Abstract
Background
Lung cancer is the most frequent occurring malignancy and mostly presenting with pain. Interventional procedures reduce medications and their side effects. Rhizotomy is another modality for control of chest wall pain due to tumor invasion or somatic and neural structures. We compared the degree of pain relief in thoracic rhizotomy versus thoracic paravertebral nerve radiofrequency.
Results
Six hours postoperatively, radiofrequency (RF) ablation of dorsal root ganglia resulted in reduction of required dose of narcotics in 12 patients (80%) compared to 6 patients (40%) treated with RF ablation of TPN (P value = 0.025). After 4 weeks reduction in required narcotic dose was recorded in 80.0% of DRG patients compared to 33.3% of TPN patients (P value = 0.010). Patients’ activity improved in 11 patients (73.3%) in DRG group compared to 5 patients (33.3%) in TPN group (P value = 0.028). No significant difference in frequency of sensory loss (P value = 1.000), burning sensation (P value = 0.128) and allodynia (P value = 0.139).
Conclusion
RF ablation of DRG is superior to RF ablation of TPN in relieving thoracic pain with more improvement of patients’ activity and similar adverse outcomes.
Similar content being viewed by others
Background
Lung cancer is the most frequent occurring malignancy. There is 1.61 million new case diagnosed yearly (Siegel et al. 2014). Pain is the most common presentation in cancer patients (Caraceni and Portenoy 1999). Pain may complicate with other symptoms as depression, and fatigue (Laird et al. 2011a) and may affect daily activity (Laird et al. 2011b). Early intervention, including symptomatic management, improves quality of life (Temel et al. 2010).
Cancer may result in several types of pain with different manifestations (Portenoy and Lesage 1999). Neuropathic pain is burning or shooting in character. It results from peripheral or central nervous system injury and may complicate with sensory loss and variable response to opioids (Caraceni and Portenoy 1999; Stute et al. 2003).
Pain in lung cancer may be due to pleural invasion, chest wall invasion, or costopleural syndrome. Cancer irritates peripheral nerve endings of the C and A-delta primary afferent fibers. Stimulation of these fibers results in the recruitment of quiescent nociceptors, and the activation of NMDA-receptor-channel complex leading to dorsal horn sensitization. This process results in persistence of pain (Portenoy and Lesage 1999).
Typically, interventional procedures of cancer pain have an additive effect for other modalities for treatment aiming at pain control. Furthermore, interventional procedures reduce medications and their side effects. Interventional procedures in the form of the interruption of nerve conduction aiming at diminishing pain from the target area have been applied (Wong et al. 2007). Intercostal neurolysis is a quiet easy technique that lasts for 3 to 8 weeks. However, studies reported occurrence of neuritis and advised that neurolytic agents should be limited to those with a short life expectancy (Swarm et al. 2005).
Dorsal root ganglion (DRG) ablation or thoracic rhizotomy is another modality for chest wall pain due to tumor invasion or somatic and neural structures. It involves segmental or multi-segmental destruction of the dorsal sensory roots. Rhizotomy is either surgically done or achieved by chemical neurolysis or radiofrequency ablation. It is an effective method of pain control especially with refractory localized pain syndromes (Hogan et al. 1991).
Diagnostic block with local anesthetic is initially applied prior to a planned neurolytic block to predict the likely outcome (Silvestri et al. 2002). Paravertebral blocks can be used in case of chest pain (Schneider et al. 1993).
Radiofrequency ablation is attained by the passage of low-energy, high-frequency alternating current (100,000–500,000 Hz) that causes oscillations of tissue ions. This oscillation results in heating of charged macromolecules, especially proteins (Organ 1976-1977). RF heating to 45 °C causes many cells to die rapidly. Neuroablation targets either the dorsal root ganglion (DRG) or a peripheral nerve. Above 55 °C, there is an indiscriminate destruction of both small- and large-diameter myelinated fibers. Histologically, there are focal necrosis, hemorrhages, extensive edema, and features of Wallerian degeneration (Smith et al. 1981).
The mode of action of RF was initially attributed to the thermocoagulation of nerve fibers. However, contradictory observations as transient sensory loss in the associated dermatome, whereas the pain relief may last for longer periods suggest that temperature is not the only mechanism responsible for the decrease in pain transmission (Racz and Ruiz-Lopez 2006).
The use of RF for the management of neuropathic pain is controversial for the fear of development of neuritis and deafferentation pain. Consequently, RF ablation could be only applied in somatic pain (De Louw et al. 2001).
