Abstract
Background
Airway management by intubation is considered a major responsibility and vital skill for anaesthesiologists. Direct laryngoscopy and endotracheal intubation under vision continues to be the gold standard for airway management. Though conventional laryngoscopy is done with Macintosh blade, it has its own drawbacks. The Airtraq™ is a tube/guide channelled video-laryngoscope and can be used in patients with normal as well as difficult airway. On literature review, studies comparing intubation time with Airtraq™ and Macintosh laryngoscopes have shown heterogeneous results. Therefore, the present study was designed to compare the Airtraq™ video-laryngoscope and Macintosh laryngoscope for tracheal intubation in adults.
Results
The median time to intubation was significantly longer in group A [45 (27–77) s] than in group M [24 (21–26) s] (p < 0.001). In both groups, 96% patients had POGO score 75–100% and CL grade I. Intubation was noted to be easy in 88% cases in group A and 92% in group M (p > 0.05). Three cases in group A required a second attempt for successful intubation, whereas in group M, all cases were intubated in the first attempt (p > 0.05). Hemodynamic parameters and complications were comparable among the groups (p > 0.05).
Conclusions
Airtraq™ video-laryngoscope took longer time for intubation than Macintosh laryngoscope. However, both the devices were similar in terms of glottic view, ease of intubation, number of intubation attempts, incidence of failed intubation, hemodynamic changes, and complications. The overall performance of Airtraq™ video-laryngoscope was similar to Macintosh laryngoscope in patients having normal airways.
Similar content being viewed by others
Background
Airway management by tracheal intubation is considered a major responsibility and vital skill for anaesthesiologists. Therefore, laryngoscopy is one of the fundamental skills that should be mastered by the trainee anaesthesiologists. The most common laryngoscope used for direct laryngoscopy and intubation is Macintosh laryngoscope. For routine intubations, every anaesthesiologist must be familiar with this device (Achen et al. 2008). However, sometimes, it is not possible to obtain an adequate glottic view and exposure with this laryngoscope. Difficult laryngoscopy occurs with Macintosh laryngoscope in 2–8% of all general anaesthesia cases (Cattano et al. 2004; Rose and Cohen 1994; Combes et al. 2004).
Video-laryngoscopes were developed in an attempt to improve upon the view and success rate of direct laryngoscopy. They constitute an important part of the difficult airway cart. Conventional direct laryngoscopy with Macintosh laryngoscope involves alignment of oral, pharyngeal, and tracheal axes. However, with the introduction of video-laryngoscopes, this is no longer required. Thus, there may be less hemodynamic fluctuation and injury to local tissue (Maharaj et al. 2008). Video-laryngoscopes have also shown to produce less cervical spine movement (Hirabayashi et al. 2008). Another advantage is that these devices have a shorter learning curve relative to conventional Macintosh laryngoscope (Maharaj et al. 2006a).
The Airtraq™ video-laryngoscope is a channelled device for tracheal intubation in patients with normal or difficult airways. The anatomical curvature of the Airtraq™ blade and the special internal arrangement of the optical components allow visualisation of the glottic plane without alignment of the oral, pharyngeal, and tracheal axes (Maharaj et al. 2008).
Intuitively, it appears that Airtraq™ video-laryngoscope should take less time to intubate as it provides a better glottic view. Also, the endotracheal tube is already mounted in the slot for the purpose, and it can be easily inserted into the glottis. However, the studies comparing intubation time with Airtraq™ and Macintosh laryngoscopes have shown contradictory results. Many studies including meta-analysis have been carried out previously comparing Airtraq™ and Macintosh laryngoscopes. A few of them indicate that Macintosh laryngoscope takes less time to intubate (Bhandari et al. 2013; Rendeki et al. 2017), whereas other authors have concluded that Airtraq™ leads to faster intubation (Maharaj et al. 2006a; Yallapragada et al. 2016; McElwain et al. 2010). Because of the heterogeneity of results from previous studies, a clear consensus could not be achieved as in which device is better in terms of intubation time and other intubating conditions.
