Abstract
Background
Unanticipated difficult airway remains a challenge for the anesthesiologist with no established standard criteria to predict difficulty in intubation. Our aim was to correlate the pre-anesthetic ultrasonographic (USG) airway assessment parameters with Cormack-Lehane (CL) grade at direct laryngoscopy view under general anaesthesia.
This was a prospective, observational study on 150 adult patients between 18 and 70 years with the American Society of Anesthesiologist—Physical Status 1–2 requiring general endotracheal anesthesia for elective surgery.
Results
The incidence of difficult laryngoscopy was 22.7%. The sonographic distance from anterior neck surface to epiglottis (ANS-E) > 1.67 cm was observed to be a statistically significant USG predictor of difficult laryngoscopic view with sensitivity of 64.71% and specificity of 78.45% (p = 0.000). The sonographic distance from anterior neck surface to hyoid bone (ANS-H) or to anterior commissure (ANS-AC) did not corelate with difficult laryngoscopy. The ultrasound (US) parameters had higher negative than positive predictive value.
Conclusions
We found ANS-E distance to be the most significant predictor of difficult laryngoscopy in our study. USG is a useful tool to identify the “at-risk” patients for difficult airway.
Similar content being viewed by others
Background
Unanticipated difficult airway remains a challenge for the anesthesiologist. Failed or delayed intubation is associated with significant morbidity and mortality (Cook and MacDougall-Davis 2012). The incidence of difficulties encountered in perioperative airway management has been reported to range from 1 to 4% (Bajracharya et al. 2015). It is imperative to not only acquire the knowledge and skill for intubation techniques but also do careful assessment through planning and preparation. Accurate preoperative airway assessment should be performed to facilitate airway management planning.
There are many conventional bedside screening methods commonly applied such as Mallampati classification (MPC), thyromental distance (TMD), inter-incisor distance, neck movements, and neck circumference (NC) to predict difficult airway and are components of multivariate risk indices (Karkouti et al. 2000; El-Ganzouri et al. 1996; Khan et al. 2009). However, these tests have a high inter-observer variability (Reed et al. 2005) and low sensitivity and specificity (Butler and Dhara 1992; Nørskov et al. 2015). Their application in emergency and intensive care setting maybe counterproductive where the patients are uncooperative, confused and unable to follow instructions (Adhikari et al. 2011). The Modified Cormack-Lehane (CL) classification (Yentis and Lee 1998) grades the glottic view for easy or difficult intubation but depends upon direct laryngoscopy which is possible only after general anesthesia.
Ultrasound (US) of the upper airway is evolving as a useful, non-invasive tool for airway assessment in adjunct to clinical methods. However, its scope as an airway imaging technique and correlation of ultrasound guided measurements with Modified Cormack-Lehane classification is still being explored by various researchers across the globe.
Different sonographic techniques have been employed for airway evaluation in the past studies. Various airway parameters that can be measured are volume of the tongue, soft tissue thickness at the level of the hyoid bone, epiglottis and vocal cords, and visibility of the hyoid bone in sublingual ultrasound, etc. However, there is no established standard criteria to predict difficulty in intubation. Hence, we decided to study the usefulness of preoperative ultrasonographic (USG) evaluation of the airway vis-à-vis the bedside airway assessment to predict the glottic view on direct laryngoscopy in adult patients.
The primary objective was to correlate the pre-anesthetic ultrasonographic airway assessment parameters with the Modified Cormack-Lehane grade at direct laryngoscopic view under general anesthesia in adult patients. The secondary objective was to correlate the bedside parameters with Cormack-Lehane grade.
Methods
After obtaining the institutional ethics committee approval, a prospective observational study was conducted on 150 consenting adults of either sex, American Society of Anesthesiologist—Physical Status (ASA-PS) 1–2, posted for elective surgery under general endotracheal anesthesia during the period between January 2019 and July 2019.
The exclusion criteria included patients with any feature of difficult airway such as maxillofacial anomalies, restricted neck movements, cervical spine pathology, limited mouth opening, edentulous patients, skin infection over neck region, body mass index [BMI] > 35 kg/m2, tracheostomized patients, and pregnant patients. Patients requiring rapid sequence intubation or scheduled for fibreoptic tracheal intubation were also excluded.
