Abstract
Background
Post-operative sore throat, cough, and hoarseness of voice constitute the major pharyngolaryngeal morbidities following General anesthesia with an endotracheal tube since its introduction. Pharyngolaryngeal morbidity has been reported following the use of supraglottic airway devices as well, with less frequency and severity. Lidocaine jelly, a time-tested lubricating agent with local anesthetic effects is effective in reducing the incidence and severity of pharyngolaryngeal morbidity. Steroid gel application over the endotracheal tube is an effective alternative. The aim of this work is to compare betamethasone gel and lidocaine jelly in their effects leading to the causation of pharyngolaryngeal morbidity when applied to I-gel, a commonly used supraglottic airway device in practice now.
Results
Both betamethasone gel and Lidocaine jelly were found to be equally efficacious in controlling pharyngolaryngeal morbidity following I-gel insertion. Though the incidence of post-operative sore throat (POST) was lower in the B group in the first 2 h (P=0.895) and 6 h (P=0.582) postoperatively, it was not significant. Similar results with cough (P=0.362) and hoarseness of voice (P=0.123) found after 2 h were also not statistically significant.
Conclusions
Both betamethasone gel and lidocaine jelly reduced the incidence and severity of pharyngolaryngeal morbidity following I-gel insertion and was found comparable.
Trial registration
CTRI/2017/10/010058. Registered 11th October 2017.
Similar content being viewed by others
Background
Occurrence of postoperative sore throat (POST), cough, and hoarseness of voice following surgery under general anesthesia (GA) with an endotracheal tube (ETT) is considered the major pharyngolaryngeal morbidity (PLM) which makes the patient uncomfortable, and the postoperative period distressing with bad memories to recall later during second anesthetic exposure. It delays early enteral feeding, results in disturbed sleep, prolonged hospital stay, and costs. Still, it remains unaddressed because no single treatment modality has proven very effective until now, though many non-pharmacological measures and drugs are being tried. The incidence was found to vary from 14.4 to 50% in general but found significantly less following the use of laryngeal mask airway (LMA), a popularly used supraglottic airway devices (SAD) (Endo et al. 2007; Safaeian et al. 2015). The wide variation in these figures may be presumably due to the diversity of the devices used as well as the different techniques of insertion recommended for their use. SADs includes a spectrum of devices with or without an inflatable cuff. Lower cuff pressures are associated with less POST (Seet et al. 2010). I-gel (2nd generation SAD by intersurgical), which is commonly used in practice now, proves to have a lesser POST incidence than LMA (De Montblanc et al. 2014; L’Hermite et al. 2017). However, Belena et al. found that the incidence of POST was high with I-gel when compared with LMA Supreme (Belena et al. 2015). When applied adequately over the ETT, betamethasone gel, a steroid with anti-inflammatory properties, results in significantly less PLM than lidocaine (Sumathi et al. 2008). Our primary objective was to compare the effects of these drugs amounting to PLM when used for lubrication over the I-gel before its insertion.
Methods
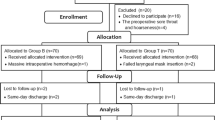
The Department of Anaesthesiology of a tertiary cancer hospital conducted an observational study including 118 patients between the age group 18 to 60 years undergoing elective surgery under GA lasting for less than 120 min. Specifically, patients who underwent breast surgeries (Modified radical mastectomy) were included. They were divided into two groups of 59 each and evaluated for PLMs post-operatively. L group received 2 ml of 2% lidocaine jelly (each ml contains 20mg lidocaine HCL so, 2ml is equivalent to 40mg lidocaine HCL) during the study period from October 2017 to February 2018 whereas the B group received 2.5 ml of 0.05% betamethasone gel over the I-gel as the lubricating agent before its insertion following anesthetic induction from March 2018 to August 2018. Those requiring more than two attempts at I-gel insertion, recent upper respiratory tract infection in the form of pharyngitis, sore throat, those on pain medications for the disease, and steroid therapy were excluded from the study.
