Abstract
Use of succinylcholine in neonates is surrounded by many controversies. The need to review this topic stems from the fact that though there is an abundance of information, but there are divergent views regarding its use in neonates. We have analyzed the incidence of intubation attempts, bradycardia, and hemodynamic changes in clinical settings.
The authors conducted a meta-analysis and systematic literature search to ascertain the risks and benefits of using succinylcholine in neonatal intubation by conducting a review in the online databases of PubMed, Cochrane, Scopus, Embase, Elsevier, and Google scholar. The combination of keywords used for the search included “Succinylcholine,” “succinylcholine” AND “neonates,” “neonates” AND “difficult airway,” “neuromuscular blockers” AND “neonates,” and “non-depolarizing neuromuscular blockers” AND “neonates”. The severe adverse reactions associated with use of succinylcholine include bradycardia, asystole, hyperkalemia, and apnea. The number of attempts required for intubation was significantly lower in the patients receiving succinylcholine as compared to those who did not receive succinylcholine. Evidence suggests that conscious awake intubation leads to adverse physiological responses in neonates. The main recommended indications for using succinylcholine include emergency intubation in laryngospasm, full stomach, difficult airway, absent intravenous access, and controlled endotracheal intubation in the neonatal intensive care unit. Hence, the use of succinylcholine can be rationally accepted after considerations of the pre-operative clinical status of the neonate and risk-benefit ratio with more research further to build up strong evidence for the most appropriate agents for use in neonatal patients.
Similar content being viewed by others
Key messages
-
It is important to understand that the primary goal during any intubation procedure is achieving safe and rapid securing of the airways with least adverse effects.
-
The number of attempts required for intubation was significantly lower in the patients receiving succinylcholine as compared to those who did not receive succinylcholine.
-
The recommended indications for use of succinylcholine for tracheal intubation include full stomach, emergency intubation in laryngospasm, difficult airway, controlled endotracheal intubation in neonatal intensive care unit (NICU). In advent of absent intravenous (IV) access it can be given intramuscular (IM).
-
Atropine premedication is effective in preventing succinylcholine-induced bradycardia and asystole.
Background
Succinylcholine was first tested as a cardiovascular agent by Hunt and Taveau for what was later discovered to be an adverse effect (Hunt et al., 1906). It is already well known that the use of succinylcholine in neonates can be associated with various potentially life-threatening complications (Woelfel et al., 1994). What is the appropriate place of succinylcholine in the current clinical practice? The aim of this study was to systematically review all available evidence from trials reporting various adverse events with succinylcholine in neonates and to conduct a meta-analysis. This would contribute in improving predictability of these events and taking measures to prevent them.
Methods
Literature search strategy
We performed search for literature between 1990 and July 2020 to identify published literature on use of succinylcholine in neonates. A systematic literature search was conducted for this review in the online databases of PubMed, PubMed Central, Cochrane, Scopus, Embase, Elsevier Clinical Key, and Google scholar. A well-formulated PICOS framework was employed to execute this research. The combination of keywords used for the search included “Succinylcholine,” “succinylcholine” AND “neonates,” “neonates” AND “difficult airway,” “neuromuscular blockers” AND “neonates,” “non-depolarizing neuromuscular blockers” AND “neonates,” and “Sugammadex.” Some publications were also retrieved through cross-references from published articles.
Data analysis
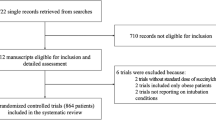
Owing to the limited literature on use of succinylcholine in neonates, we performed our search giving the highest consideration to systematic reviews and meta-analysis followed by randomized controlled trials (RCTs), observational studies, case series, and case reports. We have excluded the studies in non-English language, non-scientific commentaries, and reports from our analysis. From 3780 articles found in our initial search, 35 were finally included in the review and 5 studies were statistically analyzed for meta-analysis. We have performed this review in conformity with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (Fig. 1). The concern for various side effects and complications with succinylcholine nudge us to search for alternative approaches in neonates which have been researched in some studies (Table 1) (Barrington et al., 1989; Ghanta et al., 2007; Lemyre et al., 2009; Oei et al., 2002; Venkatesh et al., 2011). We evaluated 253 neonates included in these studies. Various neonatal intensive care unit (NICU) centers practice conscious and awake intubation in neonates using sedatives and analgesics like benzodiazepines or morphine (without using muscle relaxant). In our meta-analysis, we attempted to find the incidence of bradycardia, hypertension, and number of intubation attempts with succinnylcholine compared to the control group. For evaluation of the outcome of interests of this interventional [investigating an effect of succinylcholine on heart rate (HR), blood pressure (BP)] meta-analysis, data were extracted separately from the study groups. The data depicted in text, images, and tables were used as primary extraction source. A graph digitizing software (Enguage Digitizer version 10.10, @ Mark Mitchell) was used for efficiently extracting and estimation of numerical raw data whenever text numerical data were unavailable. The missing SDs were substituted with pooled SDs of other studies with similar comparison by ®[(∑ N*SD2)/∑ N] with N = sample size. When IQR and range were accessible, SD was calculated using the formula SD = range/4 and SD = IQR/1.35, respectively, as described in the Cochrane Hand Book of Systematic Reviews. Data were reported as 95% confidence intervals (CI).