All patients underwent a detailed preoperative history and physical examination including bedside airway evaluation on the day before surgery. The modified Mallampati class, thyromental distance, and neck circumference were noted and recorded for all patients.
All patients underwent a detailed preoperative USG assessment in the operation theatre (OT) holding area by the a credentialed point-of-care ultrasound (POCUS) anesthesiologist (Smalley et al. 2020 Aug). For sonographic assessment of the airway, the patient was made to lie supine with head in sniffing position, with mouth closed and tongue on floor of the mouth without any movement.
The linear high-frequency probe 12L SC (frequency 4–13 MHz) of the ultrasound machine (WIPRO GE VENUE 40) was used to measure the different sonographic parameters. The probe was placed on the skin in the submental region at different levels, to get the transverse view of the upper part of neck. The sonographic parameters and the way they were measured is described in Table 1. These parameters were chosen based on studies found in literature (Adhikari et al. 2011; Parameswari et al. 2017; Falcetta et al. 2018; Reddy et al. 2016; Nazir and Mehta 2018; Koundal et al. 2019; Wu et al. 2014; Koh et al. 2002; You-Ten et al. 2018; Gupta et al. 2012).
The transverse view was used for measuring—anterior neck surface to hyoid distance (ANS-H). Anterior neck surface to epiglottis distance at the level of the thyrohyoid membrane (ANS-E) and anterior neck surface to anterior commissure distance at the level of the thyroid cartilage (ANS-AC) (Figs. 1, 2, and 3).
All the clinical and sonographic parameters were observed and documented in the case record form. The time taken for the USG assessment was also documented. Subsequently, the patient was shifted to the operating room and baseline monitors of electrocardiogram, non-invasive blood pressure, and pulse oximeter were connected and values noted. The patient was placed in neutral position, without head in over extension or over flexion.
After preoxygenation with 100% O2 for 3 min, intravenous (IV) midazolam 1 mg and IV fentanyl 2 mcg/kg were administered. Induction of anesthesia with IV propofol 2 mg/kg was followed by muscle relaxation using IV atracurium 0.5 mg/kg IV and ventilation with oxygen and sevoflurane 2% for 3 min Subsequently, direct laryngoscopy was performed by an anesthesiologist (more than 2 years of experience) using an appropriate sized curved Macintosh blade, and the laryngoscopic grade as per Modified Cormack–Lehane scoring system (MCLS) was noted. External laryngeal manipulation was applied wherever appropriate (Yentis and Lee 1998; Koh et al. 2002) (Fig. 4, Table 2).
MCLS grades 1 and 2a were categorized as easy intubation (group E) and MCLS grades 2b, 3, and 4 were categorized as potentially difficult airway (group D). The patients were then intubated with an appropriate sized endotracheal tube. The number of attempts at laryngoscopy and use of any adjunct (gum elastic bougie) or use of video laryngoscope was also recorded. The rest of anesthesia and surgery was conducted as scheduled. The intubating anesthesiologist was unaware of the preoperative bedside and sonographic airway assessment parameters.
Statistical analysis
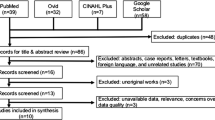
Our sample size was estimated to be 144 to predict difficult laryngoscopy with an accuracy of 87%, with 80% power and 5% level of significance based on research by Nazir I, Mehta N, on Indian patients (Nazir and Mehta 2018).
Data analysis was done using SPSS version 16. Normality test was performed before applying any statistical test. The numeric data were summarized by descriptive statistics like frequency (n) and mean ± standard deviation (SD). For statistical significance of numeric, t test was used. The categorical data were summarized by frequency count and percentage and significance analyzed using chi-square/Fisher’s exact test. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated. The correlation analysis were done using Pearson correlation test. A p value ≤ 0.05 was considered statistically significant in our study.
Results
The study was conducted on 150 consenting adult patients (69 males, 81 females) undergoing elective surgery requiring general endotracheal anaesthesia in a tertiary care hospital. There were 116 patients (77.3%) belonging to Group E and 34 patients (22.7%) in Group D of which none belonged to CL 4 (Fig. 5).
