Abstract
Background
Obesity has been identified as an independent risk factor for postoperative respiratory complications in several studies. In the pediatric and newborn populations, high-flow nasal oxygen (HFNO2) therapy was initially demonstrated to be an effective treatment for acute respiratory failure. It becomes increasingly popular as a therapy for adult patients, with a growing range of clinical applications.
Results
One hundred ten patients were admitted to the ICU for postoperative care after laparoscopic sleeve gastrectomy. They were examined and randomized equally into two groups: group A (HFNO2 therapy group) who received high-flow nasal oxygen therapy, group B (VMO2 therapy group) who received venturi mask oxygen therapy. The partial pressure of oxygen in arterial blood (PaO2), partial pressure of oxygen/fraction of inspired oxygen (PaO2/FiO2), respiratory rate, and length of ICU stay were recorded. The partial pressure of oxygen in the arterial blood (PaO2) was 131.764 (95% CI 124.562–138.965) in the HFNO2 group versus 106.767 (95% CI 99.565–113.968) in the VMO2 group, partial pressure of oxygen/fraction of inspired oxygen (PaO2/FiO2) was 321.81 (95% CI 307.486–336.153) in the HFNO2 group versus 276.767 (95% CI 262.433–291.100) in the VMO2 group, and respiratory rate was 20.778 (95% CI 20.172–21.385) in the HFNO2 group versus 24.047 (95% CI 23.441–24.654) in the VMO2 group, while the length of ICU stay was the HFNO2 group (1.09 ± .29 days) and (1.00 ± .000 day) in the VMO2 group.
Conclusions
In conclusion, our study has shown that high-flow nasal oxygen therapy in postoperative laparoscopic sleeve gastrectomy patients with atelectasis-maintained oxygenation represented as PaO2 and PaO2/FiO2 higher than the venturi mask and significantly decreased the respiratory rate but did not decrease the length of ICU stay when compared to venturi mask oxygen therapy.
Trial registration
Clinical trial registered with http://www.pactr.org (PACTR202108492295773).
Similar content being viewed by others
Background
Obesity is expressed as body mass index (BMI) which is the weight in kilograms divided by the height in square meters (kg/m2) of more than 30. Obesity is associated with multiple comorbidities; one should pay attention to respiratory complications. It affects lung volumes causing restrictive pattern and decreases the functional residual capacity (FRC) to the point that is less than the closing volume resulting in atelectasis and hypoxemia. Obesity also increase the minute ventilation and hence work of breathing, decreases lung compliance, and increases airway resistance. It can result in obstructive sleep apnea (OSA) (Hines and Marschall 2018).
Obesity combined with postoperative respiratory muscle dysfunction may lead to respiratory failure. As a result, obesity is associated with a higher risk of postoperative hypoxemia (Stéphan et al. 2017).
Baltieri et al. (2016) reported a 37% prevalence of atelectasis in obese patients after bariatric surgery in a retrospective observational study. Respiratory complications, on the other hand, are not uncommon in the general surgical population and have been demonstrated to lengthen hospital stays and increase death (Fulton et al. 2018).
High-flow nasal oxygen (HFNO2) therapy provides warmed humidified oxygen and low-level, flow-dependent positive airways pressure, and may be more tolerable than the continuous positive airway pressure (CPAP) or non-invasive ventilation; also, HFNO2 improves washout of nasopharyngeal dead space, resulting in improved oxygenation. In giving prophylactic support to preterm newborns after extubation, HFNO2 has been demonstrated to be both safe and non-inferior to standard CPAP (Zochios et al. 2018).
Aim of the study
The aim of this study is to compare the clinical outcome of treating postoperative laparoscopic sleeve gastrectomy surgery patients having atelectasis by using high-flow nasal oxygen therapy versus Venturi mask oxygen therapy.
