Abstract
Background
Gastroenteritis is a common infectious disease in children, which results in high mortality and morbidity, especially in resource-poor countries. This study presents the selected main gastroenteritis causing bacteria, including Escherichia coli O157, Salmonella and Shigella species delineating their prevalence and resistance pattern to the clinically used antibiotics.
Results
A total of 346 stool specimens from children of clinically suspected gastroenteritis below five years have been obtained, and bacterial pathogens were recovered using selective media, biochemical and serologic tests. We found that 35 (10%) of them were confirmed bacterial gastroenteritis (BGE) with either Escherichia coli O157 (14%), Salmonella spp. (43%), and Shigella spp. (43%). Nevertheless, the prevalence of E. coli O157, Salmonella spp., and Shigella spp. in this study were documented as 1.45%, 4.34%, and 4.34%, respectively. Moreover, 2 (40%) of E. coli O157, 4 (26.67%) of Salmonella spp., and 14 (93%) of the Shigella spp. were found as multidrug-resistant. Nonetheless, Shigella spp. isolates showed 100%, 87%, and 73% resistance to cotrimoxazole, ciprofloxacin, and azithromycin respectively, while E. coli O157 showed 80% resistance to cotrimoxazole and 60% to ciprofloxacin and azithromycin. On the contrary, cotrimoxazole, ciprofloxacin, azithromycin, and tetracycline were resistant in 40%, 47%, 27%, and 53% of Salmonella spp. isolates respectively.
Conclusion
These findings generate significant insights on the prevalence and antibiotic resistance of the three major gastroenteritis causing bacteria in the study area. Therefore, it will help physicians and policymakers selecting the right antibiotics in essential cases, particularly, reevaluation of recommending cotrimoxazole, ciprofloxacin, and azithromycin in the management of bacterial gastroenteritis.
Similar content being viewed by others
Background
Diarrhea or vomiting resulting from inflammation in the colon or upper small bowel could be referred as gastroenteritis. Etiologic agents might be viruses, bacteria, or parasites, but no pathogens are recovered in many cases. Bacteria cause 20–40% of diarrhea in the United Kingdom (Tam et al. 2012), though they mostly play a role in developing countries where childhood mortality resulting from diarrheal diseases is mostly happened (Guerrant et al. 2013). Shigella spp., enterotoxigenic E. coli, Vibrio spp., and Salmonella spp. are the most common causes of bacterial gastroenteritis in developing countries (O'Ryan et al. 2014), even though etiologic agents may vary with geographical region. World Health Organization (WHO) documented that gastroenteritis caused 477,293 (8%) deaths of children under five years in 2016 globally (WHO 2016). Worldwide, around 68% of diarrheal disease has been documented in young children taking 2.5 million lives, and it is recognized as the fifth top reason for child mortality (Hartman et al. 2019). In children under five years, acute gastroenteritis (AGE) is a principal cause of mortality and morbidity, 19% of deaths and 10% of hospital admission (Oppong et al. 2020) in resource-poor countries where proper hygiene, sanitation, potable water is deficient, and contaminations from food products are high (Farfán-García et al. 2020).
In developing countries, around half a million deaths of infants and young children happened due to AGE, where Shigella is the top etiologic agent (Kotloff 2017). In China, Shigella was found as the most frequent bacterial agent causing AGE (Wang et al. 2015), whereas, in India, E. coli has been recognized as the dominant (31%), followed by Shigella (24%) (Shrivastava et al. 2017; Bruzzese et al. 2018). Worldwide, in 2013, the deaths of children below five years due to shigellosis have been documented between 28,000 to 48,000 (Williams and Berkley 2018). Shigella flexneri and Shigella sonnei are the most frequent species causing infections. Shigella dysenteriae, which produces Shiga toxin recognized as a highly virulent strain, could cause epidemics with high mortality in developing countries. A high level of drug resistance, especially to ciprofloxacin and azithromycin, was observed in those outbreaks (Barrett and Fhogartaigh 2017).
According to an estimation, nontyphoidal (NTS) Salmonella are responsible for 93.8 million cases of gastroenteritis and 155,000 deaths globally per annum (Majowicz et al. 2010). A proportion of childhood diarrhea and travelers' diarrhea (TD) in developing countries are occurred by NTS, where Salmonella enterica var. Typhimurium and var. Enteritidis are frequently recovered (Barrett and Fhogartaigh 2017). A study in China revealed that diarrheagenic E. coli (5%) and Salmonella spp. (8%) were responsible for acute diarrhea in children below five years (Tian et al. 2016). Shiga toxin-producing Escherichia coli (STEC) O157 is a public health concern due to having potential for severity though it rarely caused gastroenteritis (Adams et al. 2016). Nevertheless, STEC O157: H7 is broadly distributed in the environment and foods, and humans typically get infected by contaminated food and drink or direct exposure with animals (Ahmed et al. 2017). Moreover, the expression of different virulence factors, extended survival capability in the environment, low infective dose, and challenges to treatment made STEC O157: H7 an enteric pathogen of principal concern around the world (Lupindu 2018).