Among the demographic variables (age, gender, and BMI), age was found to be statistically significant parameter (p value 0.02) with mean ± SD of 46.3 ± 14.38 years and 55 ± 11.75 years in Group E and Group D, respectively.
The bed side parameters studied namely MPC, TMD, and NC were found to be statistically significant predictors of difficult laryngoscopy as shown in Table 3.
The mean ± SD distance of ANS-E in group E and group D was 1.5689 ± 0.2067 cm and 1.7538 ± 0.2561 cm, respectively, and was found to be significant (p = 0.000). The ANS-AC and ANS-H distance were not found to be significant (Fig. 6, Table 4).
From the receiver operating characteristic (ROC) curve, the cutoff value of ANS-E distance was found to be > 1.67 cm to predict difficult laryngoscopy with sensitivity of 64.71% and specificity of 78.45%. The AUC (area under the curve) was 0.735 having a p value was < 0.0001 (significant) (Fig. 7). The PPV and NPV of ANS-E distance were 46.81 and 88.35%, respectively (Table 5).
The average time taken to perform the USG was 3.4 min ± standard deviation of 0.407 min. No assist device was used for intubation in group E. Among 34 patients in group D, bougie was used in 6 patients and video laryngoscope was used in 13 patients to assist intubation, while 15 patients did not require any assist device for intubation.
Discussion
In recent times, POCUS is emerging as a non-invasive predictor of difficult airway (You-Ten et al. 2018). In conjunction with the clinical criteria, US parameters add value to the prediction of difficult laryngoscopic view. We embarked on this study to assess the “Usefulness of preoperative ultrasonographic evaluation of the airway vis-à-vis the bedside airway assessment to predict the potentially difficult airway on direct laryngoscopy in adult patients.”
The USG parameters used in our study were the transverse views of anterior neck surface to hyoid distance (ANS-H), anterior neck surface to epiglottis distance at the level of the thyrohyoid membrane (ANS-E), and anterior neck surface to anterior commissure distance at the level of the thyroid cartilage (ANS-AC). The simplicity of performing these parameters using a single linear transducer and hence less time-consuming made these parameters of choice for our study. These parameters are similar to those studied by Wu et al.(2014).
The other USG parameters measured in various studies to predict difficult airway were the depth of pre-epiglottic space distance which is the same as ANS-E in our study, E-VC (the distance from the epiglottis to the mid-point of the distance between the vocal cords), ratio of ANS-E and E-VC (Reddy et al. 2016; Gupta et al. 2012), volume of the tongue (Parameswari et al. 2017), volume of floor of the mouth (Parameswari et al. 2017), hyomental distance in neck neutral and neck extended position (Wojtczak 2012), hyomental distance ratio (Wojtczak 2012), and visibility of hyoid bone by sublingual USG (Tsui and Hui 2008; Hui and Tsui 2014). In our study, the sonographic view to measure the ratio of the distance from ANS-E and E-VC (oblique transverse plane bisecting the epiglottis and posterior most part of the vocal folds with arytenoids in one 2-dimensional view) was technically challenging as probe resolution had limitation. Sublingual view was not done as it required change of probe and precautions to maintain sterility resulting in extra time in the OT holding area.
Difficult laryngoscopy is generally defined as the inability to visualize the vocal cords. The original Cormack-Lehane scoring system includes only grades 3 and 4 in the difficult laryngoscopy while the true incidence of difficult laryngoscopy is underestimated as it excludes a subgroup of the original grade 2 which is difficult to manage. The MCLS system allows refining the definition of difficult laryngoscopy as including grades 2b, 3, and 4 as we have done in our study (Fig. 4). This makes the incidence of difficult laryngoscopy in our study as 22.7% although none of the patients had CL 4 grade. As the distribution of CL 4 in general population is 0.2% (Koh et al. 2002), a larger sample size than our study may probably express a higher CL 4 result.
