Abstract
Background
Transpedal access is increasingly utilized for the treatment of peripheral artery disease (PAD). Femoral-popliteal artery chronic total occlusions (CTOs) are some of the most difficult lesion subsets that sometimes require the use of re-entry support devices during percutaneous intervention. Limited data is available on the use of re-entry devices when treating femoral-popliteal CTOs via transpedal access. The aim of this study was to demonstrate the feasibility of using the Outback® Elite re-entry device for the treatment of femoral-popliteal CTOs via the transpedal approach in an outpatient based lab setting.
Methods
Seventeen patients presented with femoral-popliteal CTOs in which treatment required the use of the Outback® Elite re-entry device. All procedures were performed in a single outpatient based lab. Patients were followed at 1 week and 1 month post-procedure, with lower extremity arterial duplex ultrasound assessment during the 1 month follow-up.
Results
The average patient age was 78 years-old, with 71% being males. Most patients presented with Rutherford class IV symptoms. Procedural success was achieved in all patients with no requirement to convert to femoral artery access in any of the cases. No immediate post-procedural complications nor at any time during follow-up were observed. Ultrasonography at 1 month follow-up showed patent intervention sites and access site vessels in all patients.
Conclusion
The use of the Outback® Elite re-entry device for the treatment of femoral-popliteal CTOs via transpedal access is a feasible option and may have potential benefits by avoiding risks associated with traditional femoral artery access.
Similar content being viewed by others
Background
Peripheral arterial disease (PAD) is a common and debilitating condition that affects an estimated 202 million people worldwide (Gerald et al. 2013). More importantly, there has been a greater than 20% increase in the incidence of PAD since 2001(Pande et al. 2011; Gerald et al. 2013). Due to the rapid development of new technologies and techniques, an endovascular approach is a now a first-line option after conservative therapy for the treatment of symptomatic PAD. Between 2001 and 2007, PAD treatment has seen a 78% increase in endovascular procedures and 20% decrease in open bypass procedures with an overall reduction in the need for amputation during that same time period (Hong et al. 2011).
The traditional access site for the endovascular treatment of PAD is the contralateral common femoral artery (CFA) and subsequent cross-over, or ipsilateral antegrade CFA access. However, femoral access site complication rates have been reported to be as high as 2.3% and comprise a significant proportion of overall procedural related complications (Jolly et al. 2009; Sajnani and Bogart 2013). In order to decrease these complication rates, alternative access sites, including pedal and radial artery (RA) access, have become more frequently utilized. Alternative access sites have the benefit of being safer as well as providing increased patient comfort/satisfaction and shorter recovery time/time to ambulation (Kiemeneij et al. 1997; Vora and Rao 2014; Kwan et al. 2015).
A frequent concern that many peripheral operators have with the transpedal approach is the perceived lack of availability of certain devices for use in challenging cases. Chronic total occlusions (CTOs) in the superficial femoral artery (SFA) or popliteal artery remain one of the hardest lesion subsets to treat and sometimes require re-entry from a dissection plane back into the vessel true lumen. In this case series, we show the feasibility of using the Outback® Elite re-entry device for the treatment of femoral-popliteal CTOs via transpedal access.
Methods
Patients
Seventeen patients who failed conservative management for lifestyle limiting claudication or critical limb ischemia (Rutherford class III or higher) were identified and underwent diagnostic angiograms which demonstrated femoral-popliteal CTOs. Following discussion of possible treatment options, including vascular bypass, a collective decision was made to proceed with percutaneous endovascular intervention for each patient. All procedures were performed via transpedal access in a single outpatient based lab setting. The transpedal approach was selected due to known prior difficulty and failed standard CTO revascularization attempts in each of the patients.
Vascular access and lesion identification
All patients were brought to the catheterization laboratory and prepared in standard fashion for a diagnostic unilateral peripheral angiogram. An ultrasound was performed to determine which vessel – anterior tibial artery (ATA), posterior tibial artery (PTA), or peroneal artery would be the appropriate access site. The pedal area on the ipsilateral side of the affected leg was then prepared in sterile fashion and a 21-gauge micropuncture needle was used for arterial access under ultrasound guidance followed by placement of a 4-Fr Glidesheath (Terumo). After confirming arterial flow, 5000 units of heparin were given intravenously and an antispasmodic cocktail of nitroglycerin 100 μg and verapamil 2.5 mg was administered into the sheath. To achieve an activated clotting time (ACT) > 300 s, additional heparin was given if needed. A routine diagnostic angiogram was performed and a femoral-popliteal CTO was encountered in each case. Secondary arterial access was obtained via the RA for antegrade injections. All patients received conscious sedation (fentanyl and/or midazolam) as well as local anesthesia.