Therefore, the present study was planned to compare Airtraq™ video-laryngoscope and Macintosh laryngoscope for laryngoscopy and intubation in adults with normal airway undergoing elective surgeries under general anaesthesia. Primary outcome measure was time taken for successful tracheal intubation. The secondary outcome measures were intubating conditions in terms of glottic view as per percentage of glottic opening (POGO) score and Cormack and Lehane (CL) grade, ease of intubation, need for additional manoeuvres to facilitate intubation, number of attempts of intubation, incidence of failed intubation, hemodynamic response to laryngoscopy, and complications, if any.
Methods
This randomised trial was undertaken after obtaining approval from the Institutional Ethical Committee—Human Research (IEC-HR), University College of Medical Sciences. This study was prospectively registered with the Clinical Trials Registry of India (CTRI/2018/01/011446). This study was conducted from November 2017 to April 2019 in accordance with the Declaration of Helsinki of 1975, as revised in 2013, for experiments on human with the first case being recruited only after clinical trials registry was done. A written informed consent was obtained from all the participating subjects.
Fifty ASA I/II patients of either sex, with age ranging from 18 to 60 years, with no anticipated difficulty in airway management requiring general anaesthesia with endotracheal intubation were included. Patients with significant neurological, hepatic, renal or pulmonary disease, those with known allergies or contraindications to trial drugs, or on beta blocker therapy, undergoing emergency procedures, obstetric procedures, BMI > 35 kg/m2, and patients with history of alcohol or drug abuse were excluded.
A written informed consent for participation in the study was taken from all the patients meeting the inclusion criteria. All patients were advised to remain nil per orally for 8–10 h prior to the procedure as per the institutional policy. Tablet alprazolam 0.25 mg and ranitidine 150 mg were administered the night before and morning of surgery with a few sips of water.
Patients were randomised using a computer-generated random number table into one of the two groups, comprising 25 patients in each, group A (laryngoscopy performed by Airtraq™ video-laryngoscope) or group M (laryngoscopy performed by Macintosh laryngoscope). Group allocation was concealed until after randomisation. All intubations were performed by either one of the two senior anaesthesiologists who were trained to acquire proficiency in the use of Airtraq™ video-laryngoscope by performing minimum 20 intubations on mannequin before commencing the study. Size of the blade and the endotracheal tube (ETT) was chosen as per standard guidelines and patient profile.
In the pre-operative area, baseline heart rate, systolic and diastolic blood pressure, mean blood pressure, and SpO2 were recorded. In the operating room, monitoring in the form of lead II electrocardiography, pulse oximetry, and non-invasive blood pressure were started. An IV line was secured with an 18-G intravenous catheter. General anaesthesia was induced using injection morphine 0.1 mg/kg i.v. and propofol 1.0–2.5 mg/kg i.v. After ensuring successful bag mask ventilation with 100% O2, injection vecuronium 0.1 mg/kg i.v. was administered to facilitate laryngoscopy and placement of the ETT. All patients were ventilated with 33% O2 in N2O and isoflurane for maintenance of anaesthesia. Capnography was instituted after induction of anaesthesia. Laryngoscopy and intubation was attempted after 3 min of monitoring.
All patients were placed in sniffing position using a pillow of approximately 10 cm thickness. The glottic view was graded as per the POGO score and Cormack-Lehane (CL) grading (Ochroch et al. 1999; Levitan et al. 1998; Cormack and Lehane 1984). If the laryngoscopic view on the first laryngoscopy with the test laryngoscope turned out to be CL grade ≥ III, backward-upward-rightward pressure (BURP) manoeuvre was performed. If the grade on laryngoscopy now improved to CL grade ≤ II or the POGO score became ≥ 25%, intubation was attempted. Intubation was attempted using an appropriately sized ETT. Proper placement of ETT was confirmed by auscultation and capnography. Time to successful intubation was recorded from insertion of the blade between the teeth until the ETT is placed through the vocal cords, as confirmed by appearance of capnography waveform on the monitor. ETT was fixed after confirming bilateral equal air entry in the lung fields.
Ease of intubation was rated as easy (tracheal intubation without manoeuvre), satisfactory (tracheal intubation with manoeuvre), and difficult (tracheal intubation not possible even with manoeuvres). Hemodynamic parameters, viz., heart rate, systolic and diastolic blood pressure, mean blood pressure, and SpO2, were recorded just before starting the laryngoscopy, 1 min, 3 min, 5 min, 10 min, and 15 min after intubation. Any need for optimisation manoeuvres to facilitate intubation, total number of attempts of intubation, and failed intubation were also recorded. Incidence of hypoxemia (SpO2 ≤ 90%), mucosal damage with blood staining after removal of the device, and any tooth or tongue trauma were also recorded.