In our study, the ANS-E distance was found to be a statistically significant predictor of difficult laryngoscopy with a cutoff value > 1.67 cm. This is in accordance with the studies by Koundal et al. (Koundal et al. 2019) in 200 patients and Imran Nazir et al. in 90 patients (cutoff value was ≥ 1.615 cm and 1.77 cm, respectively). Similarly, Wu et al. (Wu et al. 2014) in their study in Chinese population (203 patients) found that US measurements of distance from skin to epiglottis was greater in the difficult laryngoscopy group (p < 0.0001) while Pinto et al. conducted a study in Portuguese population (74 patients) and found a much higher cutoff value of 2.75 cm for the same (Pinto et al. 2016). In the systematic review and meta-analysis by Carsetti et al., it was concluded that the skin to epiglottis distance is the most studied index test in literature to predict difficult direct laryngoscopy (Carsetti et al. 2022).
ANS-H and ANS-AC were not found to be significant predictors of difficult laryngoscopy in our study. This is in accordance with study by Reddy et al., wherein they showed that ANS-hyoid distance is not indicative of difficult intubation (p = 0.857) (Reddy et al. 2016) Komatsu et al. (2007) in their study in 64 patients concluded that the thickness of pre-tracheal soft tissue at the level of the vocal cords is not a good predictor of difficult laryngoscopy. However, they conducted the study in obese patients with BMI > 35 kg/m2.
In contrast, Wu et al. in their study in Chinese population (203 patients) found that US measurements of distances from skin to the hyoid bone and to vocal cords were greater in the difficult laryngoscopy group and a potential predictor of difficult intubation (p = 0.0001) (Wu et al. 2014). Similarly in studies by Adhikari et al. (Adhikari et al. 2011) in 51 African–American patients and by Koundal et al. in 200 Indian patients, it was found that the distance from the skin to the hyoid bone is a reliable predictor of difficult laryngoscopy (p = 0.000) (Koundal et al. 2019).
Reddy et al. (2016) conducted their study in 100 patients and Ezri et al. (2003) in their study in 50 obese patients (BMI > 35 kg/m2) concluded that an abundance of pre-tracheal soft tissue at the level of vocal cords is a good predictor of difficult laryngoscopy.
These differences in results as compared to our study may be due to inclusion of CL 2b in group D (as the above mentioned studies have included CL 2b in easy laryngoscopic view group), the study population involved, their racial and ethnic variation, difference in sample size, and inter-observer variability (Balakrishnan and Chocalingam 2017; Farkas et al. 2005).
In our study, there was one patient with MPC I belonging to Group D. On analysis, we found that the patient had ANS-E distance of 1.98 cm which was more than our cutoff value (1.67 cm) to predict difficult laryngoscopy and bougie was required to assist intubation. However, his other bedside and sonographic parameters did not predict difficult laryngoscopy. This indicates that USG airway has a definitive role in predicting an unanticipated difficult airway making it a valuable application to be included in our armamentarium.
The average time taken in our study for assessment of USG parameters was 3.40 ± 0.40 min as compared to 10 min in study by Parameswari et al. (Parameswari et al. 2017). This may be because of more number of parameters included in their study. There are also some studies where the time taken was less than 1 min for their USG airway assessment (Gupta et al. 2012; Hui and Tsui 2014).
MPC is a predictor of difficult laryngoscopy as it indicates the amount of space within the oral cavity to accommodate the laryngoscope. In our study, there was statistical significance between MPC and CL grade (< 0.001). This is in accordance with study by Prakash et al. (p = 0.000) and Srinivasan et al. (p = 0.001) (Prakash et al. 2013; Srinivasan and Kuppuswamy 2017). However, one patient of MPC 1 was in group D and 21 patients of MPC III were in group E. Also, there were 18 patients belonging to group D who had either MPC I (1 patient) or II (17 patients). This is in accordance with meta-analyses of the modified Mallampati score by Lundstorm et al. who also concluded that modified Mallampati score was an inadequate predictor of difficult laryngoscopy as a stand-alone test (Lundstrom et al. 2011). Therefore, it is imperative that we evaluate another diagnostic parameter to predict the difficult intubation as an adjunct to bedside criteria.
In our study, TMD and NC were statistically significant predictors of difficult laryngoscopy (p = 0.016; p = 0.004, respectively). This is in accordance with various other studies which concluded that TMD is a significant predictor of difficult laryngoscopy (El-Ganzouri et al. 1996; Srinivasan and Kuppuswamy 2017; Chhina et al. 2018; Chara et al. 2014) and studies conducted by Chhina et al. (2018) and Brodsky et al. (Brodsky et al. 2002) wherein they found that the neck circumference had significant correlation with difficult intubation.