Methods
After the approval of our institutional ethics committee, number FMASU M D 239/2019 and FMASU M D 239a/2019/2020, this prospective randomized, controlled, unblinded, single-center clinical trial was conducted over 110 patients (55 patients in each group) for 18 months from December 2019 to June 2021. Written informed consent was obtained from the patients or the first kin relative. The study protocol was explained to the patients before taking their informed consent.
Inclusion criteria
All patients had BMI above 40 kg/m2 from both genders, aged 18–60 years old, with preoperative Physical Status ASA III, underwent laparoscopic sleeve gastrectomy who had postoperative atelectasis confirmed clinically, by chest X-ray (CXR) and lung ultrasound in the ICU. All patients were fully conscious upon ICU admission.
Exclusion criteria
Patients were excluded due to refusal of the intervention or participation in the study, age below 18 years old and above 60 years old, pregnancy or lactation, psychiatric illness, or known comorbidities such as chronic pulmonary diseases and cardiac diseases.
All patients were admitted to the ICU for postoperative care and were randomized using a randomization table created by a computer software program, allocated by the holder of the sequence who was situated off-site and assigned in a 1:1 ratio to one of the following two groups:
-
Group A: HFNO2 therapy group: patients who were randomized to high-flow nasal oxygen therapy.
-
Group B: VMO2 therapy group: patients who were randomized to venturi mask oxygen therapy.
In the operating theater, all patients were premedicated with intravenous (IV) 8 mg ondansetron and 8 mg dexamethasone. Standard monitors were applied, an ECG, pulse oximeter, non-invasive arterial blood pressure monitor, and the arterial line was inserted. Preoxygenation was carried out for 3 min by means of a face mask with 100% oxygen. Anesthesia was classically induced by IV fentanyl 1–2 μg/kg, propofol 2 mg/kg, and atracurium 0.5 mg/kg. After endotracheal intubation, capnography was applied. The lungs were ventilated with a tidal volume of 6–8 ml/kg, FiO2 0.6, and the respiratory rate was adjusted to maintain ETCO2 between 35 and 40 mmHg. Maintenance was done with 1.5 MAC isoflurane and top-up doses of atracurium every 20 min. At the end of the surgery, the muscle relaxant was reversed and all patients were extubated and sent to the intensive care unit (ICU). All patients received 5 mg IV nalbuphine for analgesia when the pain was present (postoperative pain was assessed using a visual analog scale (VAS)) donated by VAS 4–10.
Upon ICU admission, medical history and examination of all patients were done; standard monitors were attached including continuous electrocardiogram, non-invasive blood pressure, and pulse oximeter; the arterial line was inserted in the operating room and was used for sampling (Vygon Leadercath Arterial PE - UK); arterial blood gas was obtained, CXR (13) (Parke et al. 2014); and lung ultrasound (15, Table 1) (Lee 2016, Mongodi et al. 2017) was done for assessment of atelectasis. Patients were monitored at least every 1h (for monitoring but not all readings were analyzed).
In the HFNO2 group, the HFNO2 cannula (AIRcon gen Respiratory Humidifier WILAmed, WILAmed high-flow AIR/O2 blender with flowmeter and Oxi. Plus nasal high flow kit) was applied at a flow of 30 L/min at FiO2 of 0.6 at a temperature of 36 oC. Flow and FiO2 were adjusted according to the attached HFNO2 therapy Algorithm, Fig. 1, Table 2. Weaning was also be adjusted according to it. For the VMO2 group, the venturi mask with FiO2 0.6 was applied. The FiO2 was adjusted according to the attached venturi mask oxygen therapy algorithm, Fig. 2.