All the patients were assessed in the pre-anesthesia clinic and were premedicated with oral alprazolam 0.25 mg and pantoprazole 40mg both on the previous day night and the morning of surgery. In the operation theatre, after securing an intravenous (IV) cannula under local anesthesia, induction was done using IV lidocaine 1.5mg/kg, propofol 2mg/kg, and fentanyl 2mcg/kg followed by vecuronium bromide 0.1 mg/kg for adequate muscle relaxation after checking adequacy for mask ventilation. In the B group, an I-gel of appropriate size according to the weight of the patient was selected and 2.5ml of 0.05% betamethasone gel (BETA GEL 20GM CREAM, MICRO LABS LIMITED) equivalent to 6.25mg was applied to the dorsum of the non-inflatable soft cuff. All the insertions were done by the anesthesiologist who has performed more than 50 I-gel insertions and follows a common standard technique of insertion. Anesthesia was maintained with nitrous oxide and oxygen in a ratio of 2:1 and sevoflurane at 1–2% to attain a MAC of 1. Residual neuromuscular blockade was adequately reversed and the device was removed once the criteria for removal were achieved. Patients were shifted to the post-anesthesia care unit (PACU) and assessed by the duty anesthesiologist for the occurrence of POST, cough, and hoarseness of voice according to a proforma at the end of 2, 6, 12, and 24 h in the postoperative period. The severity of PLM was graded as 0, 1, 2, and 3 taken as nil, mild, moderate, and severe as seen in Fig. 1 (Venugopal et al. 2016b).
The sample size was calculated based on a previous study by Sumathi et al. (2008) in a comparison between betamethasone gel and lidocaine jelly applied over ETT to reduce the incidence of PLM, assuming the power of study as 80% with a confidence level of 95%. The minimum sample size needed was 54 in each group (Sumathi et al. 2008). Considering those requiring more than 2 attempts at I-gel insertion and the duration of surgery exceeding 3 h for unforeseen reasons, an additional 5 patients were added and rounded to 59 in each group. Data obtained were entered into a Statistical Software Package for Analysis (SPSS). Categorical variables were expressed as counts and percentages; and continuous variables as mean ± standard deviation. Comparison between the study groups was carried out using the unpaired t-test for normally distributed variables and Mann-Whitney U test, for otherwise continuous data whereas chi-square tests were done for the categorical data. A p-value less than 0.05 was considered significant for all comparisons.
Results
Our study period was from October 2017 to August 18, and 118 patients were observed for 11 months. None of the candidates was excluded from the study, and the flow chart has been illustrated in Fig. 2.
The association between descriptive statistics and the type of gel used observed in the study is depicted in Table 1. Here also, the candidates in the study population were comparable in all aspects.
Table 2 illustrates the association between postoperative symptoms and the type of gel used. We could not find any significant statistical difference in POST, cough, and hoarseness of voice at 2, 6, and 12 h postoperatively between the groups. At the end of 2 h, 81 patients (41 in B and 40 in L) had no sore throat, mild sore throat corresponding to a score of 1 developed in 15 patients (46.9%of candidates) in the B group and 17 patients (53.1%) of the L group, and the results were found comparable. Moreover, 5 patients developed moderate sore throat where beta gel had a higher incidence. The difference in the incidence was not found statistically significant (P=0.895). None of the patients developed a severe sore throat. Six hours later, 103 patients had no sore throat, and 14 patients developed mild sore throat out of which 57.1% belonged to the B group and 42.9% to the L group that was found comparable (P=0.582) as seen in (Table 3). Incidence was nearly the same at 12 h postoperatively.
The overall incidence of cough was 10.1% out of which mild cough (grade 1) was observed in 33.3% in the B group against 66.7% in L during the first 2 h postoperatively which was not statistically significant (P=0.362). The mild cough persisted in the Betamethasone group even at the end of 6 and 12 h. No cough was reported in 106 cases (Table 4). Out of the 5.9% of patients reported to have hoarseness of voice, I-gel smeared with betamethasone had a higher incidence (57.1%) than the lidocaine group (42.9%) at the end of 2 h in the postoperative period; again, the observed values were not statistically significant(P=0.123) as seen in Table 5.