Globally, antibiotic resistances have been increasing the risk of morbidity, mortality and economic burden, where developing countries are the primary victim due to the over and unnecessary uses of antibiotics, drugs with compromised quality, misuse of antibiotics in poultry and cattle feed, lack of continuous effective surveillance, and poverty (Chowdhury et al. 2015). The emergence of antibiotic-resistant E. coli O157 has been documented in different parts of the world in recent years. Over the past several decades, various strains of Salmonella spp. and Shigella spp. became resistant to the most widely used antibiotics with increasing frequency (Barrett and Fhogartaigh 2017). In bacterial gastroenteritis, investigations on causative agents and antibiotic treatment are generally not required. Recommendation of antibiotics is given to critically ill children having chronic conditions of particular risk factors. Types and regimens of antibiotics should be considered based on patient conditions, suspected bacteria, and local epidemiology (Buzesse et al. 2018). Importantly, antibacterial resistance data also have to be taken into consideration before selecting antibiotics. Thus, to reduce mortality, morbidity, and healthcare expense caused by BGE, the local pattern of bacterial resistance is considerably essential (Buzesse et al. 2018).
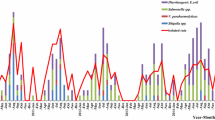
To delineate the prevalence and antibiotic resistance pattern of the three major gastroenteritis causing bacteria, E. coli O157, Salmonella spp., and Shigella spp., in children below five years of age, we have conducted a cross-sectional study in two hospitals of Chattogram district in Bangladesh from September 2017 to July 2018.
Methods
Patient selection
Children under five years of age, both male and female, exhibited acute gastroenteritis symptoms and were admitted to Chattogram Maa-O-Shishu General Hospital's diarrheal ward and Chattogram Upazila Health Complex Patiya, Chattogram were selected for this study employing a simple random sampling method. The ward's responsible physician has diagnosed the gastroenteritis in patients according to the definition of World Health Organization (WHO) as "who have diarrhea more than three times per day, with abnormal stool specimen such as watery stool, loose stool, mucus and blood in stool" (WHO 2017).
Ethical consideration
We have taken written permission from the ethical committee of the Department of Microbiology at the University of Chittagong to conduct the study, and written consent has been taken from the patient's attended guardian with informing aims and objectives, merits, and demerits of participation in the study.
Specimen collection
Fresh stool specimens were collected in sterile plastic vials and placed in an insulated box at 4 °C and transported to the laboratory at the Microbiology department, of the University of Chittagong, or Industrial Microbiology Division, Bangladesh Council of Scientific and Industrial Research (BCSIR), Chattogram.
Isolation and identification of bacteria
The stool specimen was enriched in Luria–Bertani broth (Himedia, India) for 24 h at 37 °C, and broth culture was then inoculated onto Salmonella-Shigella agar (Himedia, India) and Hektoen enteric agar (Himedia, India) plates. The plates were incubated for 24 h at 37 °C. Individually recognizable colorless colonies onto Salmonella-Shigella agar plates were primarily selected as Salmonella or Shigella species. Motile isolates that were indole negative, citrate positive, produced red alkaline slant and yellow acidic butt with black colored H2S generation in triple sugar iron (TSI) agar were confirmed as Salmonella spp. Conversely, isolates that were non-motile, indole positive, citrate negative, and produced red alkaline slant and yellow acidic butt without H2S generation were confirmed as Shigella spp. (Assefa and Girma 2019). On the contrary, green or blue-green, moist, and raised colonies on Hektoen agar plates were presumptively identified as Shigella spp., while colonies with green or blue-green color with or without black center were recognized as Salmonella spp. (Assefa and Girma 2019).
Furthermore, for the isolation of E. coli O157, the stool specimen was inoculated in modified tryptone soya broth containing novobiocin (Lab M, UK) for 24 h at 37 °C for the selective enrichment. Then, broth culture was streaked on cefixime-tellurite sorbitol MacConkey agar (CT-SMAC) (Lab M, UK) plates and incubated at 37 °C for 24 h. Colorless bacterial colonies on CT-SMAC agar were primarily selected as E. coli 0157 and then confirmed with slide agglutination with the E. coli O157 Latex test kit (Oxoid, UK).
Antibiotic susceptibility test
Antibiotic susceptibility test (AST) was performed by standard Kirby-Bauer disc diffusion method according to Clinical and Laboratory Standards Institute guidelines (CLSI 2018). The antibiotic discs of azithromycin (15 µg), chloramphenicol (30 µg), cotrimoxazole (25 µg), tetracycline (30 µg), doxycycline (30 µg), and ciprofloxacin (5 µg) (Oxoid, UK) were used in this study. The zone of inhibition for each antibiotic was measured in millimeters, and on the basis of the inhibitory zones, isolates were classified as sensitive, intermediate, and resistant (CLSI, 2018). Isolates resistant to one or more drugs in three or more classes of antibiotics are recognized as multidrug-resistant (MDR) (Magiorakos et al. 2012; Rahman et al. 2021).
