy demonstrated little additional diagnostic value with only 1 malignancy (0.2%) detected by flexible cystoscopy alone. Given the high frequency of abnormal urinalysis sample in the community coupled with the logistics, costs and resources necessary for a cystoscopy, we may have to reconsider our current threshold in utilising flexible cystoscopy in patients with persistent microscopic abnormalities of urinalysis. The ultimate goal is balancing the risk of potentially missing a diagnosis of cancer versus excessive usage of resources.
Availability of data and materials
Data are presented in the main paper.
Abbreviations
- CT:
-
Computed tomography
- AUA:
-
American Urology Association
- NICE:
-
National Institute for Health and Care Excellence
References
Cauberg E, Nio C, de la Rosette J, Laguna M, de Reijke T (2011) Computed tomography-urography for upper urinary tract imaging: is it required for all patients who present with hematuria? J Endourol 25(11):1733–1740
Clark K, Higgs M (1990) Urinary infection following out-patient flexible cystoscopy. Br J Urol 66(5):503–505
Davis R, Jones J, Barocas D, Castle E, Lang E, Leveillee R et al (2012) Diagnosis, evaluation and follow-up of asymptomatic microhematuria (AMH) in adults: AUA guideline. J Urol 188(6S):2473–2481
Edwards T, Dickinson A, Natale S, Gosling J, Mcgrath J (2006) A prospective analysis of the diagnostic yield resulting from the attendance of 4020 patients at a protocol-driven haematuria clinic. BJU Int 97(2):301–305
Erkal S (2007) Patients’ experiences at home after day case cystoscopy. J Clin Nurs 16:1118–1124
Gonzalez A, Lipsky M, Li G, Rutman M, Cooper K, Weiner D et al (2019) The prevalence of bladder cancer during cystoscopy for asymptomatic microscopic hematuria. Urology 126:34–38
Halpern J, Chughtai B, Ghomrawi H (2017) Cost-effectiveness of common diagnostic approaches for evaluation of asymptomatic microscopic hematuria. JAMA Intern Med 177(6):800
Herr H (2015) The risk of urinary tract infection after flexible cystoscopy in patients with bladder tumor who did not receive prophylactic antibiotics. J Urol 193(2):548–551
Jung H, Gleason J, Loo R, Patel H, Slezak J, Chien G et al (2010) APP-081 Association of hematuria on microscopic urinalysis and risk of urinary tract cancer development. Jpn J Urol 101(2):221
Konety B, Shore N, Kader A, Porten S, Daneshmand S, Lough T et al (2019) Evaluation of Cxbladder and Adjudication of Atypical Cytology and Equivocal Cystoscopy. Eur Urol 76(2):238–243
Lai W, Ellenburg J, Lockhart M, Kolettis P (2016) Assessing the costs of extraurinary findings of computed tomography urogram in the evaluation of asymptomatic microscopic hematuria. Urology 95:34–38
Lisanti C, Toffoli T, Stringer M, DeWitt R, Schwope R (2014) CT evaluation of the upper urinary tract in adults younger than 50 years with asymptomatic microscopic hematuria: is IV contrast enhancement needed? Am J Roentgenol 203(3):615–619
Morgan A, Berland L, Ananyev S, Lockhart M, Kolettis P (2015) Extraurinary incidental findings on CT for hematuria: the radiologist’s role and downstream cost analysis. Am J Roentgenol 204(6):1160–1167
Recommendations organised by site of cancer | Suspected cancer: recognition and referral | Guidance | NICE. Nice.org.uk. 2020 [cited 4 December 2020]. https://www.nice.org.uk/guidance/ng12/chapter/1-Recommendations-organised-by-site-of-cancer.
Samson P, Waingankar N, Shah P, Friedman D, Kavoussi L, Han J (2018) Predictors of genitourinary malignancy in patients with asymptomatic microscopic hematuria. Urol Oncol Semin Orig Invest 36(1):10.e1-10.e6
Tan W, Feber A, Sarpong R, Khetrapal P, Rodney S, Jalil R et al (2018a) Who should be investigated for haematuria? Results of a contemporary prospective observational study of 3556 patients. Eur Urol 74(1):10–14
Tan W, Tan W, Tan M, Khetrapal P, Dong L, deWinter P et al (2018b) Novel urinary biomarkers for the detection of bladder cancer: a systematic review. Cancer Treat Rev 69:39–52
Thompson I (1987) The evaluation of microscopic hematuria: a population-based study. J Urol 138(5):1189–1190
Wieder JA. Pocket guide to urology, 4th ed. Wieder Medical: [Caldwell, Idaho]: in association with Griffith Publishing, 2010.
Wolf J, Bennett C, Dmochowski R, Hollenbeck B, Pearle M, Schaeffer A (2008) Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol 179(4):1379–1390
Wollin T, Laroche B, Psooy K (2013) Canadian guidelines for the management of asymptomatic microscopic hematuria in adults. Can Urol Assoc J 3(1):77
Woolhandler S (1989) Dipstick urinalysis screening of asymptomatic adults for urinary tract disorders. JAMA 262(9):1214
Acknowledgements
Not applicable.
Funding
None to declare.
Author information
Authors and Affiliations
Contributions
ZMAZB performed data collection, data analysis as well as writing the initial and final draft. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This review has been assessed by the Health and Disability Ethics Committees (HDEC) of New Zealand and has been deemed as “out of scope” and does not require HDEC approval.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zainal Bahren, Z.M.A. The diagnostic utility of cystoscopy in assessing patients with persistent microscopic abnormalities of urinalysis. Bull Natl Res Cent 46, 104 (2022). https://doi.org/10.1186/s42269-022-00777-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-022-00777-1