Discussion
The definition of sore throat varies between anesthesiologists and the severity varies among patients as it is mainly subjective and depends on one’s tolerance to pain. The insult is said to be multifactorial in origin including the size of the device selected, cuff design, the pressure generated, duration of surgery being a few leading to mechanical contact, and abrasion by the SAD in and around the glottic area (Endo et al. 2007). In ref (Endo et al. 2007), chose surgeries lasting for about 60 to 120 min under GA as a longer duration per se can contribute to PLM (Endo et al. 2007). Sore throat following the use of a laryngeal mask appears to be related to the technique of insertion, but the high intracuff pressure generated can lead to nerve palsies due to neuropraxia and nerve compression like the hypoglossal nerve palsy leading to dysphagia, dysarthria, and immobility of the tongue (Endo et al. 2007). SADs are intrinsically more invasive than a facemask but less invasive than tracheal intubation, and careful insertion techniques particularly for laryngeal mask insertion are of paramount importance in the prevention of PLM (Venugopal et al. 2016a). Studies have demonstrated a significant reduction in the incidence of POST and cough when ETT was smeared with betamethasone gel (Sumathi et al. 2008; Selvaraj and Dhanpal 2002). The beneficial effect of steroid gel application was attributed to the widespread effect of the drug on all portions of the tube that came in contact with the posterior pharyngeal wall, vocal cords, and trachea and not just confined to the tip and cuff of the tracheal tube (Selvaraj and Dhanpal 2002). Since the I-gel does not have a cuff to be inflated, the incidence of PLM is expected to be further less than the LMA in the post-operative period.
PLM is better prevented than treated. The incidence has reduced drastically with the availability of a newer generation of SADs which varies in cuff design, shape, and material, and better lubricating agents available like steroid gel. Cuffless SADs like I-gel provides an optimum seal at the laryngeal aperture with less pressure required for positive pressure ventilation which has recently gained recognition as an airway management device both in elective as well as emergencies. In a significant study of data-based systematic review done by Tanaka et al. using lidocaine as a topical preparation, the incidence of PLM was found to be significantly lower (Tanaka et al. 2015). In another interesting study, the incidence of PLM was found to be higher in women than men (Jansson et al. 2014).
In a study by Kiran.S et al., it was found that betamethasone gel resulted in a significantly lower incidence of PLM compared to 2% Lidocaine jelly, but they used Proseal LMA as the SAD (Kiran et al. 2012). Gupta et al. in their study found that the use of Strepsils lozenges resulted in a 20% reduction in the post-operative cough which was statistically significant (Gupta et al. 2014). Gargling ketamine 50 mg for the 40 s just 5 min before induction of GA and intubation was found to reduce the incidence and severity of POST in a significant way (Rudra et al. 2009). Similar results were also found with the use of oral dispersible Zinc tablets and magnesium lozenges in ameliorating POST (Sarkar and Mandal 2020; Singh et al. 2019). Rieger et al. showed that the incidence of PLMs was not directly related to the intracuff pressure transmitted to the mucosa (Rieger et al. 1997). Although hoarseness of voice seems to be a trivial adverse effect, along with sore throat and dysphagia it can lead to significant patient discomfort, anxiety, and postoperative morbidity following intubation (Ebneshahidi and Mohseni 2010). Like LMA, I-gel insertion can also lead to dislocation of the arytenoid joints causing hoarseness of voice or it may be following vocal cord paralysis which may be unilateral or bilateral (Brimacombe 1997). None of our patients had severe grades of POST according to the questionnaire. Only two cases out of 118 had a traumatic placement which was noted as a bloodstain on the dorsum of the I-gel at the end of the procedure. SADs with I-gel in particular are expected to have a lower incidence of PLM. Since the device is bulky because of the cuff, it may cause abrasive injuries in the pharyngeal mucosa if not placed gently and well lubricated. Also in patients with limited mouth opening and larger tongue where I-gel is inserted with difficulty, it can lead to abrasive injuries of the mucosa, unlike LMA which requires less space for insertion as the cuff is deflatable. Betamethasone gel acts as a lubricating agent with additional anti-inflammatory effects at the site of insult like the pharyngeal mucosa. This research work found that the outcome was comparable to lidocaine jelly used I-gel as the SAD which is cuffless and less likely to cause pharyngeal trauma, unlike other studies where either ETT or LMAs were used. But, surprisingly in a cross-sectional observational study on the incidence of POST following LMA and I-gel, it was found that both the incidence and severity were more with I-gel (Lin et al. 2020).