If intubation was not possible with the test laryngoscope, a senior anaesthesiologist took over the case, and if this attempt also failed, standard protocol for anticipated difficult intubation was followed. The case was counted as a failure to intubate with that particular laryngoscope.
Sample size calculation was done on the basis of a previous study. Considering the standard deviation of 6 s and 17 s for time taken for intubation with Macintosh and Airtraq™ laryngoscope groups respectively, a difference of 11 s has been established (McElwain et al. 2010). A minimum sample size of 25 cases was required in each group at an alpha error of 5% and power 80%. Data was entered in Microsoft excel spreadsheet. All statistical analysis was done using SPSS v.20.0. One-time measured quantitative data was analysed by unpaired Student t-test, and qualitative data was analysed using chi-square test. Hemodynamic parameters were analysed using repeated measure of ANOVA followed by Tukey’s test. A p value < 0.05 was considered significant.
Results
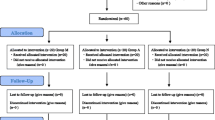
Fifty-eight patients were assessed for eligibility. Eight patients were excluded. Fifty patients were finally randomised and allocated into two groups of 25 each (Fig. 1). The demographic data is shown in Table 1.
The median time to successful intubation was significantly longer with use of Airtraq™ video-laryngoscope [45 (27–77) s] as compared to Macintosh laryngoscope [24 (21–26) s] (p-value < 0.05). In both groups, 96% patients had POGO score 75–100%. Ninety-six percent of patients had CL grade I in both groups. Intubation was observed to be ‘easy’ in 88% patients in group A and 92% patients in group M. No case of difficult intubation was observed in group M, whereas one incidence of difficult intubation was noted in group A. Both the groups were comparable in terms of glottic view, ease of intubation, and total number of intubation attempts (Table 2).
Both devices lead to a rise in heart rate and blood pressure following intubation; however, these parameters were comparable at all the observed time points among the two groups (Figs. 2 and 3). The incidence of intra and post-operative complications was similar in the two groups.
Discussion
From the results of the study, we found that the median time for successful tracheal intubation was longer with use of Airtraq™ video-laryngoscope as compared to Macintosh laryngoscope. The glottic view as per POGO score and Cormack and Lehane (CL) grade was similar with both the devices. Other outcome measures (ease of intubation, total number of intubation attempts, need for optimisation manoeuvres and hemodynamic parameters) were also comparable in both the groups. None of the patients in either group developed any clinically significant complication during the study.
Although the difference in time to successful tracheal intubation among the two groups was statistically significant but with adequate preoxygenation in a patient with normal airway, such a difference in time to intubation does not hold much clinical value. The longer intubation time with Airtraq™ in this study can be attributed to the wider and longer experience of the anaesthesiologists with the use of Macintosh laryngoscope as compared to the Airtraq™ video-laryngoscope. Some other authors have also reported results similar to our study (Yallapragada et al. 2016; McElwain et al. 2010; Trimmel et al. 2011; Chalkeidis et al. 2010).
In contrast to our study, some authors have reported shorter intubation time with Airtraq™ video-laryngoscope as compared to Macintosh (Maharaj et al. 2008, 2006a; Samal et al. 2014). This variation in study findings can be due to difference in the methodology or patient-profile included in the study. Unlike our study, Maharaj et al. (Maharaj et al. 2008) compared the two devices in patients with increased risk of difficult tracheal intubation and demonstrated the superiority of Airtraq™ over Macintosh (13.4 ± 6.3 vs 47.7 ± 8.5 respectively, p < 0.001) in difficult airway. Airtraq™ resulted in rapid intubation in both normal as well as difficult airway scenarios as compared to Macintosh in mannequins when intubation was performed by novice laryngoscopists (Maharaj et al. 2006a). A meta-analysis on Airtraq™ versus Macintosh also reported shorter intubation time with Airtraq™, especially when used by novices (Lu et al. 2011). Novice laryngoscopists having equal exposure to both Airtraq™ and Macintosh laryngoscopes eliminates the selection bias due to incorporation of experienced anaesthesiologists in the study.