Data synthesis
Incidence of the number of attempts required in both the comparator groups reported was analyzed. Time required for intubation in both groups was considered for analysis. Incidence of bradycardia was considered whenever the events were reported either individually or synonymously in the subject at least once. Mean arterial blood pressure (MBP) was considered for data evaluation and the data synthesis was similar to that followed for HR. We excluded pooled data of systolic or diastolic blood pressures. When SDs were not reported for lowest values, they were calculated from pooled SDs of the same group. Incidences of fall in saturation during intubation in both groups reported were compared and analyzed.
Meta-analysis was conducted with Review Manager (RevMan) 5.3 (Cochrane Collaboration, Copenhagen, Denmark, 2014). Random effects model was employed for all the analysis. Heterogeneity was measured and expressed as I2. For dichotomous variables (incidences of bradycardia, number of attempts, hypotension), odds ratio (OR), risk ratio (RR), or risk differences (RD) were computed by the Mantel-Haenszel (M-H) or I-V methods. Publication bias was checked with regression test for funnel plot asymmetry. The statistical significance was kept at P < 0.05.
Results
The results of comparison between groups receiving succinylcholine and the other not receiving succinylcholine for intubation from five studies conducted in neonates are enumerated as follows:
-
1.
Number of attempts: It was found from the meta-analysis that the number of attempts required for intubation was significantly lower in the patients receiving succinylcholine as compared to those who did not receive succinylcholine with p<0.00001, odds ratio (OR) of 0.24, and 95% CI 0.13–0.44. In the group not receiving succinylcholine, as high as 81% patients required multiple attempts for successful intubation as compared to 40% in the succinylcholine group.
-
2.
Time required for successful intubation: Time required for successful intubation was also faster in the succinylcholine group but was not statistically significant.
-
3.
Desaturation: The fall in oxygen saturation noticed during the process of intubation was significantly higher in the succinylcholine group with a mean difference of −15.87; 95% CI, −20.58, −11.15.
-
4.
Bradycardia: Although the heart rates decreased in both the groups, the difference in mean drop in patients administered succinylcholine was not significant (p=0.44, I2=95%).
-
5.
Hypertension: Barrington et al. reported a rise in mean arterial blood pressure in both the groups (atropine vs atropine with succinylcholine), but there was no significant difference between them.
-
6.
Increase in intracranial pressure (ICP): They also found a significantly higher rise in intracranial pressure in the atropine group compared to the succinylcholine group (Barrington et al., 1989).
Discussion
An understanding that the primary goal during any intubation procedure is achieving safe and rapid securing of the airways with least adverse effects is important. The comprehension of physiological, pharmacodynamic, and pharmacokinetic differences between the neonates and adult patients is essential to provide safe drug therapy to neonates. Total body water content and extracellular fluid (ECF) volumes are higher in neonates. The immaturity of neuromuscular junction results in intense neuromuscular blockade in neonates compared to children (Goudsouzian et al., 1981). Onset of action of neuromuscular blocking (NMB) drugs in neonates is faster than in adults (Martyn et al., 1992). However, we need to understand that the onset of action may be slower in ill neonates than their healthy counterparts. A close observation of drug effects is more useful than comprehension of expected physiologic, pharmacodynamic, and pharmacokinetic differences between neonates and adults in guiding clinical administration of drugs. This is more relevant in the case of drugs like succinylcholine, which is usually cleared very rapidly, because the faster the clearance, the greater the effect of variability in rate of equilibration on peak effect.
Main utility of succinylcholine
The mainly recommended indications for use of succinylcholine include:
-
1)
Full stomach, difficult airway, emergency intubation in laryngospasm and absent intravenous (IV) access as can give intramuscular (IM) (Gavel & Walker, 2014).