High-flow nasal oxygen therapy algorithm. *1: Thoraco-abdominal asynchrony and/or persistent auxiliary muscle use. *2: The table shows escalation and de-escalation of oxygen in the HFNO2 group (Table 2). *3: Respiratory rate <25 breath/min or SpO2 ≥90%, no increased work of breathing. ABG, no respiratory acidosis (PH>7.35), no CO2 rise for > or = 10 mmHg; HFNO2, high-flow oxygen therapy; VMO2, venturi mask oxygen therapy; NIPPV, non-invasive positive pressure ventilation; IPPV, invasive positive pressure ventilation; SpO2, oxygen saturation
Data collection, measurements, and outcome
Upon ICU admission age, weight, BMI, sex, and duration of surgery were recorded. During ICU stay, the respiratory rate was recorded on admission, 1, 2, 3, 4, 8, 12, 16, 20, and 24 h, and ABGs and PaO2/FiO2 were recorded on admission, 2, 4, 8, 12, and 24 h. Chest X-ray (CXR) was done on admission assessed by Modified RAS score (13) (Parke et al. 2014). Lung ultrasound (Mindray M5 Diagnostic Ultrasound System (China)) was done on admission (using both 3C5s and L14-6s probes) as well assessed by lung U/S score for regional atelectasis (15, Table 1) (Mongodi et al. 2017). The primary outcome of this study was to compare PaO2/FiO2 during 24 h of oxygen therapy in both groups, and the secondary outcome was to compare the respiratory rate during 24 h and the length of ICU stay.
Statistical method
Data were collected, coded, tabulated, and then analyzed using the SPSS software package (SPSS for Windows®, Version 16.0. Chicago, SPSS Inc.). Numerical variables were presented as mean (standard deviation), and categorical variables were presented as frequency (%). Between-group comparisons were done using unpaired t test and Fisher’s exact test, for numerical variables and categorical variables, respectively. Repeated-measured variables were analyzed using repeated-measures ANOVA. Sphericity assumption of repeated-measures ANOVA was tested using Mauchly’s test of sphericity. A greenhouse-Geisser correction was applied whenever a lack of sphericity was evident. Error bars represent a 95% confidence interval. Any difference with a p-value < 0.05 was considered statistically significant.
Sample size
The sample size was calculated using the STATA program, setting the type-1 error (α) at 0.05 and the power (1-β) at 0.8. The result from a previous study (Testa et al. 2014) showed that the mean PaO2/FiO2 was 140±90 among conventional oxygen therapy compared to 190±100 among the HFNO2 group. Calculation according to these values produced a minimal sample size of 52 cases per group approximated to 55 per group (total 110).
Results
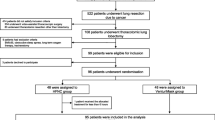
Between December 2019 and June 2021, 122 patients underwent laparoscopic sleeve gastrectomy surgery with successful extubation and 12 were excluded as shown in the CONSORT flow chart (Fig. 3 and Table 3).
PaO2 was found to be significantly higher 131.764 (95% CI 124.562–138.965) in the HFNO2 group versus 106.767 (95% CI 99.565–113.968) in the VMO2 group (p-value < 0.001). PaO2/FiO2 was found to be significantly higher 321.81 (95% CI 307.486–336.153) in the HFNO2 group versus 276.767 (95% CI 262.433–291.100) in the VMO2 group (p-value < 0.001). The PaO2/FiO2 was maintained in both groups till the 8 h reading. That was followed by a comparable gradual increase in PaO2/FiO2 in both groups (p-value > 0.05), but higher in the HFNO2 group than in the VMO2 group (p-value < 0.05) as shown in Fig. 4 and Table 4.
The respiratory rate was found to be significantly lower 20.778 (95% CI 20.172–21.385) in the HFNO2 group versus 24.047 (95% CI 23.441–24.654) in the VMO2 group, noted from the first hour (p-value < 0.001). That was followed by a continuous drop till 12 h after initiation. Then, the respiratory rate was maintained till the end of the study in both groups as shown in Fig. 5 and Table 5.
The length of the ICU stay was 1.09 ± .29 days in the HFNO2 group when compared to 1.00 ± .000 day in the VMO2 group (p-value 0.002), but this difference is about 2 h and 10 min as shown in Table 5.