Regarding limitations of our study, chose only breast patients for mastectomy to limit the duration of surgery where positioning is supine and surgical duration is expected to be less than 120 min. A larger study taking other types of cases requiring positioning other than supine, an extended duration of surgery, obesity and pediatric cases taken as subsets or confounding factors may reveal whether they have a higher propensity to PLM. We didn’t have a control group with KY jelly applied over the device. We had only one male patient for mastectomy out of 118 cases and hence cannot comment whether the sex of the individual had any role in the contribution of PLM.
Conclusions
This work found that betamethasone gel was equally efficacious and even a better alternative to lidocaine jelly when they were compared to cause PLM following the insertion of I-gel.
Availability of data and materials
Based on request will provide data.
Abbreviations
- POST:
-
Post-operative sore throat
- PLM:
-
Pharyngolaryngeal morbidities
- GA:
-
General anesthesia
- ETT:
-
Endotracheal tube
- SAD:
-
Supraglottic airway devices
- MAP:
-
Mean arterial pressure
- SPSS:
-
Statistical Software Package for Analysis
- PACU:
-
Post anesthesia care unit
References
Belena JM, Nunez M, Vidal A, Gasco C, Alcojor A, Lee P et al (2015) Randomized comparison of the i-gel(TM) with the LMASupreme (TM) in anesthetized adult patients. Anaesthesist 64:271–276
Brimacombe JR (1997) Arytenoid dislocation, and the laryngeal mask airway. Anesth Analg 85:463–462
De Montblanc J, Ruscio L, Mazoit JX, Benhamou D (2014) A systematic review and meta-analysis of the i-gel ((R)) vs laryngeal mask airway in adults. Anaesthesia 69:1151–1162
Ebneshahidi A, Mohseni M (2010) Strepsils® tablets reduce sore throat and hoarseness after tracheal intubation. Anesth Analg 111(4):892
Endo K, Okabe Y, Maruyama Y, Tsukatani T, Furukawa M (2007) Bilateral vocal cord paralysis caused by laryngeal mask airway. Am J Otolaryngol 28(2):126
Gupta D, Agrawal S, Sharma JP (2014) Evaluation of preoperative Strepsilslozenges on the incidence of postextubation cough and sore throat in smokers undergoing anesthesia with endotracheal intubation. Saudi J Anaesth 8(2):244–248
Jansson M, Gupta A, Nilsson U (2014) Gender differences in sore throat and hoarseness following endotracheal tube or laryngeal mask airway: a prospective study. BMC Anesthesiol 14:56
Kiran S, Goel M, Singhal P, Gupta N, Bhardwaj M (2012) Postoperative sore throat with 0.05% betamethasone gel and 2% lignocaine jelly used as a lubricant for ProSeal LMA (PLMA) insertion. Egypt J Anaesth 28(2):139–142
L’Hermite J, Dubout E, Bouvet S, Bracoud LH, Cuvillon P, Coussaye JE et al (2017) Sore throat following three adult supraglotticairway devices: a randomised controlled trial. Eur J Anaesthesiol 34:417–424
Lin GJ, Lim YC, Wang J, Shahla S (2020) An audit of the post-operative sore throat using different laryngeal mask airways. Indian J Anaesth 64:513–516
Rieger A, Brunne B, Striebel HW (1997) Intracuff pressures do not predict laryngopharyngeal discomfort after use of the laryngeal mask airway. J Am Soc Anesthesiol 87(1):63–67
Rudra A, Ray S, Chatterjee S, Ahmed A, Ghosh S (2009) Gargling with Ketamine attenuates the postoperative sore throat. Indian J Anaesth 53:40–43
