Abstract
Background
Patients with polytrauma (fractures of the humerus and the femur) require concurrent operative fixation. Pain originating from multiple operative sites leads to increasing doses of opioid-based analgesia, which has detrimental effects in the form of longer hospital stays, higher costs, and increased mortality.
Case presentation
In twelve patients with humerus and femur fractures, a cervical erector spinae plane block (ESPB) at the level of T1 and a lumbar ESPB at the level of L2 were administered with a catheter and continuous infusion technique for postoperative analgesia. None of these patients required opioids in the postoperative period. The catheters were removed after 48 h.
Conclusions
A dual ESPB can be used successfully in patients with multiple injuries by appropriately selecting the level of intervention, and opioid-sparing analgesia can be effectively delivered to these patients.
Similar content being viewed by others
Background
Patients with polytrauma present with unstable hemodynamics, moderate to severe pain related to injury, and pulmonary comprise related to multiple rib fractures. A general anesthetic technique though appropriate, postoperative pain relief would be challenging in terms of multiple operated limbs and intrathoracic and abdominal injuries. Untreated or inadequately treated pain increases stress response, neuro-inflammatory response, and length of hospital stays (Gadsden and Warlick 2015). Though epidural analgesia has been the cornerstone of pain management, recently, the interfascial blocks have gained considerable importance as a part of multimodal analgesia. Erector spinae plane block (ESPB) has been implemented at the cervical and lumbar areas for postoperative pain relief in proximal humerus and femoral fractures respectively (Diwan and Nair 2021, 2020).
We present a series of 12 patients with multiple injured limbs without visceral injuries who received interfascial plane blocks at 2 different sites integral to a multimodal analgesic regimen. The study was approved by the institutional review board, and written informed consent was obtained from all subjects.
Case presentation
Twelve patients (age: 22–68 years, male—8, female—4) who suffered from isolated fractures of the proximal humerus and shaft femur were to undergo open and open or close surgical fixation of the fractures of the humerus and femur respectively. The side of fractures and type of blocks are mentioned in Table 1. All patients were evaluated by specialists and optimized before surgery. None of them had brain injuries. They received intravenous paracetamol 1 g in the casualty and infusion every 8th h. Upon admission, of the 12, three patients suffering from multiple rib fractures (3 in number) and with rib fracture score (Fokin et al. 2018) of more than 7 received single bolus serratus anterior plane block (30 ml 0.2% ropivacaine and 30-μg clonidine).
After obtaining consent from the ethical committee, patients were recruited for the cervical and lumbar ESPB. Informed consent for a continuous cervical and lumbar ESPB is to be administered after general anesthesia, as an interventional pain management technique for postoperative pain relief was obtained. They were also notified in the event of pain persisting with these techniques; intravenous fentanyl as a rescue analgesic would be infused. General anesthesia was induced with a standard protocol (fentanyl, propofol, cis-atracurium, sevoflurane). Electrocardiogram, oxygen saturation, non-invasive arterial blood pressure, and end-tidal carbon dioxide were monitored intraoperatively.
Block technique
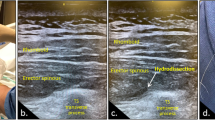
L-ESPB
The lumbar ESPB was administered at the level of the L3 transverse process (TP) identified in the parasagittal plane. An 18-G Tuohy needle was inserted from cephalad to caudal, and the tip of the needle was positioned deep to the erector spinae muscle and superficial to the tip of the L3 TP. After an initial injection of 15-ml 0.2% ropivacaine through the needle, a catheter was introduced, and the remaining 15-ml 0.2% ropivacaine was administered through the catheter (Fig. 1A).
A Lumbar ESP catheter at the level of L2 in the long axis in the non-dependant and operative side. The catheter is directed in-plane from the cephalad to the caudal. B Cervical ESP catheter at the level of T1 in the long axis in the non-dependant operative side. The catheter is directed in-plane from the caudal to the cephalad. C Subcutaneous tunnelling (SCT) of the L-ESPB catheter. D Dual ESPB (cervical—CESP and lumbar—LESP) catheter at the cervical and lumbar level. E Postoperative infusions (circled yellow) of cervical and lumbar catheters in the ICU
C-ESPB
The first rib was identified, following which a linear probe was deployed in the parasagittal plane at the first costotransverse junction. An 18-G Tuohy needle was inserted in-plane from caudal to cephalad, and the tip was positioned deep to the erector spinae and superficial to the first costotransverse junction. Initially, 10-ml 0.2% ropivacaine was injected following which a catheter was introduced, and a further 10 ml was injected.
In both blocks, the catheter (20-G multi-hole catheter) was introduced not more than 4–5 cm (Fig. 1B) and was subcutaneously tunneled (Fig. 1C). The catheter sites were labeled as cervical and lumbar ESPB (Fig. 1D), and 0.1% ropivacaine at 6 ml/h was initiated for all patients (Fig. 1E). IV paracetamol 1 g was infused 30 min before surgical closure and 12 hourly thereafter. IV fentanyl 20 μg was used as a rescue analgesic if the visual analog scale (VAS) score persisted more than 4. Pain scores were monitored at 0, 6, 12, 24, and 48 h and were 1.75, 2.5, 1.83, 1.91, and 1.66, respectively.