Results
In this study, a total of 346 watery stool specimens (single specimen from each child) were obtained from children below five years of age, who were clinically suspected as gastroenteritis attended in the two study hospitals, and 10% (35/346) of them were infected with either one of the three targeted bacteria, Shigella spp. (n = 15, 43%), Salmonella spp. (n = 15, 43%), and E. coli O157 (n = 5, 14%), and termed as "positive with bacterial gastroenteritis (BGE)." The BGE positive cases' median age was 11 months, and 28 (80%), 5 (14.29%), and 2 (5.71%) cases are aged < 1, 1–2, and > 2–4 years, respectively. Moreover, 53% (19) of them were female, and 47% (16) were male. The prevalence of BGE caused by Shigella spp., Salmonella spp., and E. coli O157 was documented as 4.34% (15/346), 4.34% (15/346), and 1.45% (5/346), respectively (Table 1).
Over half (57%) of the isolates causing BGE were resistant to three or more antibiotics tested in this study and recognized as multidrug-resistant. Alarmingly, 14 (93%) of the Shigella spp. 4 (26.67%) of Salmonella spp. and 2 (40%) of E. coli O157 were found as multidrug-resistant (Table 1). Shigella spp. revealed a high level of drug resistance; 100% to cotrimoxazole, 87% to ciprofloxacin, 73% to azithromycin, 40% to tetracycline, and 20% to chloramphenicol and doxycycline. Moreover, Salmonella spp. showed resistance to six out of six tested antibiotics as 53% to tetracycline, 40% to cotrimoxazole, 47% to ciprofloxacin, 27% to azithromycin, and 7% to both chloramphenicol and doxycycline. Another isolate E. coli O157 showed 80% resistance to cotrimoxazole, 60% to ciprofloxacin and azithromycin, and 20% to tetracycline, chloramphenicol and doxycycline (Table 2).
Discussion
A study by Web and Starr (2005) reported that 15% of gastroenteritis were caused by E. coli, Salmonella, Shigella, and Campylobacter species, whereas, in our study, the prevalence of bacterial gastroenteritis (BGE) caused by Shigella spp., Salmonella spp., and E. coli O157 was recorded as 10%. Shigella species caused gastroenteritis in pediatric patients in central Iran has been reported by Abbasi et al. (2019); out of the 230 samples, Shigella spp. were identified by culture and PCR as 8.2% and 11.3%, respectively; wherein the most frequent species were S. flexneri (21%), and S. sonnei (78.9%). In acute gastroenteritis cases, the prevalence of Shigella has been documented in Tehran, Iran (Rahbar et al. 2007), Kerman, Iran (Nave et al. 2016), Ethiopia (Roma et al. 2000), North of Ethiopia (Kahsay and Teklemariam 2015), and Tanzania (Temu et al. 2007) as 46.5%, 9%, 34.6%, 13.3%, and 14%, respectively. Similar studies conducted in Kerman, Iran (Nave et al. 2016) and the North of Ethiopia (Kahsay and Teklemariam 2015) reported 9% and 13.3% frequencies. On the contrary, studies conducted in India reported frequencies around 2% (Aggarwal et al. 2016). In countries such as Nigeria (25%) (Abdu et al. 2014), Ethiopia (54%) (Debas et al. 2011), and Ghana (70.8%) (Opintan and Newman 2007), the most common species was S. flexeneri (Mahmoudi et al. 2017). These shigellosis variations could be due to age, economic growth, geographical location, temperature, and several other environmental factors (Abbasi et al. 2019). In contrast, Shigella spp.'s prevalence in our study is relatively low (4.34%).
The prevalence of Salmonella spp. in our study has been recorded as 4.3%, in contrast, other studies conducted in Iran (Mahmoudi et al. 2017), Harar (eastern Ethiopia) (Reda et al. 2011), Mozambique (Mandomando et al. 2007), Palestine (Elamreen et al. 2007), and Ethiopia (Mengistu et al. 2014) reported the prevalence of Salmonella spp. was 42%, 42.8%, 2.5%, 2%, and 10.5%, respectively.
In parts of Europe, Japan, and North America, most outbreaks of gastroenteritis are because of enterohemorrhagic E. coli serotype O157: H7, though other serotypes are significantly remained health concerns in the rest of the developed countries. E. coli O157 and Shiga toxin-producing E. coli (STEC) were not commonly found in Bangladesh (Islam et al. 2007). Our study also found BGE positive cases of E. coli O157 were relatively lower (14%, 5/35) than the other two bacteria. The prevalence of E. coli O157 in this study was 1.45%, lower than the other two bacteria. In contrast, a prevalence of over 7% of STEC O157: H7 was reported in the diarrheal patient of Morogoro, Tanzania in 2006 (Raji et al. 2008), whereas 3.4% of isolates were STEC E. coli O157: H7 found in Tunisia (Al-Gallas et al. 2006). Similar studies in Nigeria reported a prevalence of 6% (Olorunshola et al. 2000) in Lagos and 5.4% (Chigor et al. 2010) in Zaria. The pathogen was responsible for diarrhea in children at a proportion of 1.9% in Mozambique (Mandomando et al. 2007; Lupindu 2018).