Video-laryngoscopes require a higher degree of hand–eye coordination due to indirect image obtained during procedure. Also, it is now well known that guiding the ETT through mouth, till laryngeal inlet, may at times be difficult resulting into longer intubation time. In the present study, we observed that visualising the glottis with Airtraq™ was relatively easier, but passing the ETT took more time as the ETT was hitting either the epiglottis anteriorly or the arytenoids posteriorly and manoeuvring the tube through the vocal cords was not always smooth as it has to pass through a fixed slot in the device. This explains the longer time to intubation with Airtraq™ in this study.
In our study, 96% of the patients had POGO score ≥ 75% and CL grade I in both the groups. Both the devices were similar in terms of glottic view. On the other hand, some previous studies have reported a better view of the glottic inlet when assessed in terms of POGO score and CL grade with Airtraq™ video-laryngoscope as compared to Macintosh laryngoscope (Bhandari et al. 2013; McElwain et al. 2010; Owada et al. 2017). Rendeki et al. also reported use of Airtraq™ video-laryngoscope significantly improved the POGO scores compared to Macintosh laryngoscope for difficult and normal airway in mannequins (Rendeki et al. 2017).
Ease of intubation was comparable among the two groups suggesting that degree of difficulty of laryngoscopy and intubation were similar with the two test laryngoscopes. Intubation was noted to be difficult in one patient in group A, whereas no case of difficult intubation was seen in group M (p > 0.05). Some of the previous studies have concluded that tracheal intubation was easy with Airtraq™ video-laryngoscope when compared to Macintosh laryngoscope (Bhandari et al. 2013; Samal et al. 2014; Ndoko et al. 2008).
In the present study, the number of patients requiring a second attempt to achieve a successful tracheal intubation was more with the use of Airtraq™ than Macintosh laryngoscope (3 vs.0; p > 0.05). This, again, can be attributed to wider experience of the anaesthesiologists with Macintosh laryngoscope. Similar results were reported by Maharaj et al. where the median number of attempts required to intubate manikin was more with Airtraq™ video-laryngoscope as compared to Macintosh laryngoscope in high-risk difficult airway (Maharaj et al. 2008). In a different study involving adult patients with routine airway, Maharaj et al. reported no difference in number of attempts for successful intubation between Airtraq™ and Macintosh (Maharaj et al. 2006b).
In the current study, hemodynamic parameters were comparable at the observed time points among the two groups. Similar to our study, Essam et al. reported an insignificant difference in MAP and HR between Airtraq™, Macintosh, and GlideScope laryngoscope (Abdelgalel and Mowafy 2018). McElwain et al. reported a non-significant difference in hemodynamic parameters in patients with cervical immobilisation when they were intubated with Airtraq™ or Macintosh (McElwain et al. 2010).
In contrast to our results, some authors have reported less hemodynamic stimulation with Airtraq™ compared to Macintosh laryngoscopy (Maharaj et al. 2008; Savoldelli et al. 2008; Abdelgalel and Mowafy 2018). Theoretically, Macintosh blade is expected to cause more significant changes in hemodynamic parameters as its tip makes direct contact with posterior surface of epiglottis which is supplied by the internal branch of the superior laryngeal nerve. The stress response during laryngoscopy and intubation was more with Macintosh laryngoscope.
One of the previous studies have reported sympathetic response related to airway instrumentation was more with Airtraq™ as compared to Macintosh laryngoscope in adult patients when intubation was performed by anaesthesia trainees. The authors attributed prolonged intubation time to be the cause for this increased pressor response with Airtraq™ (Yallapragada et al. 2016). Prolonged intubation time leading to increased pressor response in this study can be attributed to the involvement of less experienced participants in contrast to our study where all the intubations were performed by experienced anaesthesiologists.
There were no episode of hypoxia, bradycardia, and hypo/hypertension during laryngoscopy in any group. The SpO2 remained above 99% in all groups. Blood staining of the device and ETT was observed in one patient of Macintosh group. There was no significant difference among the two groups regarding the incidence of complications. Similar to our study, Chalkeidis et al. reported no difference in complication during and after laryngoscopy and intubation in routine airway (Chalkeidis et al. 2010).