The aim of this study is to compare the reduction in the narcotic requirement after thoracic rhizotomy versus thoracic paravertebral nerve radiofrequency in thoracic cancer pain management. The secondary outcome was the degree of improvement in daily activity.
Methods
This study was approved by the ethical committee. All patients were asked for a signed and informed consent after declaration of the technique and its possible benefits, risks, and side effects while for patients under 21 years old, an informed consent from their guardians was signed. We enrolled 30 patients with somatic chest pain due to underlying intra-thoracic malignancy. The inclusion criteria were age 18 years to 60 years, no interspinal extension of the tumor that was confirmed by MRI prior to the intervention, duration of pain was more than 3 months, and visual analogue scale (VAS) was more than 5 on 0–10 scale despite medical treatment or intolerability to medical treatment. Preoperative exclusion criteria were patient refusal and lack of understanding by the patient of the purpose of the study, coagulopathy, i.e., INR > 1.4 or platelet count < 80000 or local infection. Intraoperative exclusion criteria were failure either to localize or to get the anterior epidural space or the paravertebral space by image guidance and dye confirmation.
The preoperative evaluation included physical examination. Patients underwent complete blood count and coagulation profile. The primary outcome variable was the incidence of more than 50% reduction in the narcotic requirement after intervention at two assessment intervals 6 h after the procedure and 4 weeks later. The secondary outcome was improved daily activity as described by the patient to be improved or not after 4 weeks.
A standardized protocol was used. It included standard monitoring (ECG, non-invasive arterial pressure, pulse oximetry). All patients fulfilling the inclusion criteria got a diagnostic block with 5 ml, 0.25% bupivacaine thoracic paravertebral nerve block for each affected level. The affected dermatome determined the level of the nerve block (NB) (Uchida 2009).
All patients were put in prone position, and in both groups, we got anteroposterior view to determine the intended levels for injection and then we got to an oblique view about 10 to 15° to the contralateral side.
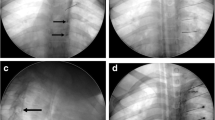
Then, in the dorsal root ganglia block group, we intended the foramen just below the pedicle (Fig. 1a), and then, the needle was introduced in a gun barrel fashion (Fig. 1b) after that we confirmed the position of the needle in a lateral view (Fig. 1c) after that we injected contrast to confirmed delineation of the contrast at the anterior epidural space (Fig. 1d, e).
While in the paravertebral nerve block group after turning to the oblique view about 10 to 15° to the contralateral side, we entered just lateral to the vertebral body, the needle hit the lateral side of vertebral body, it rotated laterally, and then, the position was confirmed in lateral position by injecting contrast and saw its spread within the paravertebral space (Fig. 2a).
Following the diagnostic testing, patients were randomized by a computer-generated numbers’ technique into two groups. Group 1 got dorsal root ganglia ablation at 67 °C for 60 s. The generator (PMG-115- TD, V2.0A, Baylis Medical) with a 10-cm electrode and a 5-mm active tip had been used after sensory stimulation between 0.2 and 0.7 V while group 2 got thoracic paravertebral nerve (TPN) ablation with the same protocol. Before ablation, 1.5 ml of 2% mepivacaine and 2 mg of betamethasone were administered (Cohen et al. 2004).
Measured parameters
The two groups were compared regarding the reduction of narcotics, activity improvement, sensory loss, burning sensation, and back pain.
Sample size calculation
A previous study (Cohen et al. 2006) reported more than 50% pain relief in 61.5% of patients treated by dorsal root ganglia pulsed radiofrequency compared to 21.4% of those treated with radiofrequency of the intercostal nerves. Based on these results, a sample size of 15 cases in each group will be satisfactory to elicit the difference at an alpha level of 0.05 and a power of the test of 95%.
Statistical methods
IBM SPSS Advanced Statistics Version 20.0 was used for data analysis using (SPSS Inc., Chicago, IL). Normally distributed numerical data are presented as mean ± SD, and differences between groups were compared using the independent Student’s t test, categorical variables were analyzed using the χ2 test or Fisher’s exact test and are presented as number (%). All p values are two-sided. p < 0.05 is considered statistically significant.
Results
The study was conducted in the period from 28th of September 2014 to 30th of June 2015 at the National Cancer Institute and included thirty patients with thoracic cancer pain. Patients fulfilling inclusion criteria were randomized to receive RF ablation of DRG (group 1, n = 15) or of TPN (group 2, n = 15) to treat somatic chest pain. Patients included (8 and 9) males and (7 and 6) females in group 1 and group 2, respectively, with the mean age 43.866 ± 10.58 and 44.8 ± 9.45 years. No significant difference (p value = 1.000) in the type of patients between the two groups regarding previous treatment and procedures they got (Table 1). Table 2 shows the intended levels for ablation as indicated by the diagnostic intercostal block prior to intervention. Table 3 shows the actually performed thoracic segments.