In our study, the ultrasound parameters had high negative predictive value than a positive predictive value. This is in accordance with the study by Parameswari et al. (2017).
Assist device in the form of bougie or video laryngoscope was used in 19 of 34 group D intubations in the current study. In other studies, gum elastic bougie, stylet, change of laryngoscopic blade, videolaryngoscope, patient repositioning, laryngeal mask airway (LMA), or fibreoptic intubation through LMA were used to assist difficult intubation (Yentis and Lee 1998; Prakash et al. 2013).
A sample size of 150 might have been inadequate to extrapolate the results to general population. The standard threshold value as observed in other racial and ethnic population in predicting difficult airway may not apply to the Indian population as mentioned by Prakash et al. (2013). Another limitation of our study is the possibility of inter-observer variability in perception of Mallampati class (Karkouti et al. 2000) and the Cormack-Lehane grade (Krage et al. 2010).
Conclusions
USG is a useful tool to identify the “at-risk” patients for difficult airway. Recognizing those at risk is a priority rather than relying on a single-bedside airway assessment parameter (All India Difficult Airway Association guidelines).
In our study, among the three USG parameters studied, ANS-E distance greater than 1.67 cm was found to be the most significant predictor of difficult airway.
Future research as a multi-centric study involving a larger cohort of Indian population is required to establish the standard value range for various USG parameters in the Indian population.
Availability of data and materials
Individual data and materials were collected in case record forms at the Fortis Hospital, Mulund, Mumbai, where the study was conducted. The data was assimilated in a master-chart for interpretation and analysis. The datasets used and analyzed are available with the corresponding author, Dr. Anita R. Chhabra on reasonable request.
Abbreviations
- USG:
-
Ultrasonographic
- CL:
-
Cormack-Lehane
- ANS-E:
-
Anterior neck surface to epiglottis
- ANS-H:
-
Anterior neck surface to hyoid
- ANS-AC:
-
Anterior neck surface to anterior commissure
- US:
-
Ultrasound
- MPC:
-
Modified Mallampati Class
- TMD:
-
Thyromental distance
- NC:
-
Neck circumference
- ASA-PS:
-
American Society of Anesthesiologist—Physical Status
- BMI:
-
Body mass index
- OT:
-
Operation theater
- IV:
-
Intravenous
- POCUS:
-
Point of Care Ultrasound
- MCLS:
-
Modified Cormack Lehane Scoring System
- Group E:
-
Easy intubation – MCLS 1 and 2a
- Group D:
-
Potentially difficult airway – MCLS 2b, 3, and 4
- SPSS:
-
Statistical Package for the Social Sciences
- SD:
-
Standard deviation
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- ROC:
-
Receiver operating characteristic
- E-VC:
-
Distance from epiglottis to mid-point of distance between vocal cords
- LMA:
-
Laryngeal mask airway
References
Adhikari S, Zeger W, Schmier C, Crum T, Craven A, Frrokaj I et al (2011) Pilot study to determine the utility of point-of-care ultrasound in the assessment of difficult laryngoscopy. Acad Emerg Med 18:754–758
Balakrishnan KP, Chocalingam PA (2017) Ethinicity and upper airway measurements: a study in South Indian population. Indian J Anaesth 61:622–628
Brodsky JB, Lemmens HJM, Brock-Utne JG, Vierra M, Saidman LJ (2002) Morbid obesity and tracheal intubation. Anesth Analg 94:732–736
Butler PJ, Dhara SS (1992) Prediction of difficult laryngoscopy: an assessment of the thyromental distance and Mallampati predictive tests. Anaesth Intensive Care 20:139–142
Carsetti A, Sorbello M, Adrario E, Donati A, Falcetta S (2022) Airway ultrasound as predictor of difficult direct laryngoscopy: a systematic review and meta-analysis. Anesth Analg 134(4):740–750
Chara L, Eleftherios V, Maria M, Anastasia T, Chryssoula S (2014) Anatomic features of the neck as predictive markers of difficult direct laryngoscopy in men and women: a prospective study. Indian J Anaesth 58:176–182