There are certain limitations of the present study. Firstly, this study was conducted on patients with normal airway. So, we do not know if the results from this study are going to be valid for patients with difficult airway. Secondly, intubations were performed by experienced anaesthesiologists. Hence, results may not be applicable to less experienced personnel. Furthermore, the element of bias due to longer experience with the use of Macintosh laryngoscope among the anaesthesiologists who performed intubations in this study as compared to Airtraq™ video-laryngoscope could not be eliminated.
Conclusions
Although the time taken for successful tracheal intubation was longer with Airtraq™ video-laryngoscope as compared to Macintosh laryngoscope, it is not much of a clinical significance in patients with normal airways. Both, Airtraq™ and Macintosh, were similar in terms of glottic view, ease of intubation and number of intubation attempts, need for optimisation manoeuvres, hemodynamic changes, and complications. Thus, we conclude that both the devices were equally effective in securing airway in patients with normal airway anatomy. Airtraq™ offers no added advantage over conventional Macintosh laryngoscope in patients having normal airways.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- ASA:
-
American Society of Anaesthesiologists
- BMI:
-
Body mass index
- BURP:
-
Backward upward rightward pressure
- CL:
-
Cormack and Lehane
- ETT:
-
Endotracheal tube
- IV:
-
Intravenous
- IQR:
-
Interquartile range
- MAC:
-
Minimum alveolar concentration
- MAP:
-
Mean arterial pressure
- MPC:
-
Mallampati class
- NS:
-
Non-significant
- POGO:
-
Percentage of glottic opening
- SD:
-
Standard deviation
- SPSS:
-
Statistical Package for Social Sciences
- vs:
-
Versus
References
Abdelgalel EF, Mowafy SMS (2018) Comparison between Glidescope, Airtraq™ and Macintosh laryngoscopy for emergency endotracheal intubation in intensive care unit: randomized controlled trial. Egypt J Anaesth 34(4):123–128
Achen B, Terblanche OC, Finucane BT (2008) View of the larynx obtained using the Miller blade and paraglossal approach, compared to that with the Macintosh blade. Anaesth Intensive Care 36(5):717–721
Bhandari G, Shahi KS, Asad M, Bhakuni R (2013) Airtraq(®) versus Macintosh laryngoscope: a comparative study in tracheal intubation. Anesth Essays Res 7(2):232–236
Cattano D, Panicucci E, Paolicchi A, Forfori F, Giunta F, Hagberg C (2004) Risk factors assessment of the difficult airway: an Italian survey of 1956 patients. Anesth Analg 99(6):1774–1779
Chalkeidis O, Kotsovolis G, Kalakonas A, Filippidou M, Triantafyllou C, Vaikos D et al (2010) A comparison between the Airtraq™® and Macintosh laryngoscopes for routine airway management by experienced anesthesiologists: a randomized clinical trial. Acta Anaesthesiol Taiwanica 48(1):15–20
Combes X, Le Roux B, Suen P, Dumerat M, Motamed C, Sauvat S et al (2004) Unanticipated difficult airway in anesthetized patients: prospective validation of a management algorithm. Anesthesiology 100(5):1146–1150
Cormack RS, Lehane J (1984) Difficult tracheal intubation in obstetrics. Anaesthesia 39:1105–1111
Hirabayashi Y, Fujita A, Seo N, Sugimoto H (2008) A comparison of cervical spine movement during laryngoscopy using the Airtraq or Macintosh laryngoscopes. Anaesthesia 63(6):635–640
Levitan RM, Ochroch EA, Rush S, Shofer FS, Hollander JE (1998) Assessment of airway visualization: validation of the percentage of glottic opening (POGO) scale. Acad Emerg Med 5(9):919–923
Lu Y, Jiang H, Zhu YS (2011) Airtraq laryngoscope versus conventional Macintosh laryngoscope: a systematic review and meta-analysis. Anaesthesia 66(12):1160–1167
Maharaj CH, Costello JF, Higgins BD, Harte BH, Laffey JG (2006a) Learning and performance of tracheal intubation by novice personnel: a comparison of the Airtraq and Macintosh laryngoscope. Anaesthesia 61(7):671–677
