Abstract
Background
Due to the growing use of cannabis for the purposes of pain relief, evidence is needed on the impact of cannabis use on concurrent analgesic use. Therefore, our objective was to evaluate the association between the use of cannabis and codeine.
Methods
We conducted a cross-sectional study using data from the nationally representative Canadian Tobacco, Alcohol and Drugs Survey (2017). The primary explanatory variable was self-reported use of cannabis within the past year. The outcome was the use of codeine-containing product(s) within the past year. We used multivariable binomial logistic regression models.
Results
Our study sample comprised 15,459 respondents including 3338 individuals who reported cannabis use within the past year of whom 955 (36.2%) used it for medical purposes. Among individuals who reported cannabis use, the majority were male (N = 1833, 62.2%). Self-reported use of cannabis was associated with codeine use (adjusted odds ratio [aOR] 1.89, 95% CI 1.36 to 2.62). Additionally, when limited to cannabis users only, we found people who used cannabis for medical purposes to be three times more likely to also report codeine use (adjusted odds ratio [aOR] 2.96, 95% CI 1.72 to 5.09).
Discussion
The use of cannabis was associated with increased odds of codeine use, especially among individuals who used it for medical purposes. Our findings suggest a potential role for healthcare providers to be aware of or monitor patients’ use of cannabis, as the long-term adverse events associated with concurrent cannabis and opioid use remain unknown.
Similar content being viewed by others
Introduction
Approximately one out of four Canadians aged 15 years and older live with non-cancer chronic pain, a condition for which people may use opioid therapy for adequate pain relief (Reid et al. 2002). However, chronic use of opioids warrants caution due to the increased risk of severe adverse events such as constipation, hyperalgesia, and the potential for developing an opioid addiction, which may result in the occurrence of an overdose (Deshpande et al. 2015; Campbell et al. 2018; Lee et al. 2011). Recent research has shown that concomitant use of cannabis and opioids may be beneficial for chronic non-cancer pain patients, as cannabis may enhance the analgesic effects of opioids, thereby decreasing daily opioid intake and risk of opioid-related harms (Degenhardt et al. 2015; Haroutounian et al. 2016). As a result, cannabis is currently being investigated for the treatment of chronic pain and opioid dependence. While the use of cannabis may offer potential harm reduction to stem the impacts of the current epidemic of opioid-related deaths, little research has been done to assess the long-term patient outcomes associated with concurrent opioid and cannabis use (Rogers et al. 2019; Khan et al. 2020). Specifically, as both substances are central nervous system depressants, concomitant use may put people at increased risk of falls, motor vehicle accidents, and respiratory depression (Rogers et al. 2019; Windle et al. 2021).
Codeine is the most frequently prescribed opioid in the world and is easily accessible to Canadians over the counter (OTC) as a low dose (≤ 15 mg/dosage unit) preparation made in combination with simple analgesics (acetaminophen or nonsteroidal anti-inflammatory drugs [NSAIDs]) upon pharmacist consultation (Nielsen et al. 2018; Non-prescription analgesic and antitussive medications containing codeine: a review of clinical effectiveness and safety 2018; Canadian Institute for Health Information 2019). However, appropriate pharmacy screening for codeine dependence prior to dispensing of low-dose codeine rarely occurs (MacKinnon 2016; Foley et al. 2016). While codeine is primarily indicated for use as a cough suppressant or analgesic, guidelines generally suggest that codeine has a limited role in the management of chronic pain conditions, prior to initiating stronger opioids in acute pain conditions (Gisev et al. 2016). While codeine may be characterized as a “weak opioid,” the risk of dependence and harm secondary to tolerance and subsequent dose escalations must be cautioned (Canadian Institute for Health Information 2019). In fact, the Canadian province of Ontario reported codeine to be detected in 6.3% of all accidental opioid-related deaths that occurred between July 2017 and June 2018 (Chief OAfHPaPPHOOot, Coroner; Ontario Forensic Pathology Service; Ontario Drug Policy Research Network n.d.). Additionally, overuse of codeine-containing products may also lead to serious harms secondary to the supratherapeutic intake of the simple analgesic component. For example, hepatotoxicity may occur due to acetaminophen overdose, and gastric and/or renal complication may arise due to chronic NSAID exposure (Frei et al. 2010).