Discussion
In our study, postoperative laparoscopic sleeve gastrectomy surgery patients with confirmed atelectasis by chest auscultation, mRAS score, and lung ultrasound examination (lung US score) were randomly assigned to either the HFNO2 group or VMO2 group. The study showed that HFNO2 resulted in a significantly higher oxygenation represented by PaO2, PaO2/FiO2, and effectively decrease the respiratory rate.
Comparing both groups across the first 24 h postoperatively, they showed a statistically significant increase in PaO2/FiO2 along the 2-h, 4-h, and 24-h values with p-value < 0.05 as shown in Table 4 and Fig. 4. They also showed a statistically significant decrease in respiratory rate along the first 12 h with a p-value < 0.05 as shown in Table 5 and Fig. 5.
Maurizio et al. study showed that oxygenation for the same set FiO2 was improved by HFNO2 therapy when compared to the venturi mask in patients with acute respiratory failure in the post-extubation period, and PaO2/FiO2 was 287.2 ± 74.3 versus 247.4 ± 80.6 mmHg (p-value 0.03). In addition to that, the HFNO2 therapy decreased the respiratory rate with a mean difference of 4 ± 1 breaths/minute (Maurizio et al. 2014).
Yu et al. underwent a multicenter randomized interventional trial showed that the application of HFNO2 therapy to patients who underwent thoracoscopic lobectomy after the extubation could decrease the risk of hypoxemia (29.62% with conventional oxygen therapy, 12.51% with HFNO2) and reintubation as well as improve oxygenation represented by PaO2, PaO2/FiO2, and SaO2/FiO2 when compared to conventional oxygen (p-value < 0.05) (Yu et al. 2017).
Testa et al. found that the HFNO2 therapy was not able to affect the partial pressure of carbon dioxide in the arterial blood (PaCO2) in the pediatric population following open-heart surgeries. PaCO2 was used as a primary endpoint as the patients had both cyanotic and cyanotic heart diseases; however, HFNO2 was found to improve PaO2 levels in both categories, and PaO2 was significantly higher in HFNO2 (p-value 0.01). PaO2/FiO2 was found to be also statistically significant (p-value < 0.001) (Testa et al. 2014).
According to Corley’s study, using the HFNO2 therapy resulted in a decrease in respiratory rate by 3.4 breaths/min (95% CI 1.7–5.2) and improved oxygenation. Thus, HFNO2 therapy may be a useful treatment option for patients experiencing respiratory dysfunction post-cardiac surgery, especially those who cannot tolerate non-invasive ventilation and those with BMI ≥ 30 kg/m2 (Corley et al. 2011).
In contradiction to the previous studies, in patients with a BMI ≥ 30 kg/m2, direct extubation onto HFNO2 therapy following cardiac surgery did not improve atelectasis, oxygenation (PaO2/FiO2 in the 24 h post-extubation with a mean of 227.9 for HFNO2 and 253.3 for the control group with p-value 0.08), and respiratory rate (mean was 16.7 in control the group and 17.24 in HFNO2 with a difference of 0.54 and p-value 0.17) when compared to standard oxygen therapy, or reduce the need for escalation of respiratory support, a result found by Corley et al. They suggested further research clarifying the role of HFNO2 therapy (Corley et al. 2015).
As regards the length of the ICU stay in our study, there was the significantly longer length of ICU stay (1.09 ± .29 days) in the HFNO2 group when compared to (1.00 ± .000 day) in the VMO2 group, yet it is clinically insignificant as the increased duration in HFNO2 group can be attributed to the longer weaning of high-flow nasal oxygen therapy applied in our study protocol.