Endovascular intervention and follow-up
The Outback® Elite re-entry device (Cordis) was used after initial wire escalation attempts failed to re-enter into the true lumen of the stenotic lesion. For each procedure, radial access was obtained using a 4-Fr sheath, which was eventually upsized to a 6-Fr Slender Glidesheath (Terumo) to allow use of the Outback re-entry device. Final treatment of the CTO with angioplasty and/or stenting was performed at the discretion of the operator. Procedural success was defined as successful re-entry into the true vessel lumen with < 20% residual stenosis at the target lesion by the end of the procedure. Based on our prior success and low complication rates using the TR band (Terumo) and VasoStat (Forge Medical, Inc.) devices to achieve hemostasis at different transpedal puncture sites, we implemented the same previously described technique in all the cases (Patel et al. 2016). Each patient was discharged home 2 h post-procedure on atorvastatin 80 mg daily and dual antiplatelet therapy with daily aspirin 81 mg and clopidogrel 75 mg for at least 1 month. All patients had clinical follow-up at 1 week and 1 month post-procedure, with lower extremity arterial duplex ultrasound assessment at the 1 month follow-up. Below are 3 selected cases to illustrate how the Outback® Elite re-entry device was utilized in each endovascular intervention.
Case #1
A 74 year-old male who presented with Rutherford class IV ischemic rest pain was brought to the catheterization laboratory and a right peroneal artery access was obtained. A tibioperoneal (TP) trunk into the proximal peroneal artery CTO with zero vessel runoff was identified (ATA and PTA were also occluded – Fig. 1a). To visualize the full length of the CTO and facilitate re-entry, radial access was obtained with a 4-Fr sheath, followed by advancement of a 4-Fr Multicurve 150 cm catheter (Terumo) into the CFA (Fig. 1b). The 4-Fr pedal sheath was upsized to a 6-Fr Slender Glidesheath (Terumo) to allow use of the Outback re-entry device. Using test injections from the antegrade catheter via radial access, the Outback re-entry device was positioned and advanced over a hydrophobic 0.014-in. Grand Slam wire (ASAHI) with successful penetration into the true lumen of the popliteal artery (Fig. 1c). Angioplasty of the distal popliteal into the TP trunk/peroneal artery was performed (Fig. 1d). Post-angioplasty angiogram showed excellent flow with no dissection – therefore stenting was not necessary (Fig. 1e). Final angiogram of the distal peroneal artery did not reveal any vessel injury (Fig. 1f).
Case #1 (a) Retrograde angiography via the right peroneal artery (thick white arrow) demonstrating the tibioperoneal (TP) trunk into the proximal peroneal artery CTO (thin white arrows) with an extensive network of collaterals and vague reconstitution of the native popliteal artery through retrograde filling (black arrow). b Antegrade angiogram re-demonstrating the CTO with zero vessel runoff and an occluded proximal ATA (black arrow). Note again the retrograde catheter in the peroneal artery (white arrow). c The Outback re-entry device entering the true lumen of the distal popliteal artery (white arrow). d Balloon angioplasty via pedal artery access. e Post-intervention angiogram showing successful recanalization through the TP trunk and peroneal artery. f Post-intervention angiogram of the peroneal artery access site illustrating excellent flow without vessel injury
Case #2
A 79 year-old male was sent for evaluation for worsening claudication that had progressed to Rutherford class IV ischemic rest pain in his left lower extremity. Left ATA access was obtained and angiography revealed a distal CTO of the ATA (Fig. 2a). Left radial access was obtained and a catheter was advanced into the CFA. Antegrade angiogram revealed a popliteal artery CTO. Collateral filling of the PTA and peroneal artery were noted. With wire escalation techniques, a dissection plane was created from the ATA adjacent to the true lumen of the popliteal artery (Fig. 2b). Small balloon inflation using a 3.0 mm × 250 mm Saber balloon (Cordis) of the ATA was performed as part of preparing the vessel lumen for the Outback re-entry device. Using test injections from the antegrade catheter via radial access, the Outback re-entry device was positioned and advanced over a hydrophobic 0.014-in. Grand Slam wire (ASAHI) with successful re-entry into the true lumen of the target vessel (Fig. 2c). Angioplasty and stenting were performed (Fig. 2d) with good post-intervention results (Fig. 2e). Direct 3-vessel outflow was seen at the end of the procedure (Fig. 2f).