Due to the legalization of cannabis across Canada (in 2017) and widespread availability of both prescription and OTC codeine, people may be concurrently using cannabis- and codeine-containing products, placing them at increased risk of adverse events (Rogers et al. 2019; Canadian Institute for Health Information 2019; Government of Canada 2021; Corroon et al. 2019). Moreover, healthcare providers may be unaware of their patient’s concomitant cannabis and prescription and/or OTC codeine use as a majority of individuals choose not to disclose their use of cannabis to their healthcare provider due to self-perceived stigma (Leos-Toro et al. 2018). Therefore, the objective of our study was to evaluate the association between the use of cannabis- and codeine-containing products.
Methods
Study design and source population
We conducted a population-based cross-sectional study using the public use microdata file from the nationally administered Canadian Tobacco, Alcohol and Drugs Survey (CTADS) as the source population (Statistics Canada 2021). In brief, the CTADS was conducted in 2017 by computer-assisted telephone technology and aimed to assess the prevalence of cigarette smoking, alcohol use, and drug use and the extent of harm related to usage. Survey sampling was allocated based on age, sex, and geographical distribution to ensure representation at both provincial and national levels. Individual participants were 15 years and older and resided in one of the 10 Canadian provinces. Exclusion criteria included residents of the Yukon, Northwest Territories, Nunavut, and individuals living in long-term care institutions or Canadian Forces bases. Additional details on the design and methodology of the CTADS are available through the Statistics Canada (Statistics Canada 2021). Data from the CTADS were kept private and confidential as per the Statistics Act. Where possible, this investigation adhered to STROBE reporting guidelines for observational studies.
Study variables
The main explanatory variables were as follows: (1) self-reported use of cannabis within the past year (“During the past 12 months have you used marijuana?”) and (2) self-reported use of cannabis for medical purposes within the past year (“In the past 12 months, have you used or tried marijuana (hashish, hash oil or other cannabis derivatives) for medical purposes?”). Both were binary categorical in nature with response options of “yes” or “no.” We also considered additional variables describing cannabis use including the following: (1) method of cannabis consumption (“eaten,” “vaporized,” “drank,” or “smoked”), (2) frequency of cannabis use within the past 3 months (“once or twice,” “monthly,” “weekly,” or “daily or almost daily”), (3) illicit drug use excluding cannabis in the past 12 months (“yes” or “no”), and (4) self-perceived impairment due to cannabis use (“yes” or “no”).
The main outcome variable was self-reported use of any codeine-containing products within the past year. This was assessed by the question “During the past 12 months, have you used any codeine products like Tylenol #3, Tylenol #1, 292’s or 222’s?” with response options of “yes” or “no.”
We considered the following variables as potential confounders to the relationship between cannabis and codeine use: age, sex, geographic region of residence (rural or urban), education (university degree and above, trade/college, secondary, or less than secondary), absence from work (present or absent), current smoking status (smoker or nonsmoker), and self-perceived general health (excellent/very good, good, fair/poor). We selected the aforementioned covariates based on data availability in the CTADS, function as social determinants of health (Canada Go 2020) or due to an established association with cannabis and/or codeine use (Hindocha et al. 2015). Participants with invalid responses (i.e., “don’t know,” “not stated,” or “refusal”) to explanatory, outcome, and confounding variables were excluded.
Statistical analysis
Descriptive statistics were used to summarize participants’ characteristics. We estimated the weighted prevalence of cannabis use among the Canadian population based on our study sample and described characteristics of cannabis use. In our primary analysis, we used multivariable binomial logistic regression to evaluate the association between self-reported use of cannabis and codeine, adjusted for confounding variables. In the secondary analysis, we limited analysis to cannabis users to evaluate the association between self-reported use of cannabis for medical purposes and codeine. For the secondary analysis, we also used multivariable binomial logistic regression, adjusted for confounding variables. The statistical analyses were weighted using CTADS master weights to provide population-level estimates (i.e., proportion (%), odds ratio (Force 2020)). All of the analyses were completed using SAS University Edition (SAS Institute Inc., Cary, NC).
Ethics approval
Ethical approval to use the publicly available CTADS data was covered by the University of British Columbia’s Policy (no. LR9) on research involving human participants.