According to Xiang et al., when compared to conventional oxygen therapy, HFNO2 therapy reduced the rate of intubation or non-invasive ventilation for respiratory failure in postoperative patients at high risk of pulmonary complications, but did not reduce the length of stay in the hospital or ICU, the rate of oxygen requirement after discontinuation, or hypoxemia. Although HFNO2 does not reduce mortality, there was little harm associated with its usage, suggesting that it could be a better alternative to conventional oxygen therapy in postoperative patients at high risk of pulmonary complications. Future studies should concentrate on determining which subgroups of postoperative patients are most likely to benefit from HFNO2 therapy (Xiang et al. 2021).
Study limitations
Our study has some limitations, it has a relatively short duration and was limited to 24 h. PaCO2 was not analyzed and the 2-h difference in the ICU stay may not be attributable to the interventions being practiced, but due to logistic issues or the longer weaning hours of the HFNO2 as mentioned in its algorism, the pain assessment was not analyzed and patient satisfaction was not studied, data about complications was not collected, follow-up with CXR and lung U/S were not recorded and analyzed, and hospital stay was not studied; these data can be considered in future studies.
Conclusions
In conclusion, our study has shown that high-flow nasal oxygen therapy in postoperative laparoscopic sleeve gastrectomy patients with atelectasis-maintained oxygenation represented as PaO2 and PaO2/FiO2 higher than the venturi mask and significantly decreased the respiratory rate but did not decrease the length of the ICU stay when compared to venturi mask oxygen therapy.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due [Publishing the clinical data about any study conducted in our hospitals and approved by the institutional ethical committee is against the policy of the Faculty of medicine, Ain Shams university unless there is a reasonable request] but are available from the corresponding author on reasonable request.
Abbreviations
- HFNO2 :
-
High-flow nasal oxygen
- VMO2 :
-
Venturi mask oxygen
- PaO2 :
-
Partial pressure of oxygen in arterial blood
- PaO2/FiO2 :
-
Partial pressure of oxygen/fraction of inspired oxygen
- ICU:
-
Intensive care unit
- BMI:
-
Body mass index
- FRC:
-
Functional residual capacity
- CPAP:
-
Continuous positive airway pressure
- ASA:
-
American Society of Anesthesiologists
- CXR:
-
Chest X-ray
- mRAS:
-
Modified radiological atelectasis
- Lung U/S:
-
Lung ultrasound
- PaCO2 :
-
Partial pressure of carbon dioxide in arterial blood
- OSA:
-
Obstructive sleep apnea
References
Baltieri L, Peixoto-Souza F, Rasera-Junior I, de Lima Montebelo M, Costa D, Pazzianotto-Forti EM (2016) Analysis of the prevalence of atelectasis in patients undergoing bariatric surgery. Braz J Anesthesiol (English Edition) 66(6):577–582
Corley A, Bull T, Spooner AJ, Barnett AG, Fraser JF (2015) Direct extubation onto high-flow nasal cannulae post-cardiac surgery versus standard treatment in patients with a BMI≥ 30: a randomised controlled trial. Intens Care Med 41(5):887–894
Corley A, Caruana LR, Barnett AG, Tronstad O, Fraser JF (2011) Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Bri J Anaesth 107(6):998–1004
Fulton R, Millar J, Merza M, Johnston H, Corley A, Faulke D, Fraser J (2018) High flow nasal oxygen after bariatric surgery (OXYBAR), prophylactic post-operative high flow nasal oxygen versus conventional oxygen therapy in obese patients undergoing bariatric surgery: study protocol for a randomised controlled pilot trial. Trials 19(1):402
Hines R, Marschall K (2018) Stoelting’s Anesthesia and Co-existing Diseases. Nutritional diseases, obesity and malnutrition. Seventh edition, pp 385–391
Lee J (2016) Lung Ultrasound in Critically Ill Patients. Korean J Crit Care Med 31(1):4–9