The emergence of multidrug-resistant (MDR) Shigella spp. is a progressive concern worldwide (Zamanlou et al. 2018). As shigelloses are highly infectious, it is necessary to know the disease's occurrence and antimicrobial susceptibility of the strains to ensure proper clinical care and patient management (Singh et al. 2011). Mild symptoms are self-limited, but antibiotics are prescribed in extreme dysentery cases to shorten the duration of diarrhea (Williams and Berkley 2018). In our study, Shigella spp. showed resistance to cotrimoxazole (100%), ciprofloxacin (87%), azithromycin (73%), chloramphenicol (20%), tetracycline (40%), and doxycycline (20%). Ciprofloxacin-resistant S. dyseteriae 1 first found in Bangladesh in 2003, but S. boydii and S. flexneri were documented in 2007 and 2008, respectively (Talukder et al. 2006; Khatun et al. 2011). Other studies from Bangladesh also revealed that ciprofloxacin-resistant S. sonnei was about 10% in 2007, but in 2011 it was increased by sevenfold (Ud-Din et al. 2013). Zamanlou et al. (2018) reported that 4.2% of Shigella spp. showed resistance to ciprofloxacin in Tabriz, Iran. In contrast, 56.2% of S. flexneri were also resistant to the antibiotic has been documented in India (Aggarwal et al. 2016). A study conducted in Bangladesh between 2001 to 2011 documented that Shigella spp. were resistant to trimethoprim-sulfamethoxazole (89.5%), nalidixic acid (86.5%), mecillinam (10.5%), and ampicillin (9.5%), respectively (Ud-Din et al. 2013). The other study from Bangladesh also stated that 248 (69%) Shigella strains showed resistance to cotrimoxazole (Talukder et al. 2003). The study conducted by Abbasi et al. (2019) revealed that cotrimoxazole (100%), ampicillin (84.2%), cefixime (68.4%), ceftriaxone (63.1%), and ciprofloxacin (10.5%) were affected by Shigella resistance. World Health Organization (WHO) proposed fluoroquinolone (ciprofloxacin) as first-line therapy for all patients with bloody diarrhea without age restriction, and ceftriaxone is recommended as second-line therapy or alternative antibiotics in children and adults; because of resistance to trimethoprim-sulfamethoxazole, sulfonamides, ampicillin, and tetracycline (WHO 2019). In developing countries, MDR was rising in Shigella spp. mainly to azithromycin, fluoroquinolones, and third-generation cephalosporins (Li et al. 2016). The raised resistance level is mostly because of the horizontal transfer via plasmids, transposons, and integrons (Barrantes and Achí 2016). Though cotrimoxazole is broadly used in the empirical management of diarrheal diseases, and its widespread application has contributed to the emergence of resistance of Shigella spp. (Pourakbari et al. 2010). Previously, a high level of resistance to cotrimoxazole has been reported in Iran (92.2% to 94%) (Pourakbari et al. 2010; Nikfar et al. 2017) and Turkey (95%) (Kacmaz et al. 2014). Our findings were also consistent with their results that 100% of all Shigella spp. found resistant to the antibiotic. Mahmoudi et al. (2017) reported that the frequency of trimethoprim/sulfamethoxazole resistance among Shigella spp. was high (92%), which agrees with reports from Ethiopia (Asrat 2008). These results were similar to Mengistu et al. (2014), Savadkoohi and Ahmadpour-Kacho (Barari and Ahmadpour 2007), and Jomezadeh et al. (2014), which documented trimethoprim/sulfamethoxazole resistance rates of 76.5%, 73.8%, and 80.5%, respectively. These findings may indicate inappropriate antibiotic use in the recent decade (Mahmoudi et al. 2017).
Though rates of multidrug resistance (MDR) of Salmonella to traditional first-line agents in both Asia and Africa is increasing (Gordon et al. 2008), Leung et al. (2013) found a marked decline in MDR and decreasing resistance to the ampicillin, chloramphenicol, and cotrimoxazole but increasing resistance to ciprofloxacin in Bangladesh. In our study, Salmonella spp. were found resistant to tetracycline (53%), ciprofloxacin (47%), cotrimoxazole (40%), azithromycin (27%), chloramphenicol (7%), and doxycycline (7%). Several reports from around the world also showed the occurrence of a high level of ciprofloxacin-resistant isolates. The studies conducted by Mahmoudi et al. (2017), Mamuye et al. (2015), Mengistu et al. (2014), and Beyene et al. (2011) found the resistance of Salmonella isolates to trimethoprim/ sulfamethoxazole as 23%, 60%, 37.5%, and 31.5%, respectively.