Maharaj CH, O’Croinin D, Curley G, Harte BH, Laffey JG (2006b) A comparison of tracheal intubation using the Airtraq™ or the Macintosh laryngoscope in routine airway management: a randomised, controlled clinical trial. Anaesthesia 61(11):1093–1099
Maharaj CH, Costello JF, Harte BH, Laffey JG (2008) Evaluation of the Airtraq™® and Macintosh laryngoscopes in patients at increased risk for difficult tracheal intubation. Anaesthesia 63(2):182–188
McElwain J, Malik MA, Harte BH, Flynn NM, Laffey JG (2010) Comparison of the C-MAC videolaryngoscope with the Macintosh, Glidescope, and Airtraq laryngoscopes in easy and difficult laryngoscopy scenarios in manikins. Anaesthesia 65(5):483–489
Ndoko SK, Amathieu R, Tual L, Polliand C, Kamoun W, El Housseini L et al (2008) Tracheal intubation of morbidly obese patients: a randomized trial comparing performance of Macintosh and Airtraq™ laryngoscopes. Br J Anaesth 100(2):263–268
Ochroch EA, Hollander JE, Kush S, Shofer FS, Levitan RM (1999) Assessment of laryngeal view: percentage of glottic opening score vs Cormack and Lehane grading. Can J Anaesth 46(10):987–990
Owada G, Mihara T, Inagawa G, Asakura A, Goto T, Ka K (2017) A comparison of the Airtraq™®, McGrath®, and Macintosh laryngoscopes for difficult paediatric intubation: a manikin study. PLoS ONE 12(2):e0171889
Rendeki S, Keresztes D, Woth G et al (2017) Comparison of VividTrac®, Airtraq®, King Vision®, Macintosh laryngoscope and a custom-made videolaryngoscope for difficult and normal airways in mannequins by novices. BMC Anesthesiol 17(1):68
Rose DK, Cohen MM (1994) The airway: problems and predictions in 18,500 patients. Can J Anaesth 41(5):372–383
Samal RK, Kundu R, Ghosh M, Singha S (2014) A comparative study of tracheal intubation characteristics using Macintosh and Airtraq™ laryngoscope. Int J Med Dent Sci 3(2):460
Savoldelli GL, Schiffer E, Abegg C, Baeriswyl V, Clergue F, Waeber JL (2008) Comparison of the Glidescope®, the McGrath®, the Airtraq™® and the Macintosh laryngoscopes in simulated difficult airways. Anaesthesia 63(12):1358–1364
Trimmel H, Kreutziger J, Fertsak G, Fitzka R, Dittrich M, Voelckel WG (2011) Use of the Airtraq™ laryngoscope for emergency intubation in the prehospital setting: a randomized control trial. Crit Care Med 39(3):489–493
Yallapragada SV, Parasa M, Vemuri NN, Shaik MS (2016) Comparison of the ease of tracheal intubation by postgraduate residents of anesthesiology using Airtraq™ and Macintosh laryngoscopes: An observational study. Anesth Essays Res 10(2):233–237
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
SM—concept, design, definition of intellectual content, literature search, data acquisition, data analysis, manuscript preparation, manuscript editing and manuscript review. SC—concept, design, definition of intellectual content, literature search, clinical studies, data analysis, critical review. RS—concept, design, definition of intellectual content, literature search, clinical studies, manuscript editing and manuscript review. SB—literature search, data acquisition, manuscript editing and manuscript review. BK—literature search, data acquisition, manuscript editing and manuscript review. All authors have read and approved the manuscript. Each author believes that the manuscript represents honest work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical Approval and/or Institutional Review Board (IRB) Approval taken in a meeting of Institutional Ethics Committee – Human Research (IEC – HR), University College of Medical Sciences, University of Delhi, on 7 October 2017, chaired by Prof. Nalin Mehta (Chairman). IEC approval number: IEC-HR/2017/32/21 dated 17 October 2017. A written informed consent was taken from all fifty participants who met the inclusion criteria.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meena, S., Chaudhary, S., Salhotra, R. et al. Comparison of Airtraq™ video-laryngoscope and Macintosh laryngoscope for tracheal intubation in adults—a randomised study. Ain-Shams J Anesthesiol 15, 30 (2023). https://doi.org/10.1186/s42077-023-00328-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-023-00328-4