Case # 2 (a) Angiogram through the pedal access sheath in the ATA (white arrow) shows a distal CTO of the ATA (black arrow). b Antegrade angiogram showing a popliteal CTO. Note the dissection plane created by wire escalation techniques adjacent to the true lumen of the popliteal artery (thick white arrow). The ATA is completely occluded from proximal to distal (black arrow). Collaterals fill the TP trunk into the PTA and peroneal artery (thin white arrows). c The Outback re-entry device entering the true lumen of the distal popliteal artery (white arrow). d Balloon angioplasty followed by stenting of the popliteal artery. e Post-intervention angiogram showing restoration of flow post-stenting. f Final angiogram of the infrapopliteal vessels demonstrating direct line flow to all pedal arteries, including the ATA access site (white arrow)
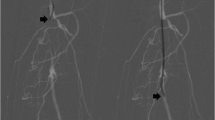
Case #3
A 74 year-old female presented with Rutherford Grade V symptoms - ischemic rest pain and dry gangrene on the plantar surfaces of her right 1st, 3rd, and 5th toes with duplex ultrasonography showing a long CTO of the entire right SFA and extending into the popliteal artery. Right peroneal artery access was obtained and retrograde angiogram demonstrated the distal cap of the CTO at the popliteal artery as well as total occlusion of the ATA and PTA (Fig. 3a). Left radial access was obtained and a catheter was advanced into the CFA. Antegrade injections localized the proximal cap of the CTO to the ostial SFA (Fig. 3b). The Outback re-entry device was advanced over a 0.014-in. Grand Slam wire (ASAHI) and positioned using antegrade injections with successful entry into the true lumen (Fig. 3c). Angioplasty of the entire SFA and popliteal was performed using 6.0 mm × 250 mm Saber balloons (Cordis; Fig. 3d). Post-intervention angiography of the SFA demonstrated patency of the previously occluded vessel (Fig. 3e) and patency of the peroneal artery access site (Fig. 3f).
Case #3 (a) Retrograde angiography via peroneal access demonstrating the distal cap of the CTO at the popliteal artery (white arrow). b Antegrade angiography depicting the proximal cap of the CTO at the ostial SFA (white arrow). c The Outback re-entry device traversing the SFA (thick white arrow) with the tip positioned in the CFA for re-entry into the true lumen (thin white arrow). d Balloon angioplasty of the occluded SFA. e Post-intervention angiogram showing a patent vessel with no significant stenosis. f Final angiography of the peroneal access site exhibiting vessel patency and no evidence of vessel injury
Results
The patient and lesion characteristics are listed in Tables 1 and 2. The average patient age was 78 years-old with 71% male. All patients had multiple co-morbidities predisposing to PAD. Most patients presented with Rutherford class IV symptoms. Post-angioplasty stenting was performed in 1/17 patients. Procedural success was achieved in all patients without the need to convert to femoral artery access in any of the cases. The average duration of the procedures was 56 min. No complications immediately post procedure nor at any time period during follow up were noted. All patients reported clinical improvement in symptoms. Duplex ultrasound at 1 month follow-up showed patent intervention sites as well as patent pedal access sites.
Discussion
Several approaches are being utilized for the endovascular treatment of femoral-popliteal CTOs. An antegrade intraluminal approach had been the traditional method of revascularization, however, this technique may fail in up to 25% of cases, particularly with long, heavily calcified lesions (Jacobs et al. 2006; Conrad et al. 2006). Intentional subintimal dissection with true lumen re-entry, as first described by Bolia et al., is an appealing alternative strategy for treatment of CTOs, but it is not uncommon to fail true lumen access using a wire alone (Bolia et al. 1990). The Outback re-entry device is one of several support devices that has shown to be successful in transfemoral access, and more recently via transpedal access, when wire escalation techniques fail (Beschorner et al. 2009; Gandini et al. 2013; Patrone and Stehno 2019; Hayakawa et al. 2020). At our own practice, while the majority of femoral-popliteal CTOs can be crossed using standard techniques (mainly wire escalation therapies via transepdal or even dual access), < 5% of cases require the use of a support device. In this case series, we show that the Outback re-entry device can just as easily be utilized in high complexity lesion subsets such as femoral-popliteal CTOs, when wire escalation/dissection techniques fail. While the treatment of complex PAD via a transpedal approach is not new, the feasibility of using re-entry devices for femoral-popliteal CTOs through pedal access sites is not yet widely reported (Scott et al. 2007; Clark et al. 2016). The ability to treat complex PAD via the transpedal approach with the same armamentarium available with the femoral access site is important to realize because one of the concerns that many operators have in adopting the transpedal approach is the availability of support equipment for complex cases.