Results
The CTADS source population consisted of 16,349 participants in total; after excluding 890 participants with invalid responses to study variables, the final study sample included 15,459 individuals. Demographic characteristics for the study sample are reported in Table 1. Overall, 3338 (21.6%) individuals reported use of cannabis within the past year, and 12,121 (78.4%) did not. Among individuals who reported cannabis use, approximately two-thirds were male (N = 1833, 62.2%) and between the ages of 15 to 44 years old (N = 2967, 74.3%). Illicit drug use was greater among individuals self-reporting use of cannabis (22.3%) in comparison with those who did not (0.8%). Lastly, codeine use was higher among individuals who reported use of cannabis (14.0%) in comparison with those who did not report use of cannabis (8.0%).
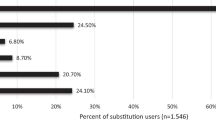
Patterns of cannabis used among individuals who did and did not self-report use of codeine-containing product(s) are stated in Table 2. The vast majority of individuals who did (98.3%) and did not (97.4%) self-report use of codeine also reported using cannabis more than once. However, the self-reported prevalence of cannabis on a weekly or more frequent basis was greater among individuals who reported use of codeine (55.4%), in comparison with those who did not report use of codeine (36.0%). Additionally, among individuals who reported use of codeine, a higher proportion also reported use of cannabis for medical purposes (61.6%), in comparison with those who did not report use of codeine (32.1%).
The unadjusted odds ratio (OR) for the association between self-reported use of cannabis and codeine was 1.86 (95% CI, 1.37 to 2.54). After including age, sex, geographic region of residence, education, absence from work, smoking status, marital status, and self-perceived health in the multivariable logistic regression model, we observed a small increase in the OR representing the association between cannabis and codeine use (adjusted odds ratio [aOR] 1.90, 95% CI 1.38 to 2.62) (Table 3). In this multivariable model, we also found an inverse association between being in very good/excellent health with use of codeine (aOR 0.53, 95% CI 0.36 to 0.80) as compared to being in fair/poor health.
For our secondary analyses limited to individuals who used cannabis, the unadjusted OR for the association between self-reported use of cannabis for medical purposes and codeine-containing product(s) was 3.42 (95% CI, 2.04 to 5.76). In the multivariable model, after adjusted for age, sex, geographic region of residence, education, absence from work, smoking status, marital status, and self-perceived health, we observed an attenuation of the OR but nonetheless represented a nearly 3-fold increase in the odds of codeine use among individuals who used cannabis for medical purposes (aOR 2.96, 95% CI 1.71 to 5.10) (Table 4). Additionally, within this subgroup of cannabis users, males had lower odds of reporting codeine use in comparison with females (aOR 0.57, 95% CI 0.34 to 0.97).
Discussion
We used data from an established nationally representative Canadian survey to evaluate the relationship between cannabis and codeine use. Overall, 21.6% of Canadians self-reported use of cannabis in 2017, of whom 36.2% used cannabis for medical purposes. Multivariable logistic regression models indicate that individuals who self-reported use of cannabis had greater odds of also reporting use of codeine. When limited to cannabis users, individuals who used cannabis for medical purposes were nearly three times more likely to also report codeine use. These findings reflect the increasing need to further investigate the safety profile of concomitant cannabis and opioid use along with the need for healthcare providers, particularly prescribers (i.e., physicians, nurse practitioners) and pharmacists to assess a patient’s use of cannabis prior to prescribing or dispensing codeine. Furthermore, these findings suggest a potential role for healthcare providers for monitoring patients’ use of cannabis, as the long-term adverse events associated with concurrent use with prescription medications, particularly codeine, remain unknown.
Evidence to support the use of cannabis for treatment of non-cancer chronic pain and opioid dependence has recently emerged, as studies highlight a declining trend in opioid consumption following subsequent cannabis use (Lucas et al. 2021; Dranitsaris et al. 2021). Specifically, a Canadian prospective study (N = 1145) conducted by Lucus et al. reported an overall 78% reduction in mean opioid dosage over the course of 6 months with cannabis use (Lucas et al. 2021). However, it should be noted that study participants received physician guidance regarding appropriate cannabis use throughout the entirety of the study, an aspect which is not observed in the general population (Leos-Toro et al. 2018; Lucas et al. 2021). Additionally, due to the short-term durations (e.g., 6 months) of studies assessing the impact of cannabis on opioid consumption, many fail to assess the potential for long-term adverse effects. Furthermore, with concomitant use, it is important to consider harms associated with polypharmacy, which has always been shown to be more significant than single drug use (Lake et al. 2020; Giummarra et al. 2015).