Catheters were appropriately positioned in all patients at both cervical and lumbar levels. There were no additional requirements for IV fentanyl in the intraoperative period. Hemodynamics were stable throughout the intraoperative period. All patients were successfully extubated postoperatively. None of these patients required IV fentanyl in the postoperative period. Three patients who had MRFs demanded additional analgesics and received intramuscular diclofenac 75 mg 8 hourly. Both catheters were removed at the end of the infusion after 48 h.
Discussion
Pain in complex trauma (multiple extremity injuries) requires the implementation of peripheral nerve blocks in conjunction with multimodal analgesia. However, with the advent of interfascial plane blocks which are safe and efficient, these are more favorable in comparison to deep-seated and technically difficult blocks.
In interfascial plane blocks, the local anesthetic (LA) is injected in a potential space between fascial layers. LA infusions in the cervical and lumbar ESPB provide motor and opioid-sparing postoperative pain relief for surgical procedures on the proximal humerus and proximal femur fractures, respectively (Diwan and Nair 2020; Taketa and Irisawa 2019). A major concern is LA toxicity with high-volume blocks and continuous infusions for 48 h. A total of 100-mg bolus of 0.2% ropivacaine was injected in the combined blocks, which is below the recommended dose of ropivacaine in elderly patients. However, none of the patients exhibited signs or symptoms of LA toxicity. In a randomized controlled trial, total plasma levobupivacaine concentrations were significantly lower in the thoracic ESPB as compared to thoracic paravertebral block (1.911 μg/ml), measured at the 20th h after the first bolus. Except for the LA molecule, the dose of the initial bolus and the infusion concentration injected were the same as in our study. Dual interfascial plane blocks are now combined to add benefits to the individual block and provide longer-lasting analgesic effects than the peripheral nerve blocks (Xia et al. 2021).
Conclusions
With this case series, we suggest that a dual ESPB can be used successfully in patients with multiple injuries by appropriately selecting the level of intervention, and opioid-sparing analgesia can be effectively delivered to these patients.
Availability of data and materials
Not applicable.
Abbreviations
- SAPB:
-
Serratus anterior plane block
- ICU:
-
Intensive care unit
- ESPB:
-
Erector spinae plane block
- CT:
-
Computed tomography
- MRF:
-
Multiple rib fracture
- IV:
-
Intravenous
- TP:
-
Transverse process
- VAS:
-
Visual analogue scale
- LA:
-
Local anesthesia
References
Diwan S, Nair A (2020) Erector spinae plane block for proximal shoulder surgery: a phrenic nerve sparing block! Turk J Anaesthesiol Reanim 48:331–333
Diwan S, Nair A (2021) Lumbar erector spinae plane block at L3 level for managing post-operative pain in patients undergoing surgery for proximal femur fractures. Turk J Anaesthesiol Reanim 49:477–479
Fokin A, Wycech J, Crawford M, Puente I (2018) Quantification of rib fractures by different scoring systems. J Surg Res 229:1–8
Gadsden J, Warlick A (2015) Regional anesthesia for the trauma patient: improving patient outcomes. Local Reg Anesth 8:45–55
Taketa Y, Irisawa Y, Fujitani T (2019) Comparison of ultrasound-guided erector spinae plane block and thoracic paravertebral block for postoperative analgesia after video-assisted thoracic surgery: a randomized controlled non-inferiority clinical trial. Reg Anesth Pain Med 0:1–6
Xia Q, Ding W, Lin C, Xia J, Xu Y, Jia M (2021) Postoperative pain treatment with transmuscular quadratus lumborum block and fascia iliaca compartment block in patients undergoing total hip arthroplasty: a randomized controlled trial. BMC Anesthesiol 21:188
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Contributions
SD, this author helped in conceptualization and manuscript writing—initial, performed the interventions, collected data, and did formal analysis. AN, this author helped in manuscript editing, analyzing data, and review of literature. BA, this author helped in data collection and manuscript writing. GB, This author helped in data collection and manuscript writing. PS, this author helped in review of literature, supervision, and conceptualization. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Institutional Ethics Committee, Sancheti Hospital for Orthopedics & Rehabilitation, Pune-411005, India, on 25th September 2021. Written informed consent was obtained to participate from the participant.
Consent for publication
Consent to publication has been taken. Written informed consent was obtained from the participant.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Diwan, S., Nair, A., Adhye, B. et al. Dual erector spinae plane block for complex traumas of upper and lower limb: an opioid reduction strategy—a case series. Ain-Shams J Anesthesiol 15, 81 (2023). https://doi.org/10.1186/s42077-023-00380-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-023-00380-0