The endovascular treatment of PAD via the transpedal approach is also a possible way to follow the current trend in healthcare of providing patients with safe, effective care while decreasing costs and minimizing risks. The risks associated with femoral artery access have been well published which has led to the development of smaller, alternative access sites. In our coronary counterparts, radial access has been proven to be a safer alternative to femoral access (Kiemeneij et al. 1997; Jolly et al. 2009; Sajnani and Bogart 2013; Vora and Rao 2014). Other benefits to the transpedal approach may include less contrast utilization, less radiation exposure, and less post procedure monitoring (decreased time to ambulation). This is especially important as many of these procedures can be performed in the outpatient based lab setting – which may decrease health care costs by reducing inpatient hospital monitoring.
Ideally, transpedal retrograde revascularization using the Outback re-entry device is best suited if prior antegrade attempts are unsuccessful and in cases with at least 2 tibial vessels (should access vessel closure occur). Pedal vessel selection and determining the appropriateness of the access site should be guided by duplex ultrasound. In addition, it is important to be aware of potential procedure complications such as vessel perforation, and dissection of the treated or accessed vessel. For these reasons, the contralateral femoral site should be always prepared in case of bailout.
Limitations
This is a small, single center retrospective series of selected patients and larger studies are necessary to better evaluate safety and efficacy. For the purposes of this paper, follow-up was limited to 1 month and our results cannot be extrapolated to determine long-term vessel patency using this approach. Furthermore, the procedures were performed by operators familiar with transpedal access and the results may not be generalizable to those with less experience in the transpedal technique especially since ultrasound guided access may be difficult and time-consuming to operators unfamiliar with the approach.
While radial access was still necessary to visualize the proximal cap and length of the CTO, smaller 4-Fr sheaths are still utilized and the femoral artery is still avoided which will result in less complications. Furthermore, Clark et al. reported a case of transpedal only access for treatment of a superficial femoral artery CTO - which highlights the fact that in some cases the filling of the proximal cap through collaterals may be sufficient (therefore making radial access unnecessary) (Clark et al. 2016). Although more studies need to be performed to further evaluate the scope of PAD treatment via the transpedal access site, the ability to use re-entry devices via transpedal access is an important step towards increased utilization of alternative access sites.
Conclusion
The treatment of femoral-popliteal CTOs can be successfully performed using the Outback® Elite Re-entry device via the transpedal approach – an innovative access site that may help with the current healthcare trend of cost containment while increasing patient safety.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ACT:
-
Activated clotting time
- ATA:
-
Anterior tibial artery
- CFA:
-
Common femoral artery
- CTO:
-
Chronic total occlusion
- PDA:
-
Peripheral arterial disease
- PTA:
-
Posterior tibial artery
- RA:
-
Radial artery
- SFA:
-
Superficial femoral artery
- TP:
-
Tibioperoneal
References
Beschorner U, Sixt S, Schwarzwälder U, Rastan A, Mayer C, Noory E, Macharzina R, Buergelin K, Bonvini R, Zeller T (2009) Recanalization of chronic occlusions of the superficial femoral artery using the outback re-entry catheter: a single centre experience. Catheter Cardiovasc Interv 74:934–938. https://doi.org/10.1002/ccd.22130
Bolia A, Miles KA, Brennan J, Bell PR (1990) Percutaneous transluminal angioplasty of occlusions of the femoral and popliteal arteries by subintimal dissection. Cardiovasc Intervent Radiol 13:357–363. https://doi.org/10.1007/BF02578675
Clark TWI, Watts MM, Kwan TW (2016) Percutaneous femoropopliteal recanalization using a completely transpedal/transtibial approach. Cardiovasc Intervent Radiol 39:1750–1758. https://doi.org/10.1007/s00270-016-1427-x
Conrad MF, Cambria RP, Stone DH, Brewster DC, Kwolek CJ, Watkins MT, Chung TK, LaMuraglia GM (2006) Intermediate results of percutaneous endovascular therapy of femoropopliteal occlusive disease: a contemporary series. J Vasc Surg 44:762–769. https://doi.org/10.1016/j.jvs.2006.06.025