-
2)
Controlled endotracheal intubation in NICU.
-
3)
Endoscopy as for diagnostic airway intervention.
Dosage and route of succinylcholine in neonates
The dosage of succinylcholine (IV= 1–3 mg/kg, IM= 2–4 mg/kg) is governed largely by the fact that neonates have a high ECF and, hence, a higher volume of distribution. The onset of intubating conditions and total duration of action is 30–60 s and 3–12 min respectively after IV administration and 2–5 min and 10–30 min respectively after IM administration. If intubating conditions are not achieved in 1–5 min of IV injection, 1mg/kg/dose can be repeated. Intramuscular injection should be administered only when intravenous access is unavailable and in dire emergency to control airway (Shaw et al., 2014).
Contraindications of the use of succinylcholine
These include patients in acute phase injury including major burns (after 48 h till 2 years), multiple trauma and extensive skeletal muscle denervation, and muscular dystrophies, who are predisposed to severe rise in potassium levels. Family history of malignant hyperthermia (MH) and pseudocholinesterase deficiency (very rare) also falls under the category of contraindication. Administration of succinylcholine without sedation is also contraindicated unless there is an urgent life-threatening situation. Caution needs to be exercised in various circumstances while administration of succinylcholine as in congenital myxoedema which is as common as 1:3000 newborns (LaFranchi, 2011), severe hepatic insufficiency, raised intracranial pressure, and tetanus. Neonates receiving aminoglycosides or cholinesterase inhibitors should not be administered succinylcholine due to their ability to reduce the metabolism of the neuromuscular blocker and prolong paralysis.
Adverse drug reactions (ADR)
The adverse reactions associated with use of succinylcholine include bradycardia, asystole, hyperkalemia, and malignant hyperthermia (MH) which have been postulated as severe reactions. Bradycardia has been noticed more with repeated dose, IV>IM injection and by concurrent use of negative chronotropic drugs like halothane, fentanyl, and propofol (Fischer, 1999). Our meta-analysis revealed a higher incidence of bradycardia with use of succinylcholine in neonates but it was not statistically significant when compared with the patients not receiving succinylcholine. It is imperative to acknowledge that neonates, owing to their parasympathetic predominance, are already at a higher risk of bradycardia and asystole even without succinylcholine. Hence, it is noteworthy that bradycardia and asystole in neonates after administration of succinylcholine could have had various etiologies (Woelfel et al., 1994). Pretreatment with anticholinergic agents (e.g., atropine) may reduce the occurrence of hypersecretion and bradyarrhythmias that can follow the administration of succinylcholine. Other documented adverse effects include urticaria, flushing, masseter spasm, and xerophthalmia. The incidence of minor side effects like bradycardia, muscle pain, increase in intraocular, or intragastric pressure is more but easily treatable. On the contrary, the incidence of potentially life-threatening complications like MH, myoglobinuria, and cardiac arrest is rare (Kaus & Rockoff, 1994).
Pseudocholinesterase deficiency and phase 2 block
Butyrylcholinesterase (BChE) or pseudocholinesterase enzyme hydrolyzes neuromuscular blockers like succinylcholine and mivacurium and also ester group of local anesthetics. In neonates homozygous for abnormal enzyme, duration of action of succinylcholine in is not well documented (Frawley & Carden, 1994). The diagnosis of pseudocholinesterase deficiency can be formed by evaluating plasma cholinesterase level and dibucaine number (Jeevendra & Marcel, 2006). However, prolonged or high dose administration of succinylcholine can convert the characteristic depolarization block (phase I block) to a nondepolarizing type (phase II block). Lee found that neonates also exhibit phase I block after 1.5 mg/kg of succinylcholine (Lee, 1975).
Rationale behind the concern of major complications
Here, we strive to explore the altogether need to waive off the use of succinylcholine in neonates. It is noteworthy that in the UK, succinylcholine in combination with other agents is being used by 77% of neonatal intensive care units (Kelleher et al., 2009). This calls for us to find a rationale behind the concern of major complications with succinylcholine leading to avoidance in neonates and whether it is an exaggerated state of affairs. It is noteworthy that there have been innumerable administrations of succinylcholine in children without incidents. Therefore, we would discuss the facts for more clarity to the concerns associated with use of succinylcholine in neonates.
The normal range of serum potassium in neonates is 3.5–6 mEq/L. Keneally and Bush found a mean potassium level increase of 0·23 mEq/l with suxamethonium administration in children under 5 years (Keneally & Bush, 1974). This rise in potassium with a single dose is not very critical considering the wide upper limit allowable in neonates.