Chhina AK, Jain R, Gautam PL, Garg J, Singh N, Grewal A (2018) Formulation of a multivariate predictive model for difficult intubation: a double blinded prospective study. J Anaesthesiol Clin Pharmacol 34:62–67
Cook TM, MacDougall-Davis SR (2012) Complications and failure of airway management. Br J Anaesth 109:68–85
El-Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD (1996) Preoperative airway assessment: predictive value of a multivariate risk index. AnesthAnalg 82:1197–1204
Ezri T, Gewurtz G, Sessler DJ et al (2003) Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia 58:1111–1114
Falcetta S, Cavallo S, Gabbanelli V, Pelaia P, Sorbello M, Zdravkovic I et al (2018) Evaluation of two neck ultrasound measurements as predictors of difficult direct laryngoscopy: a prospective observational study. Eur J Anaesthesiol 35:605–612
Farkas L, Katic M, Forrest C (2005) International anthropometric study of facial morphology in various ethnic groups/races. Journal of Craniofacial Surgery 16:615–646
Gausan Ratna Bajracharya, Angela T Truong, Dam-Thuy Truong, Juan Pablo Cata. Ultrasound-assisted evaluation of the airway in clinical anesthesia practice: past, present and future. International Journal of Anaesthesiology and Pain Medicine. 2015;1(1:2):1–10
Gupta D, Srirajakalidindi A, Ittiara B, Apple L, Toshniwal G, Haber H et al (2012) Ultrasonographic modification of Cormack Lehane classification for pre-anesthetic airway assessment. Middle East J Anaesthesiol 21:835–842
Hui CM, Tsui BC (2014) Sublingual ultrasound as an assessment method for predicting difficult intubation: a pilot study. Anaesthesia 69:314–319
Karkouti K, Rose DK, Wigglesworth D, Cohen MM (2000) Predicting difficult intubation: a multivariable analysis. Can J Anaesth 47:730–739
Khan ZH, Mohammadi M, Rasouli MR, Farrokhnia F, Khan RH (2009) The diagnostic value of the upper lip bite test combined with sternomental distance, thyromental distance, and inter-incisor distance for prediction of easy laryngoscopy and intubation: a prospective study. AnesthAnalg 109:822–824
Koh LKD, Kong CF, Ip-Yam PC (2002) The Modified Cormack-Lehane Score for the grading of direct laryngoscopy: evaluation in the Asian population. Anaesth Intensive Care 30:48–51
Komatsu R, Sengupta P, Wadhwa A et al (2007) Ultrasound quantification of anterior soft tissue thickness fails to predict difficult laryngoscopy in obese patients. Anaesth Intensive Care 35:32–37
Koundal V, Rana S, Thakur R, Chauhan V, Ekke S, Kumar M (2019) The usefulness of Point of Care Ultrasound (POCUS) in preanaesthetic airway assessment. Indian J Anaesth 63:1022–1028
Krage R, Van Rijn C, Van Groeningen D, Loer SA, Schwarte LA, Schober P (2010) Cormack-Lehane classification revisited. Br J Anaesth 105:220–227
Lundstrom LH, Vester-Andersen M, Moller AM, Charuluxananan S, L’Hermite J, Wetterslev J (2011) Poor prognostic value of the modified Mallampati score: a meta-analysis involving 177,088 patients. Br J Anaesth 107:659–667
Nazir I, Mehta N (2018) A comparative correlation of pre-anaesthetic airway assessment using ultrasound with Cormack Lehane classification of direct laryngoscopy. IOSR Journal of Dental and Medical Science 17:43–51
Nørskov AK, Rosenstock CV, Wetterslev J, Astrup G, Afshari A, Lundstrøm LH et al (2015) Diagnostic accuracy of anaesthesiologists’ prediction of difficult airway management in daily clinical practice: a cohort study of 188 064 patients registered in the Danish Anaesthesia Database. Anaesthesia 70:272–281
Parameswari A, Govind M, Vakamudi M (2017) Correlation between preoperative ultrasonographic airway assessment and laryngoscopic view in adult patients: a prospective study. J Anaesthesiol Clin Pharmacol 33:353–358
Pinto J, Cordeiro L, Pereira C, Gama R, Fernandes HL, Assuncao J (2016) Predicting difficult laryngoscopy using ultrasound measurement of distance from skin to epiglottis. J Crit Care 33:26–31
Prakash S, Kumar A, Bhandari S, Mullick P, Singh R, Gogia AR (2013) Difficult laryngoscopy and intubation in the Indian population: an assessment of anatomical and clinical risk factors. Indian J Anaesth 57:569–575