Gandini R, Fabiano S, Spano S, Volpi T, Morosetti D, Chiaravalloti A, Nano G, Simonetti G (2013) Randomized control study of the outback LTD reentry catheter versus manual reentry for the treatment of chronic total occlusions in the superficial femoral artery. Catheter Cardiovasc Interv 82:485–492. https://doi.org/10.1002/ccd.24742
Gerald F, Fowkes R, Rudan D, Rudan I, Aboyans V, Denenberg JO, Mcdermott MM, Norman PE, Sampson UKA, Williams LJ, Mensah GA, Criqui MH (2013) Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet 382:1329–1340. https://doi.org/10.1016/S0140-6736(13)61249-0www.thelancet.com
Hayakawa N, Kodera S, Arakawa M, Kanda J (2020) Successful re-entry using the outback® elite catheter via retrograde popliteal access with IVUS guidance for femoropopliteal occlusion: a case report. CVIR Endovasc 3:1–6. https://doi.org/10.1186/S42155-020-00156-9
Hong MS, Beck AW, Nelson PR (2011) Emerging national trends in the management and outcomes of lower extremity peripheral arterial disease. Ann Vasc Surg 25:44–54. https://doi.org/10.1016/j.avsg.2010.08.006
Jacobs DL, Motaganahalli RL, Cox DE, Wittgen CM, Peterson GJ (2006) True lumen re-entry devices facilitate subintimal angioplasty and stenting of total chronic occlusions: initial report. J Vasc Surg 43:1291–1296. https://doi.org/10.1016/j.jvs.2006.02.051
Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR (2009) Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J 157:132–140. https://doi.org/10.1016/j.ahj.2008.08.023
Kiemeneij F, Laarman GJ, Odekerken D, Slagboom T, van der Wieken R (1997) A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol 29:1269–1275. https://doi.org/10.1016/s0735-1097(97)00064-8
Kwan TW, Shah S, Amoroso N, Diwan R, Makker P, Ratcliffe JA, Lala M, Huang Y, Nanjundappa A, Daggubati R, Pancholy S, Patel T (2015) Feasibility and safety of routine transpedal arterial access for treatment of peripheral artery disease. J Invasive Cardiol 27:327–330
Pande RL, Perlstein TS, Beckman JA, Creager MA (2011) Secondary prevention and mortality in peripheral artery disease: national health and nutrition examination study, 1999 to 2004. Circulation 124:17–23. https://doi.org/10.1161/CIRCULATIONAHA.110.003954
Patel A, Parikh R, Huang Y, Liou M, Ratcliffe J, Bertrand OF, Puma J, Kwan TW (2016) Pseudoaneurysm after transpedal arterial access for evaluation and treatment of peripheral arterial disease. Cardiovasc Revasc Med 18:123–127. https://doi.org/10.1016/j.carrev.2016.10.003
Patrone L, Stehno O (2019) Retrograde insertion of the outback reentry device from a tibial artery for complex infrainguinal recanalization. CVIR Endovasc 2:47. https://doi.org/10.1186/S42155-019-0088-7
Sajnani N, Bogart DB (2013) Retroperitoneal hemorrhage as a complication of percutaneous intervention: report of 2 cases and review of the literature. Open Cardiovasc Med J 7:16–22. https://doi.org/10.2174/1874192401307010016
Scott EC, Biuckians A, Light RE, Scibelli CD, Milner TP, Meier GH, Panneton JM (2007) Subintimal angioplasty for the treatment of claudication and critical limb ischemia: 3-year results. J Vasc Surg 46:959–964. https://doi.org/10.1016/j.jvs.2007.06.031
Vora AN, Rao SV (2014) Bleeding complications after PCI and the role of transradial access. Curr Treat Options Cardiovasc Med 16:305. https://doi.org/10.1007/s11936-014-0305-6
Acknowledgements
Not applicable.
Disclosures
None of the authors have any conflict of interest to disclose as pertains to this manuscript.
Funding
The authors did not receive any funding for this publication.
Author information
Authors and Affiliations
Contributions
MG – prepared the manuscript; CFB – prepared the figures and tables; DA – took part in the interventions, was a major contributor to the discussion section; PG – took part in the interventions, reviewed and edited technical details of the performed procedures; NR and PK – reviewed and edited technical details of the performed procedures; TK – took part in the interventions; JP – provided consultation and made critical revision of the manuscript; JR – took part in the interventions, patients are under care of this physician. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our institutional review board waived formal approval for this manuscript.
Consent for publication
Consent for publication was obtained from all patients.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gorenchtein, M., Rajper, N., Green, P. et al. Transpedal approach for femoral-popliteal chronic total occlusions using the outback® elite re-entry device. CVIR Endovasc 4, 9 (2021). https://doi.org/10.1186/s42155-020-00203-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42155-020-00203-5