Another major concern with use of succinylcholine in neonates is bradycardia and asystole. The results from our analysis revealed that as compared to the control group, succinylcholine showed higher incidence of bradycardia but it was not statistically significant. It is imperative to acknowledge that neonates, owing to their parasympathetic predominance, are already at a higher risk of bradycardia and asystole even without succinylcholine. Hence, it is noteworthy that bradycardia and asystole in neonates after administration of succinylcholine could have had various etiologies (Woelfel et al., 1994). Therefore, in the absence of severe hyperkalemia, bradycardia is a preventable complication of succinylcholine. In children, another major complication from succinylcholine is cardiac arrest due to undiagnosed Duchenne muscular dystrophy. These children generally survive infancy. If there is screening for elevated creatine kinase in neonates the patients with occult myopathy can be identified by genetic testing after documentation of persistently elevated creatine kinase.
We also found significantly higher episodes of desaturation in the succinylcholine group. Hence, administration of supplemental oxygen, by insufflation or intermittent positive pressure ventilation, can reduce hypoxemia. It is noteworthy that alternative agents to succinylcholine including thiopentone, propofol, and ketamine also carry a potential risk of hypoxemia if the intubating person is unable to secure the airway promptly in neonate (Bhutada et al., 2000; De Cosmo et al., 2005). Prolonged apnea in pseudo-cholinesterase deficiency is another major concern. The incidence of abnormal pseudo-cholinesterase is yet unknown in neonates. While homozygous patients show prolonged paralysis (3 to 6 h), heterozygous patients exhibit only slightly prolonged duration of action (Viby-Morgenson, 1981; Rosenberg & Brandom, 2006). Malignant hyperthermia (MH) is another dreadful complication feared with succinylcholine. However, despite being described in newborns, the earliest reaction confirmed by tests is in a 6-month old baby (Mathur et al., 2016). There are other potent triggers of MH including halothane (LaFranchi, 2011; Duncanp, 1993).
Fast acting non-depolarizing muscle relaxants
Rocuronium with its shorter onset and longer duration of action appears a suitable paralytic drug for the non-emergent intubations. Though, studied in older children, further studies are required to study use of rocuronium in the neonatal patients (Driessen et al., 2002). As we consider the use of rocuronium in difficult airway and short procedures, we need to discuss more about sugammadex. Sugammadex is a synthetic cyclodextrin molecule that reverses the action of rocuronium by encapsulation of the free molecule and forming a stable complex. It has been investigated in adults and older children, but there is very limited data in reference to the safety and efficacy in neonates (Nag et al., 2013). Alonso et al. found that the reversal of profound rocuronium-induced neuromuscular block with sugammadex (4.0 mg/kg) in neonates was fast and complete (Alonso et al., 2014). The use of this drug is also limited by its availability and cost. Hence, more evidence is warranted to recommend use of rocuronium in neonates with difficult airway and short procedures.
Alternative modalities of tracheal intubation—awake intubation/sedative intubation
The possibility to avoid muscle relaxants altogether offers a great promise and potential in future. Endotracheal intubation has been done using a combination of propofol and alfentanil as described by Steyn et al. (Steyn et al., 1994). Neonates with craniofacial abnormalities pose a grave challenge in securing airway owing to factors like micrognathia, large tongue, and limited neck mobility. Awake intubation remains the most appropriate technique in the neonates with anticipated difficult tracheal intubation where rapid control of airway is essential. The term here refers to intubation without any muscle relaxant; using some pre-medication so that the child is relaxed while maintaining spontaneous ventilation. It has been considered a safe approach for securing airway in neonates and infants with tracheo-esophageal fistula (TEF), cystic hygroma, etc. (Brett & Davis, 2011; Bryan et al., 2005). Although awake intubation is thought to preserve airway protective reflexes, evidence suggests that conscious awake intubations lead to adverse physiological responses in neonates. It may result in complications like soft tissue trauma, bradycardia, breath-holding, laryngospasm, hypoxemia, and even aspiration. It is associated with more severe and prolonged hypoxia than compared to when anesthesia is used. We found in our analysis that multiple attempts were required in awake intubation. The increase in mean arterial and intracranial blood pressure was seen in both groups but was higher (not statistically significant) with awake intubation. Awake intubation has been associated with a marked increase in anterior fontanelle pressure of up to 250% in neonates (Friesen et al., 1987). This rise in B.P can be of special concern in neonates with pre-existing risk of BP fluctuations and high ICP like hydrocephalus and intracranial hemorrhage.3 Various studies have shown the association of hypoxemia, bradycardia, increased blood pressure, and intracranial pressures with conscious intubation of newborn (Duncan et al., 2001; Millar & Bissonnette, 1994).