Our study adds to the existing body of literature by highlighting the strong positive association between the use of cannabis and codeine, two substances which are widely accessible to patients without prescription and/or healthcare professional supervision, particularly in recent years in Canada (Novak et al. 2016). To contextualize with studies in other jurisdictions, in 2018, Caputi et al. used nationally representative individual-level data and reported positive association (aOR 1.66 95% CI 1.49 to 1.83) between use of cannabis and pain relieving medications (Caputi and Humphreys 2018), similar to our current study. Additionally, our study results reflect a strong association (3-fold odds) between the use of cannabis for medical purposes and codeine use. While our study was unable to specify which medical condition study participants were using medical cannabis for, this substantial increase in odds of codeine use among individuals who used cannabis for medical purposes may be attributed to experiencing greater pain severity as a majority of people who use cannabis for medical purposes do so for pain relief (Lake et al. 2019; Boehnke et al. 2022; Leung et al. 2022).
In addition to findings on the association between cannabis and opioid use, our findings also highlight that people who report very good/excellent perceived general health were less likely to report codeine use, compared to those who perceive their health as fair/poor. These findings are in line with previous literature demonstrating poorer physical and mental health scores among individuals who report opioid use (Millson et al. 2004). Another unique finding of our study was that among cannabis users, males were less likely to use codeine in comparison with females. These findings are in line with previous literature that highlights differences in opioid prescription rates among males and females. In comparison to males, females are more likely to be prescribed opioids (Serdarevic et al. 2017), which may be explained in part due to the increased prevalence of chronic conditions resulting in pain among females, such as inflammatory arthritis, fibromyalgia, and migraines (Darnall et al. 2012).
Limitations must be considered when interpreting the results of this study. First, the CTADS survey was conducted between February and December of 2017; therefore, the survey was conducted prior to legalization of cannabis across Canada (October 17, 2018) which may put study results at risk of respondent or social desirability bias. However, it should be noted that access to cannabis for medical purpose has been legalized in Canada since 2000. While we do acknowledge the rising prevalence of cannabis use since legalization in 2018 (Rotermann 2021), the intent of our work was not to establish cannabis use patterns but rather to explore the potential for concurrent cannabis and codeine use. Future research is required to further explore the relationship and impacts of concurrent cannabis and opioid use. Second, our study is restricted to the variables included in the CTADS survey, which does not include information on how frequently participants consumed codeine-containing product(s), limiting our results from truly assessing concurrent use. Third, the cross-sectional study design precludes the ability to infer temporality between exposure and outcome variables. Fourth, exclusion of survey participants with invalid responses to explanatory, outcome, and confounding variables may have impacted the external validity of our study, as a greater proportion of participants included in our study received education past secondary school in comparison with those excluded, which may bias the result of our analysis. Fourth, we excluded survey participants (n = 890) with invalid responses to explanatory, outcome, and confounding variables. Comparison with our study sample on sociodemographic characteristics (i.e., sex, age, geographic region, and education) revealed no differences except with respect to education, whereby a lower proportion of excluded participants reported completing secondary school education or did not provide a response to the question. Lastly, due to sample size limitations, certain descriptive variables did not meet Statistics Canada’s definition for acceptable “quality,” as the coefficient of variation was above their stated threshold (Statistics Canada 2021). Therefore, we were unable to include covariates that have been shown to be associated with codeine use such as use of psychoactive substances, cannabis use characteristics (i.e., method, frequency, self-perceived impairment, and reason for medical cannabis use), and alcohol consumption to maintain the quality of our analysis.
Conclusion
Altogether, this current study suggests that individuals who have used cannabis in the past year are at 72% greater odds of reporting the use of codeine-containing product(s). When limited to individuals who used cannabis in the past year, those who used cannabis for medical purpose were at an even greater odds of codeine use and were three times more likely to use codeine-containing product(s) in comparison with those who used cannabis for nonmedical purposes. The strong association between codeine and cannabis indicates the need for health professionals to monitor patients for concomitant use of cannabis and codeine as long-term adverse events associated with concomitant use remain largely unknown. Patients using cannabis for medical purposes may benefit from interdisciplinary care and should receive patient counseling on the potential for increased central nervous system depression if cannabis and opioids are used concurrently (Rogers et al. 2019).