We also documented that E. coli O157 isolates were resistant to cotrimoxazole (80%), ciprofloxacin (60%), azithromycin (60%), chloramphenicol (20%), tetracycline (20%), and doxycycline (20%). A study conducted by Chigor et al. (2010) in Nigeria found that E. coli O157 were resistant to cotrimoxazole (15%), ciprofloxacin (10%), chloramphenicol (5%), tetracycline (75%), ampicillin (65%), cefuroxime (50%), gentamicin (10%), nalidixic acid (55%), and nitrofurantoin (45%). Wilkerson et al. (2004) reported that 52% (15/29) of the resistant human E. coli O157 isolates were multidrug-resistant, including tetracycline. Another study reported that E. coli O157 isolates recovered from humans (n = 131) were resistant to trimethoprim-sulfamethoxazole (5%) and tetracycline (12%) (Schroeder et al. 2002).
Bacterial gastroenteritis is self-limiting; therefore, antibiotic therapy is only needed as an intervention to control BGE in infants, older people, and immunosuppressed patients, especially when bacteremia is suspected. Empiric therapy usually starts with oral cotrimoxazole or metronidazole, but parenteral treatment with ciprofloxacin or ceftriaxone could be preferred (Bruzzese et al. 2018).
Conclusions
This cross-sectional study delineated the prevalence of bacterial gastroenteritis in children below five years of age caused by the three significant pathogens Escherichia coli O157, Salmonella spp., and Shigella spp. in the Chattogram district of Bangladesh. The study findings revealed that the prevalence of those bacteria causing gastroenteritis is alarming. Preventive measures are highly recommended to reduce the disease burden and healthcare expense, eventually improving life quality. The findings of antibiotic resistance patterns will help physicians and policymakers select the right antibiotics where necessary, especially making a rational decision while choosing cotrimoxazole, ciprofloxacin, and azithromycin to manage bacterial gastroenteritis cases.
Availability of data and materials
All figures, graphs, and tables generated during this study are included in this manuscript.
References
Abbasi E, Abtahi H, van Belkum A, Ghaznavi-Rad E (2019) Multidrug-resistant Shigella infection in pediatric patients with diarrhea from central Iran. Infect Drug Resist 12:1535–1544
Abdu A, Aboderin AO, Elusiyan JB, Kolawole DO, Lamikanra A (2014) Serogroup distribution of Shigella in Ile-Ife, southwest Nigeria. Trop Gastroenterol 4(3):164–169
Adams NL, Byrne L, Smith GA, Elson R, Harris JP, Salmon R, Smith R, O’Brien SJ, Adak GK, Jenkins C (2016) Shiga toxin–producing Escherichia coli O157, England and Wales, 1983–2012. Emerg Infect Dis 22(4):590–597
Aggarwal P, Uppal B, Ghosh R, Prakash SK, Chakravarti A, Jha AK, Rajeshwari K (2016) Multi drug resistance and extended spectrum beta lactamases in clinical isolates of Shigella: a study from New Delhi India. Travel Med Infect Dis 14(4):407–413
Ahmed MO, Almshawt NF, Elnageh HR (2017) Diarrheagenic Escherichia coli O157 from Libya: recent perspectives and challenges. J Public Health Afr 8(1):685
Al-Gallas N, Bahri O, Aissa RB (2006) Prevalence of shiga toxin-producing Escherichia coli in a diarrheagenic Tunisian population, and the report of isolating STEC O157: H7 in Tunis. Curr Microbiol 53(6):483–490
Asrat D (2008) Shigella and Salmonella serogroups and their antibiotic susceptibility patterns in Ethiopia. East Mediterr Health J 14(4):760–767
Assefa A, Girma M (2019) Prevalence and antimicrobial susceptibility patterns of Salmonella and Shigella isolates among children aged below five years with diarrhea attending Robe General Hospital and Goba Referral Hospital, South East Ethiopia. Trop Dis Travel Med 5(1):1–11
Barari SKR, Ahmadpour KM (2007) Prevalence of Shigella species and their antimicrobial resistance patterns at Amirkola Children’s Hospital North of Iran. Iran J Pediatr 17(2):118–122
Barrantes K, Achí R (2016) The importance of integrons for development and propagation of resistance in Shigella: the case of Latin America. Braz J Microbiol 47(4):800–806
Barrett J, Fhogartaigh CN (2017) Bacterial Gastroenteritis. Medicine 45(11):683–689
Beyene G, Nair S, Asrat D, Mengistu Y, Engers H, Wain J (2011) Multidrug resistant Salmonella Concord is a major cause of salmonellosis in children in Ethiopia. J Infect Dev Ctries 5(1):23–33
Bruzzese E, Giannattasio A, Guarino A (2018) Antibiotic treatment of acute gastroenteritis in children. F1000Res 7:193–196.