Maurizio MS, Antonio IF, Vaschetto R, Festa R, Cataldo A, Antonicelli F, Montini L, Navalesi P, Antonelli M (2014) Nasal high-flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med 190(3):282–288
Mongodi S, Bouhemad B, Orlando A, Stella A, Tavazzi G, Via G, Mojoli F (2017) Modified lung ultrasound score for assessing and monitoring pulmonary aeration. Ultraschall Med-Eur J Ultrasound 38(05):530–537. https://doi.org/10.1055/s-0042-120260
Parke R, McGuinness S, Milne D, Jull A (2014) A new system for assessing atelectasis on chest x-ray after sternotomy for cardiac surgery. Med Imaging Radiol 2(1):2
Stéphan F, Bérard L, Rézaiguia-Delclaux S, Amaru P (2017) High-flow nasal cannula therapy versus intermittent noninvasive ventilation in obese subjects after cardiothoracic surgery. Respir Care 62(9):1193–1202
Testa G, Iodice F, Ricci Z, Vitale V, De Razza F, Haiberger R, Cogo P (2014) Comparative evaluation of high-flow nasal cannula and conventional oxygen therapy in paediatric cardiac surgical patients: a randomized controlled trial. Interact Cardiovasc Thorac Surg 19(3):456–461
Xiang GL, Wu QH, Xie L, Song JQ, Wu X, Hao SY, Zhong M, Li SQ (2021) High flow nasal cannula versus conventional oxygen therapy in postoperative patients at high risk for pulmonary complications: A systematic review and meta-analysis. Int J Clin Pract 75(3):e13828
Yu Y, Qian X, Liu C, Zhu C (2017) Effect of high-flow nasal cannula versus conventional oxygen therapy for patients with thoracoscopic lobectomy after extubation. Can Respir J 2017. https://doi.org/10.1155/2017/7894631
Zochios V, Collier T, Blaudszun G, Butchart A, Earwaker M, Jones N, Klein A (2018) The effect of high-flow nasal oxygen on hospital length of stay in cardiac surgical patients at high risk for respiratory complications: A randomised controlled trial. Anaesthesia 73(12):1478–1488
Acknowledgements
Not applicable.
Funding
Self- funded.
Author information
Authors and Affiliations
Contributions
MA designed the study, revised literature, followed the patients and critically reviewed the manuscript. GA designed the study, analyse the data, wrote and critically revised the manuscript. MH and AF revised literature followed the patients. AA collected the data, performed the analysis and wrote the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by ethical committee of Ain Shams University with approval number (FMASU M D 239 / 2019 and FMASU M D 239a /2019 / 2020). Written informed consent was obtained from the patients or the first kin relative. This clinical trial is retrospectively registered by PACTR, PACTR202108492295773 Registered 26 August 2021 - http://www.pactr.org/ PACTR202108492295773.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Modified RAS score
The modified radiological atelectasis score (m-RAS):
Including the lingua, each lobe is scored 0–3 as shown below. The scores of the six lobes are then summed to give a (0–18) score.
0=Normal
1=Plate or minor infiltrate
2=Moderate atelectasis
3=Total atelectasis (Parke et al. 2014)
Appendix 2
Lung ultrasound score
To assess the lateral chest wall, patients were examined in a semi-recumbent position with arms abducted. The anterior and posterior axillary lines divide each hemi-thorax into anterior, lateral, and posterior areas. The regions were further divided into upper and lower sections, resulting in a total of 6 regions in each hemi-thorax, allowing for the evaluation of the dependent lungs (Lee 2016)
The probe was applied for both longitudinal and transverse views, and the score was calculated as shown in Table 2 with a total of 36.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Allam, A.A.N.N.A., Elsersi, M.H.S.A., Elkady, G.A.M.A. et al. A comparative study between high-flow nasal oxygen therapy and venturi mask oxygen therapy for postoperative laparoscopic bariatric surgery patients with atelectasis: a randomized clinical trial. Ain-Shams J Anesthesiol 14, 38 (2022). https://doi.org/10.1186/s42077-022-00238-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-022-00238-x