Availability of data and materials
The public use microdata file can be accessed through the Statistics Canada (https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=4440).
Abbreviations
- OTC:
-
Over the counter
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- CTADS:
-
Canadian Tobacco, Alcohol and Drugs Survey
- OR:
-
Odds ratio
- aOR:
-
Adjusted odds ratio
References
Boehnke KF, Dean O, Haffajee RL, Hosanagar A. U.S. trends in registration for medical cannabis and reasons for use from 2016 to 2020 : an observational study. Ann Intern Med. 2022;175(7):945–51.
Campbell G, Hall WD, Peacock A, et al. Effect of cannabis use in people with chronic non-cancer pain prescribed opioids: findings from a 4-year prospective cohort study. Lancet Public Health. 2018;3(7):e341–e50.
Canada Go. Social determinants of health and health inequalities 2020 Available from: https://www.canada.ca/en/public-health/services/health-promotion/population-health/what-determines-health.html cited 26 Sept 2021.
Canadian Institute for Health Information. Opioid prescribing in canada: how are practices changing? Ottawa: CIHI; 2019.
Caputi TL, Humphreys K. Medical marijuana users are more likely to use prescription drugs medically and nonmedically. J Addict Med. 2018;12(4):295–9.
Corroon J, Sexton M, Bradley R. Indications and administration practices amongst medical cannabis healthcare providers: a cross-sectional survey. BMC Fam Pract. 2019;20(1):174.
Darnall BD, Stacey BR, Chou R. Medical and psychological risks and consequences of long-term opioid therapy in women. Pain Med. 2012;13(9):1181–211.
Degenhardt L, Lintzeris N, Campbell G, et al. Experience of adjunctive cannabis use for chronic non-cancer pain: findings from the pain and opioids in treatment (point) study. Drug Alcohol Depend. 2015;147:144–50.
Deshpande A, Mailis-Gagnon A, Zoheiry N, Lakha SF. Efficacy and adverse effects of medical marijuana for chronic noncancer pain: systematic review of randomized controlled trials. Can Fam Physician. 2015;61(8):e372–81.
Dranitsaris G, DeAngelis C, Pearson B, McDermott L, Pohlmann-Eden B. Opioid prescribing in Canada following the legalization of cannabis: a clinical and economic time-series analysis. Appl Health Econ Health Policy. 2021;19:537–44.
Foley M, Carney T, Rich E, Parry C, Van Hout MC, Deluca P. Medical professionals' perspectives on prescribed and over-the-counter medicines containing codeine: a cross-sectional study. BMJ Open. 2016;6(7):e011725.
Force CPT. Working together to better understand, prevent, and manage chronic pain: what we heard. Health Canada. 2020.
Frei MY, Nielsen S, Dobbin MD, Tobin CL. Serious morbidity associated with misuse of over-the-counter codeine-ibuprofen analgesics: a series of 27 cases. Med J Aust. 2010;193(5):294–6.
Gisev N, Nielsen S, Cama E, Larance B, Bruno R, Degenhardt L. An ecological study of the extent and factors associated with the use of prescription and over-the-counter codeine in Australia. Eur J Clin Pharmacol. 2016;72(4):469–94.
Giummarra MJ, Gibson SJ, Allen AR, Pichler AS, Arnold CA. Polypharmacy and chronic pain: harm exposure is not all about the opioids. Pain Med. 2015;16(3):472–9.
Government of Canada. Cannabis legalization and regulation. 2021. Available from: https://www.justice.gc.ca/eng/cj-jp/cannabis/ [updated 2021; cited 31 May 2021].
Haroutounian S, Ratz Y, Ginosar Y, et al. The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain: a prospective open-label study. Clin J Pain. 2016;32(12):1036–43.
Hindocha C, Shaban ND, Freeman TP, et al. Associations between cigarette smoking and cannabis dependence: a longitudinal study of young cannabis users in the United Kingdom. Drug Alcohol Depend. 2015;148:165–71.
Khan R, Naveed S, Mian N, Fida A, Raafey MA, Aedma KK. The therapeutic role of cannabidiol in mental health: a systematic review. J Cannabis Res. 2020;2(1):2.