Reddy PB, Punetha P, Chalam KS (2016) Ultrasonography - a viable tool for airway assessment. Indian J Anaesth 60:807–813
Reed MJ, Dunn MJG, Mckeown DW (2005) Can an airway assessment score predict difficulty at intubation in the emergency department. Emerg Med J 22:99–102
Smalley CM, Fertel BS, Broderick E (2020Aug) Standardizing point-of-care ultrasound credentialing across a large health care system. Jt Comm J Qual Patient Saf 46(8):471–476
Srinivasan C, Kuppuswamy B (2017) Comparison of validity of airway assessment tests for predicting difficult intubation. Indian Anaesth Forum 18:63–68
Tsui BC, Hui CM (2008) Sublingual airway ultrasound imaging. Can J Anaesth 55:790–791
Wojtczak JA (2012) Submandibular sonography: assessment of hyomental distances and ratio, tongue size, and floor of the mouth musculature using portable sonography. J Ultrasound Med 31:523–528
Wu J, Dong J, Ding Y (2014) Role of anterior neck soft tissue quantifications by ultrasound in predicting difficult laryngoscopy. Med Sci Monit 20:2343–2350
Yentis SM, Lee DJH (1998) Evaluation of an improved scoring system for the grading of direct laryngoscopy. Anaesthesia 53:1041–1044
You-Ten KE, Siddiqui N, Teoh WH, Kristensen MS (2018) Point-of-care ultrasound (POCUS) of the upper airway. Can J Anaesth 65:473–484
Acknowledgements
We are grateful to our Head of Department, Dr. Vijay Shetty, for being a source of constant encouragement.
We are thankful to senior consultants Dr. Nishigandha Sawant, Dr. Gita Baria, and Dr. Shashank Rane for doing the direct laryngoscopy and observing the Cormack-Lehane grade of our study patients.
Funding
There was no funding required for this study. The ultrasound machine (WIPRO GE VENUE 40), laryngoscopes, and adjunct devices belong to the Department of Anesthesia and are readily available in the operation theater of Fortis Hospital, Mulund, Mumbai.
Author information
Authors and Affiliations
Contributions
The pdf of the revised manuscript is mailed to them for approval before the corresponding author approves on site. The concept, design, and definition of the intellectual content for the study was undertaken by AC and HI. Literature search was done by all the authors. The clinical study (ultrasound of the airway) was done by AC and the observations were noted by ST. Data acquisition was primarily done by AC and ST, while the data analysis was done by all the authors. The statistical analysis was done together by all the authors. The manuscript was prepared by AC and ST, and manuscript editing was done by AC and HI. The manuscript was reviewed and approved by all the authors. The revised version of the manuscript is also read and approved by all the authors. The guarantor of the manuscript is AC. All three authors agree to be personally accountable for their contributions and ensure that questions related to accuracy or integrity are appropriately investigated and the resolution documented in literature. The authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee approval was obtained from the “Institutional Ethics Committee” at Fortis Hospital, Mulund, Mumbai.
S. No of Ethics Committee: ECR/531/Inst/MH/2014/RR-17.
(IEC submission No: IEC/2019/TH/10).
Written informed consent was obtained from all participants.
Consent for publication
Written and informed consent was obtained from all study participants for the publication of data with assurance of not revealing anyone’s identity under any circumstance.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chhabra, A.R., Thannappan, S. & Iyer, H.R. Preoperative ultrasonographic evaluation of the airway vis-à-vis the bedside airway assessment to predict potentially difficult airway on direct laryngoscopy in adult patients—a prospective, observational study. Ain-Shams J Anesthesiol 15, 2 (2023). https://doi.org/10.1186/s42077-022-00297-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-022-00297-0