Safaeian R, Hassani V, Movasaghi G, Alimian M, Faiz HR (2015) Postoperative respiratory complications of laryngeal mask airway and tracheal tube in ear, nose, and throat operations. Anesth Pain Med 5:e25111
Sarkar T, Mandal T (2020) Preoperative oral zinc tablet decreases the incidence of postoperative sore throat. Indian J Anaesth 64:409–414
Seet E, Yousaf F, Gupta S, Subramanyam R, Wong DT, Chung F (2010) Use of manometry for laryngeal mask airway reduces postoperative pharyngolaryngeal adverse events: a prospective, randomized trial. Anesthesiology 112:652–657
Selvaraj T, Dhanpal R (2002) Evaluation of the application of topical steroids on the endotracheal tube in decreasing postoperative sore throat. J Anaesthesiol Clin Pharmacol 18:167–170
Singh NP, Makkar JK, Wourms V, Zorrilla-Vaca A, Cappellini RB, Singh PM (2019) Role of topical magnesium in postoperative sore throat: a systematic review and meta-analysis of randomized controlled trials. Indian J Anaesth 63:520–529
Sumathi PA, Shenoy T, Ambareesha M, Krishna HM (2008) Controlled comparison between betamethasone gel and lidocaine jelly applied over the tracheal tube to reduce postoperative sore throat, cough, and hoarseness of voice. Br J Anaesth 100(2):215–218
Tanaka Y, Nakayama T, Nishimori M, Tsujimura Y, Kawaguchi M, Sato Y (2015) Lidocaine for preventing postoperative sore throat. Cochrane Database Syst Rev 2015(7):CD004081
Venugopal A, Jacob RM, Koshy RC (2016a) A randomized control study comparing the pharyngolaryngeal morbidity of laryngeal mask airway versus endotracheal tube. Anesth Essays Res 10(2):189–194
Venugopal A, Jacob RM, Koshy RC (2016b) A randomized control study comparing the pharyngolaryngeal morbidity of laryngeal mask airway versus endotracheal tube. Anesth Essays Res 10(2):189–194
Acknowledgements
Authors would like to thank Institutional Review Board Members and Ethical Committee for approval of this proposed work.
Funding
There is no funding for this research work.
Author information
Authors and Affiliations
Contributions
VKE has substantially conducted and contributed to the work, and drafted and revised the manuscript. VGAN conducted and contributed to the work and assisted in the drafting and revision of the manuscript. BRD and JKPMN substantially analyzed the work and revised the intellectual content of the work. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Prior approval from the Institutional Review Board and Human Ethics committee belonging to Regional Cancer Centre Thiruvananthapuram (HEC No. 02/2017 dated 10/03/2017) including Dr Paul Sebastian, Dr P Kusumakumary, Dr K Ramachandran, Dr N Geetha. Prior registration of the study, (Registration no: CTRI/2017/10/010058) all procedures were performed in accordance to the ethical guidelines of the Declaration of Helsinki. We obtained an informed written consent to participate from adult patients and telephonic consent from relatives in this multicentric study (there was no need for consent from parent or legal guardian as pediatric patients were excluded from this study).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elumalai, V.K., Nair, V.G.A., Devi, B.R. et al. A comparative evaluation of pharyngolaryngeal morbidity following I-gel insertion after the administration of betamethasone gel versus lidocaine jelly—a prospective study. Ain-Shams J Anesthesiol 14, 75 (2022). https://doi.org/10.1186/s42077-022-00275-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-022-00275-6