Chigor VN, Umoh VJ, Smith SI, Igbinosa EO, Okoh AI (2010) Multidrug resistance and plasmid patterns of Escherichia coli O157 and other E. coli isolated from diarrhoeal stools and surface waters from some selected sources in Zaria, Nigeria. Int J Environ Res Public Health 7(10):3831–3841
Chowdhury MM, Kubra K, Islam MT, Rahman MM, Mehedy ME (2015) Indiscriminate uses of antibiotics as a threat to public health demand implementation of effective drug practices and enhancement of public awareness in Bangladesh. Eur J Res 133(2):187–195
CLSI, Clinical Laboratory Standards Institute, (2018) M100 Performance standards for susceptibility testing, 28th edn. Wayne, USA
Debas G, Kibret M, Biadglegne F, Abera B (2011) Prevalence and antimicrobial susceptibility patterns of Shigella species at Felege Hiwot Referral Hospital Northwest Ethiopia. Ethiop Med J 49(3):249–256
Elamreen FHA, Abed AA, Sharif FA (2007) Detection and identification of bacterial enteropathogens by polymerase chain reaction and conventional techniques in childhood acute gastroenteritis in Gaza Palestine. Int J Infect Dis 11(6):501–507
Farfán-García AE, Imdad A, Zhang C, Arias-Guerrero MY, Sánchez-Álvarez NT, Iqbal J, Hernández-Gamboa AE, Slaughter JC, Gómez-Duarte OG (2020) Etiology of acute gastroenteritis among children less than 5 years of age in Bucaramanga, Colombia: A case-control study. PLOS Negl Trop Dis 14(6):e0008375.
Gordon MA, Graham SM, Walsh AL, Wilson L, Phiri A, Molyneux E, Zijlstra EE, Heyderman RS, Hart CA, Molyneux ME (2008) Epidemics of invasive Salmonella enterica serovar Enteritidis and S. enterica Serovar Typhimurium infection associated with multidrug resistance among adults and children in Malawi. Clin Infect Dis 46(7):963–969.
Guerrant RL, DeBoer MD, Moore SR, Scharf RJ, Lima AA (2013) The impoverished gut—a triple burden of diarrhoea, stunting and chronic disease. Nat Rev Gastroenterol Hepatol 10(4):220–229
Hartman S, Brown E, Loomis E, Russell HA (2019) Gastroenteritis in children. Am Fam Physician 99(3):159–165
Islam MA, Heuvelink AE, De Boer E, Sturm PD, Beumer RR, Zwietering MH, Faruque AS, Haque R, Sack DA, Talukder KA (2007) Shiga toxin-producing Escherichia coli isolated from patients with diarrhoea in Bangladesh. J Med Microbiol 56(3):380–385
Jomezadeh N, Babamoradi S, Kalantar E, Javaherizadeh H (2014) Isolation and antibiotic susceptibility of Shigella species from stool samples among hospitalized children in Abadan Iran. Gastroenterol Hepatol Bed Bench 7(4):218–223
Kacmaz B, Unaldi O, Sultan N, Durmaz R (2014) Drug resistance profiles and clonality of sporadic Shigella sonnei isolates in Ankara Turkey. Braz J Microbiol 45(3):845–849
Kahsay AG, Teklemariam Z (2015) Prevalence of Shigella among diarrheic children under-5 years of age attending at Mekelle health center, north Ethiopia. BMC Res Notes 8(1):1–4
Khatun F, Faruque ASG, Koeck JL, Olliaro P, Millet P, Paris N, Malek MA, Salam MA, Luby S (2011) Changing species distribution and antimicrobial susceptibility pattern of Shigella over a 29-year period (1980–2008). Epidemiol Infect 139(3):446–452
Kotloff KL (2017) The burden and etiology of diarrheal illness in developing countries. Pediatr Clin 64(4):799–814
Leung DT, Das SK, Malek MA, Ahmed D, Khanam F, Qadri F, Faruque AS, Ryan ET (2013) Nontyphoidal Salmonella gastroenteritis at a diarrheal hospital in Dhaka, Bangladesh, 1996–2011. Am J Trop Med Hyg 88(4):661–669
Li YL, Tewari D, Yealy CC, Fardig D, M’ikanatha NM, (2016) Surveillance for travel and domestically acquired multidrug-resistant human Shigella infections—Pennsylvania, 2006–2014. Health Secur 14(3):143–151
Lupindu AM (2018) Epidemiology of Shiga toxin-producing Escherichia coli O157: H7 in Africa in review. S Afr J Infect Dis 33(1):24–30
Magiorakos AP, Srinivasan A, Carey RT, Carmeli Y, Falagas MT, Giske CT, Harbarth S, Hindler JT, Kahlmeter G, Olsson-Liljequist B, Paterson DT, Rice LB, Stelling J, Struelens MJ, Vatopoulos A, Weber JT, Monnet DT (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18(3):268–281
Mahmoudi S, Pourakbari B, Moradzadeh M, Eshaghi H, Ramezani A, Ashtiani MT, Valian SK, Mamishi S (2017) Prevalence and antimicrobial susceptibility of Salmonella and Shigella spp. among children with gastroenteritis in an Iranian referral hospital. Microb Pathog 109:45–48
Majowicz SE, Musto J, Scallan E, Angulo FJ, Kirk M, O’Brien SJ, Jones TF, Fazil A, Hoekstra RM, International Collaboration on Enteric Disease “Burden of Illness” Studies (2010) The global burden of nontyphoidal Salmonella gastroenteritis. Clin Infect Dis 50(6):882–889
Mamuye Y, Metaferia G, Birhanu A, Desta K, Fantaw S (2015) Isolation and antibiotic susceptibility patterns of Shigella and Salmonella among under 5 children with acute diarrhoea: a cross-sectional study at selected public health facilities in Addis Ababa Ethiopia. Clin Microbiol 4(1):186
Mandomando IM, Macete EV, Ruiz J, Sanz S, Abacassamo F, Valles X, Sacarlal J, Navia MM, Vila J, Alonso PL, Gascon J (2007) Etiology of diarrhea in children younger than 5 years of age admitted in a rural hospital of southern Mozambique. Am J Trop Med Hyg 76(3):522–527
Mengistu G, Mulugeta G, Lema T, Aseffa A (2014) Prevalence and antimicrobial susceptibility patterns of Salmonella serovars and Shigella species. J Microb Biochem Technol 6:2–6
Nave HH, Mansouri S, Sadeghi A, Moradi M (2016) Molecular diagnosis and antimicrobial resistance patterns among Shigella spp. isolated from patients with diarrhea. Gastroenterol Hepatol Bed Bench 9(3):205–210.