Lake S, Socias ME, Milloy MJ. Evidence shows that cannabis has fewer relative harms than opioids. CMAJ. 2020;192(7):E166–E7.
Lake S, Walsh Z, Kerr T, et al. Frequency of cannabis and illicit opioid use among people who use drugs and report chronic pain: a longitudinal analysis. PLoS Med. 2019;16(11):e1002967.
Lee M, Silverman SM, Hansen H, Patel VB, Manchikanti L. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. 2011;14(2):145–61.
Leos-Toro C, Shiplo S, Hammond D. Perceived support for medical cannabis use among approved medical cannabis users in Canada. Drug Alcohol Rev. 2018;37(5):627–36.
Leung J, Chan G, Stjepanovic D, Chung JYC, Hall W, Hammond D. Prevalence and self-reported reasons of cannabis use for medical purposes in USA and Canada. Psychopharmacology. 2022;239(5):1509–19.
Lucas P, Boyd S, Milloy MJ, Walsh Z. Cannabis significantly reduces the use of prescription opioids and improves quality of life in authorized patients: results of a large prospective study. Pain Med. 2021;22(3):727–39.
MacKinnon JI. Tighter regulations needed for over-the-counter codeine in Canada. Can Pharm J (Ott). 2016;149(6):322–4.
Millson PE, Challacombe L, Villeneuve PJ, et al. Self-perceived health among Canadian opiate users: a comparison to the general population and to other chronic disease populations. Can J Public Health. 2004;95(2):99–103.
Nielsen S, MacDonald T, Johnson JL. Identifying and treating codeine dependence: a systematic review. Med J Aust. 2018;208(10):451–61.
Novak SP, Peiper NC, Zarkin GA. Nonmedical prescription pain reliever and alcohol consumption among cannabis users. Drug Alcohol Depend. 2016;159:101–8.
Ontario Agency for Health Protection and Promotion (Public Health Ontario); Office of the Chief Coroner; Ontario Forensic Pathology Service; Ontario Drug Policy Research Network. Opioid mortality surveillance report: analysis of opioid-related deaths in Ontario July 2017-June 2018. Toronto, ON: Queen’s Printer for Ontario; 2019.
Reid MC, Engles-Horton LL, Weber MB, Kerns RD, Rogers EL, O'Connor PG. Use of opioid medications for chronic noncancer pain syndromes in primary care. J Gen Intern Med. 2002;17(3):173–9.
Rogers AH, Bakhshaie J, Buckner JD, et al. Opioid and cannabis co-use among adults with chronic pain: relations to substance misuse, mental health, and pain experience. J Addict Med. 2019;13(4):287–94.
Rotermann M. Looking back from 2020, how cannabis use and related behaviours changed in canada. Health Rep. 2021;32(4):3–14.
Serdarevic M, Striley CW, Cottler LB. Sex differences in prescription opioid use. Curr Opin Psychiatry. 2017;30(4):238–46.
Statistics Canada. Canadian Tobacco AaDSCcS, 2021 Available from: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=4440.
Windle SB, Eisenberg MJ, Reynier P, et al. Association between legalization of recreational cannabis and fatal motor vehicle collisions in the united states: an ecologic study. CMAJ Open. 2021;9(1):E233–E41.
Young C, Loshak H. Non-prescription analgesic and antitussive medications containing codeine: a review of clinical effectiveness and safety. Ottawa: CADTH; 2018. (CADTH Rapid response report: summary with critical appraisal).
Acknowledgements
None declared
Funding
Dr. De Vera holds a Tier 2 Canada Research Chair in Medication Adherence, Utilization, and Outcomes.
Author information
Authors and Affiliations
Contributions
RG and MDV contributed to the study design as well as the acquisition, analysis, and interpretation of data. RG drafted the manuscript, and all study authors (RG, KS, MDV) revised and approved the final version for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval to use the publicly available CTADS data was covered by the University of British Columbia’s Policy (no. LR9) on research involving human participants.
Consent for publication
Not required
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Garg, R., Shojania, K. & De Vera, M.A. The association between cannabis and codeine use: a nationally representative cross-sectional study in Canada. J Cannabis Res 4, 49 (2022). https://doi.org/10.1186/s42238-022-00160-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42238-022-00160-x