Time required for successful intubation was found faster in the succinylcholine group than awake intubation but was not statistically significant. However, we acknowledge the fact that the disparity in grade of expertise of the intubating doctor in various studies could have been a contributing factor in the results. It is also noteworthy that in teaching hospitals, where the majority of intubating doctors are relatively less experienced, ensuring optimal intubating conditions can help achieve successful first attempt intubations with lower complications (Naguib et al., 2004).
Thus, the best approach with current evidence remains a subjective decision with careful analysis of the clinical status of neonate. Consideration of all the physiological and accessibility aspects and a cautious titration of the risk-benefit quotient should guide the use of succinylcholine in neonates.
Conclusions
The meticulous analysis of the concerns associated with use of succinylcholine in neonates reveals that the life-threatening reactions owing solely to succinylcholine are rare. The minor side effects on the other hand are more common but usually preventable. Succinylcholine should not be administered at random nor should any other drug. It is still a widely used muscle relaxant in difficult airway cases, full stomach, and for general anesthesia of short duration in newborns and is valuably efficacious even today. It is also safe to say that the grey areas of use of succinylcholine in neonates need further evaluation along with studies to build up strong evidence for the most appropriate agents for use in neonatal population before we decide to permanently waive off succinylcholine. To conclude, the use of succinylcholine can be rationally accepted after considerations of pre-operative clinical status of the neonate, risk-benefit ratio, and resources availability.
Availability of data and materials
Not applicable
Abbreviations
- PICOS:
-
Population, intervention, comparison, outcomes and study
- NICU:
-
Neonatal intensive care unit
- SD:
-
Standard deviation
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- MH:
-
Malignant hyperthermia
- OR:
-
Odds ratio
- RR:
-
Risk ratio
- CI:
-
Confidence interval
- NMB:
-
Neuromuscular blocker
- ICP:
-
Intra-cranial pressure
References
Alonso A, de Boer HD, Booij L (2014) Reversal of rocuronium-induced neuromuscular block by sugammadex in neonates. Eur J Anaesthesiol 52:163
Barrington KJ, Finer NN, Etches PC (1989) Succinylcholine and atropine for premedication of the newborn infant before nasotracheal intubation: a randomized, controlled trial. Crit Care Med 17(12):1293–1296
Bhutada A, Sahni R, Rastogi S, Wung JT (2000) Randomised controlled trial of thiopental for intubation in neonates. Arch DisChild Fetal Neonatal Ed 82:34–37
Brett C, Davis J. P. Anesthesia for general surgery in the neonate. Smith's Anesthesia for Infants and Children. Eighth ed 2011; 18: 554-58.
Bryan Y, Chwals W, Ovassapian A (2005) Sedation and fiberoptic intubation of a neonate with a cystic hygroma. Acta Anaesth Scan 49:122–123
De Cosmo G, Congedo E, Clemente A, Aceto P (2005) Sedation in PACU: the role of propofol. Curr Drug Targets 6:741–744
Driessen JJ, Robertson EN, Van Egmond J, Booij LHDJ (2002) Time course of action of rocuronium 0.3 mg/kg in children with and without endstage renal failure. Paediatr Anaesth 12(6):507–510
Duncan H, Zurick N, Wolf A (2001) Should we reconsider awake neonatal intubation? A review of the evidence and treatment strategies. Paediatr Anaesth 11:135–145
Duncanp G (1993) Neuromuscular diseases. In: Anaesthesia and uncommon paediatric diseases. Philadelphia: W.B Saunders, pp 672–694
Fischer DM (1999) NMBA in paediatric anaesthesia. Br J Anaesth 83(1):58–64
Frawley PG, Carden R (1994) Succinylcholine-induced prolonged apnoea in a premature neonate. Anaesth Intem Care 22:192–120
Friesen RH, Honda AT, Thieme RE (1987) Perianesthetic intracranial hemorrhage in preterm neonates. Anesthesiology 67:81–816
Gavel G, Walker MWR (2014) Laryngospasm in anaesthesia. Contin Educ Anaesth Crit Care Pain 14(2):47–51