Nikfar R, Shamsizadeh A, Darbor M, Khaghani S, Moghaddam M (2017) A study of prevalence of Shigella species and antimicrobial resistance patterns in paediatric medical center, Ahvaz Iran. Iran J Microbiol 9(5):277–283
Olorunshola ID, Smith SI, Coker AO (2000) Prevalence of EHEC O157: H7 in patients with diarrhoea in Lagos Nigeria. Apmis 108(11):761–763
Opintan JA, Newman MJ (2007) Distribution of serogroups and serotypes of multiple drug resistant Shigella isolates. Ghana Med J 41(1):8–29
Oppong TB, Yang H, Amponsem-Boateng C, Kyere ED, Abdulai T, Duan G, Opolot G (2020) Enteric pathogens associated with gastroenteritis among children under 5 years in sub-saharan Africa: A systematic review and meta-Analysis. Epidemiol Infect 148.
O’Ryan GM, Ashkenazi-Hoffnung L, O’Ryan-Soriano MA, Ashkenazi S (2014) Management of acute infectious diarrhea for children living in resource-limited settings. Expert Rev Anti Infect Ther 12(5):621–632
Pourakbari B, Mamishi S, Mashoori N, Mahboobi N, Ashtiani MH, Afsharpaiman S, Abedini M (2010) Frequency and antimicrobial susceptibility of Shigella species isolated in Children Medical Center Hospital, Tehran, Iran, 2001–2006. Braz J Infect Dis 14(2):153–157
Rahbar M, Deldari M, Hajia M (2007) Changing prevalence and antibiotic susceptibility patterns of different Shigella species in Tehran, Iran. Internet J Microbiol 3(2).
Rahman MM, Devnath P, Jahan R, Talukder A (2021) Detection of multiple antibiotic-resistant bacteria from the hospital and non-hospital wastewater sources of a small town in Noakhali. Bangladesh J App Biol Biotech 9(3):59–65
Raji MA, Minga UM, Machang’u RS (2008) Prevalence and characterization of verotocytoxin producing Escherichia coli O157 from diarrhoea patients in Morogoro Tanzania. Tanzan J Health Res 10(3):151–158
Reda AA, Seyoum B, Yimam J, Fiseha S, Jean-Michel V (2011) Antibiotic susceptibility patterns of Salmonella and Shigella isolates in Harar Eastern Ethiopia. J Infect Dis Immun 3(8):134–139
Roma B, Worku S, Mariam ST, Langeland N (2000) Antimicrobial susceptibility pattern of Shigella isolates in Awassa. Ethiop J Health Dev 14(2):149–154
Schroeder CM, Zhao C, DebRoy C, Torcolini J, Zhao S, White DG, Wagner DD, McDermott PF, Walker RD, Meng J (2002) Antimicrobial resistance of Escherichia coli O157 isolated from humans, cattle, swine, and food. Appl Environ Microbiol 68(2):576–581
Shrivastava AK, Kumar S, Mohakud NK, Suar M, Sahu PS (2017) Multiple etiologies of infectious diarrhea and concurrent infections in a pediatric outpatient-based screening study in Odisha India. Gut Pathog 9(1):1–12
Singh KKB, Ojha SC, Deris ZZ, Rahman RA (2011) A 9-year study of shigellosis in Northeast Malaysia: antimicrobial susceptibility and shifting species dominance. J Public Health 19(3):231–236
Talukder KA, Islam MA, Khajanchi BK, Dutta DK, Islam Z, Safa A, Alam K, Hossain A, Nair GB, Sack DA (2003) Temporal shifts in the dominance of serotypes of Shigella dysenteriae from 1999 to 2002 in Dhaka Bangladesh. J Clin Microbiol 41(11):5053–5058
Talukder KA, Khajanchi BK, Islam MA, Islam Z, Dutta DK, Rahman M, Watanabe H, Nair GB, Sack DA (2006) Fluoroquinolone resistance linked to both gyrA and parC mutations in the quinolone resistance–determining region of Shigella dysenteriae type 1. Curr Microbiol 52(2):108–111
Tam CC, O’Brien SJ, Tompkins DS, Bolton FJ, Berry L, Dodds J, Choudhury D, Halstead F, Iturriza-Gómara M, Mather K, Rait G (2012) Changes in causes of acute gastroenteritis in the United Kingdom over 15 years: microbiologic findings from 2 prospective, population-based studies of infectious intestinal disease. Clin Infect Dis 54(9):1275–1286
Temu MM, Kaatano GM, Miyaye ND, Buhalata SN, Shushu ML, Kishamawe C, Changalucha JM (2007) Antimicrobial susceptibility of Shigella flexneri and S. dysenteriae isolated from stool specimens of patients with bloody diarrhoea in Mwansa, Tanzania. Tanzan J Health Res 9(3):186–189.
Tian L, Zhu X, Chen Z, Liu W, Li S, Yu W, Zhang W, Xiang X, Sun Z (2016) Characteristics of bacterial pathogens associated with acute diarrhea in children under 5 years of age: a hospital-based cross-sectional study. BMC Infect Dis 16(1):1–8
Ud-Din AI, Wahid SU, Latif HA, Shahnaij M, Akter M, Azmi IJ, Hasan TN, Ahmed D, Hossain MA, Faruque ASG, Faruque SM, Talukder KA (2013) Changing trends in the prevalence of Shigella species: emergence of multidrug resistant Shigella sonnei biotype g in Bangladesh. PloS one 8(12):e82601.
Wang X, Wang J, Sun H, Xia S, Duan R, Liang J, Xiao Y, Qiu H, Shan G, Jing H (2015) Etiology of childhood infectious diarrhea in a developed region of China: compared to childhood diarrhea in a developing region and adult diarrhea in a developed region. Plos one 10(11):e0142136.
Webb A, Starr M (2005) Acute gastroenteritis in children. Aust Fam Physician 34:227–231
WHO (2016) Global Health Observatory (GHO) data 2016: causes of child mortality. http://www.who.int/gho/child_health/mortality/causes/en/.
WHO (2017) Diarrheal disease. http://www.who.int/mediacentre/factsheets/fs330/en/.
WHO (2019) Guidelines for the Control of Shigellosis, Including Epidemics Due to Shigella Dysenteriae Type 1. http://www.who.int/iris/handle/10665/43252.
Wilkerson C, Samadpour M, van Kirk N, Roberts MC (2004) Antibiotic resistance and distribution of tetracycline resistance genes in Escherichia coli O157: H7 isolates from humans and bovines. Antimicrob Agents Chemother 48(3):1066–1067
Williams PC, Berkley JA (2018) Guidelines for the treatment of dysentery (shigellosis): a systematic review of the evidence. Paediatr Int Child Health 38(1):50–65
Zamanlou S, Ahangarzadeh Rezaee M, Aghazadeh M, Ghotaslou R, Babaie F, Khalili Y (2018) Characterization of integrons, extended-spectrum β-lactamases, AmpC cephalosporinase, quinolone resistance, and molecular typing of Shigella spp. from Iran. Infect Dis 50(8):616–624.
Acknowledgements
The authors acknowledged the generous support and assistance provided by Professor Dr. Wahhida Shumi, former Chairman, Department of Microbiology, University of Chittagong; Dr. Md. Nurul Haque, Director (Administration), Chattogram Maa-O-Shishu Hospital Medical College; Jabed Khan Shaikat, Abdullah Al Mukarrom, and Shihab Hoque from the Department of Microbiology, University of Chittagong.
Funding
None.
Author information
Authors and Affiliations
Contributions
MSU and MMR have contributed in designing of the study. MSU, KMSI, and SD have collected samples and performed lab experiments. MSU, MMR, MOF, and AT have done data analysis and prepared the draft manuscript. MIH and MMR have contributed to the editing and critical revision of the manuscript. Finally, all authors have read and approved the manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We have taken written permission from the ethical committee of the Department of Microbiology at the University of Chittagong to conduct the study, and written consent has been taken from the patient's attended guardian with informing aims and objectives, merits, and demerits of participation in the study. The permission from the ethical committee came with a letter without mentioning any reference number.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Uddin, M.S., Rahman, M.M., Faruk, M.O. et al. Bacterial gastroenteritis in children below five years of age: a cross-sectional study focused on etiology and drug resistance of Escherichia coli O157, Salmonella spp., and Shigella spp.. Bull Natl Res Cent 45, 138 (2021). https://doi.org/10.1186/s42269-021-00597-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-021-00597-9