Ghanta S, Abdel-Latif ME, Lui K, Ravindranathan H, Awad J, Oei J (2007) Propofol compared with the morphine, atropine, and suxamethonium regimen as induction agents for neonatal endotracheal intubation: a randomized, controlled trial. Pediatrics 119(6):1248–1255
Goudsouzian NG, Liu LM, Cole CS (1981) Comparison of equipotent doses of non-depolarizing muscle relaxants in children. Anesth Analg 60:862–866
Hunt R, De M, Taveau R (1906) On the physiological action of certain choline derivatives and new methods for detecting choline. British Med J 2:1788–1791
Jeevendra M, Marcel E (2006) D. Succinylcholine: New Insights into Mechanisms of Action of an Old Drug. Anesthesiology 104(4):633–634
Kaus SJ, Rockoff MA (1994) Malignant hyperthermia. Pediatr Clin North Am 41:221–237
Kelleher J, Mallya P, Wyllie J (2009) Premedication before intubation in UK neonatal units: a decade of change? Arch Dis Child Fetal Neonatal Ed 94:332–335
Keneally JP, Bush GH (1974) Changes in serum potassium after succinylcholine in children. Anaesthesia and Intensive Care 2(2):147–150
LaFranchi SH (2011) Approach to the diagnosis and treatment of neonatal hypothyroidism. J Clin Endocrinol Metab 96(10):2959–2967
Lee C (1975) Dose relationships of phase II, tachyphylaxis and train of four fade in Succinylcholine induced dual neuromuscular block in man. BrJA 47:841–845
Lemyre B, Cheng R, Gaboury I (2009) Atropine, fentanyl and succinylcholine for non-urgent intubations in newborns. Arch Dis Child Fetal Neonatal Ed 94(6):439–442
Martyn JA, White DA, Gronert GA, Jaffe RS, Ward JM (1992) Up and down regulation of skeletal muscle acetylcholine receptors. Anesthesiology 76:822–843
Mathur PR, Rundla M, Jain N, Mathur V (2016) Malignant hyperthermia in a 6-month-old infant. Saudi J Anaesth 10(3):353–355
Millar C, Bissonnette B (1994) Awake intubation increases intracranial pressure without affecting cerebral blood flow velocity in infants. Can. J. Anaesth 41:281–287
Nag K, Singh DR, Shetti AN, Kumar H, Sivashanmugam T, Parthasarathy S (2013) Sugammadex: a revolutionary drug in neuromuscular pharmacology. Anesth Essays Res. 7(3):302–306
Naguib M, Lien CA, Aker J, Eliazo R (2004) Posttetanic potentiation and fade in the response to tetanic and train-of-four stimulation during succinylcholine-induced block. Anesth Analg 98:1686–1691
Oei J, Hari R, Butha T, Lui K (2002) Facilitation of neonatal nasotracheal intubation with premedication: a randomized controlled trial. J Paediatr Child Health 38(2):146–150
Rosenberg H, Brandom BW (2006) In: Barash PG, Cullen BF, Stoelting RK (eds) Malignant hyperthermia and other pharmacogenetic disorders, 5th edn. Clinical anesthesia. Philadelphia: Lippincott Williams & Wilkins, pp 547–548
Shaw I, Trueger NS, Pirotte M (2014) Time to paralysis after intramuscular injection of neuromuscular blocking agents: a review of the literature. Ann Emerg Med 64(4):16
Steyn P, Quinna MG, Millerd C, Bestc J, Morton NS (1994) Tracheal intubation without neuro-muscular blockade in children. BrJA 72:403–406
Venkatesh V, Ponnusamy V, Anandaraj J et al (2011) Endotracheal intubation in a neonatal population remains associated with a high risk of adverse events. Eur J Pediatr 170:223–227
Viby-Morgenson J (1981) Succinylcholine neuromuscular blockade in subjects homozygous for atypical plasma cholinesterase. Anesthesiology 55:429–434
Woelfel SK, Morell RC, Berman JM (1994) In my opinion: a debate--can succinylcholine be used routinely with safety in children? J Clin Monit 10(6):422–425
Acknowledgements
None
Funding
None
Author information
Authors and Affiliations
Contributions
BG—formal analysis, definition of intellectual content, editing, conceptualization, statistical analysis, guarantor. PM—formal analysis, literature search, writing, review, editing, and data collection). All the authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gupta, B., Mishra, P. A systematic review and meta-analysis of the use of succinylcholine to facilitate tracheal intubation in neonates. Ain-Shams J Anesthesiol 13, 68 (2021). https://doi.org/10.1186/s42077-021-00185-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-021-00185-z