Six hours postoperatively, RF ablation of DRG resulted in reduction of required dose of narcotics in 12 patients (80%) compared to 6 patients (40%) treated with RF ablation of TPN (p value = 0.025). After 4 weeks, reduction was recorded in 80.0% compared to 33.3% of patients in the two groups, respectively (p value = 0.010). Patients’ activity (assessed by yes or no scale) improved in 11 patients (73.3%) in the DRG group compared to 5 patients (33.3%) in the TPN group (p value = 0.028). The two groups were comparable in frequency of sensory loss (12 in groups 1 and 11 in group 2) (p value = 1.000), burning sensation (3 in groups 1 and 8 in group 2) (p value = 0.128), and allodynia (4 in groups 1 and 9 in group 2) (p value = 0.139).
Discussion
Considering improved cancer survival rates, the recognition and treatment of malignant chest pain has become a major challenge. There are no randomized clinical trials compared with radiofrequency lesioning of the dorsal root ganglion and thoracic paravertebral nerve. Our study aims at comparing the outcome of treatment with radiofrequency (RF) of the dorsal root ganglia (DRG) (Fig. 1a–e) versus RF of the thoracic paravertebral nerves (TPN) (Fig. 2a, b).
Thoracic DRG targeting is much more challenging than the paravertebral thoracic nerve as 3 patients in the DRG group (Table 3) got less number of level than intended. In addition, the transforaminal approach carries the risk of injury to the single radicular artery to higher thoracic levels. It may also lead to injury of the unpaired artery of Adamkiewicz which exclusively supplies the spinal cord (White and El-Khoury 2002), adding to consideration the finding of Hamann et al. (2006) who studied the delivery of pulsed RF to the L4 anterior primary ramus just lateral to the intervertebral foramen in rats. Fourteen days later, there was an upregulation in activating transcription factor 3, indicating cellular stress in DRG cell bodies. Consequently, this finding raised the question if targeting the TPN may result in comparable results to lesioning the DRG without the inherited risk of the later. Moreover, the contradictory observations of short-lived with long lasting pain relief suggest that pain relief is not temperature-dependent (Racz and Ruiz-Lopez 2006).
In our study, there was a reduction of narcotic requirement (in 80% of patients after 6 h and 4 weeks). These findings are comparable to that of Stolker et al. (1994), and they evaluated 45 patients with thoracic radicular pain treated with RF. There was a significant reduction of pain in more than 70% of patients 13 to 46 months after treatment. Van Kleff and Spans (1995) performed the same study and found that 52% had a significant pain reduction for 9–39 months. The effect was smaller when several segments were targeted. No studies compared RF with pulsed radiofrequency (PRF). Only one retrospective study compared pulsed radiofrequency PRF of the intercostal nerve with DRG. DRG PRF resulted in more success, and the effect of RF is better and lasts longer (Cohen et al. 2006).
Cohen et al. (2006) compared pharmacotherapy, pulsed RF of the intercostal nerves (ICN), and pulsed RF of the dorsal root ganglia (DRG) in chronic postsurgical thoracic pain (CPTP). It is a retrospective study, and the investigators concluded that pulsed RF of the DRG was associated with the best pain relief. They recommended the performance of prospective studies to confirm these results and identify the best candidates for this treatment (Cohen et al. 2006).
Interestingly, patients in the DRG treatment group showed that they experienced symptoms for a longer duration of time than patients in the other two groups. However, previous studies evaluating procedural interventions for pain control have shown the duration of symptoms to correlate negatively with success rates (Quigley et al. 1998; Perez et al. 2003; Tanaka et al. 2002). In our study, burning sensation and allodynia had a higher incidence in the thoracic nerve intervention group with no statistical significance. This difference with our finding can be explained by different implied techniques as RF is different from PRF in both temperature and type of energy used. Moreover, RF has been proved to have a different effect in terms of cellular structure in animal trials.
There are several limitations of this study of Steven et al. First, this was a retrospective study. The patients were not randomized. Second, outcomes are reported in terms of percent of pain relief. In clinical practice, a patient’s reported percent reduction in pain does not always correspond precisely with their change in numerical pain rating.
Animal studies provided conflicting data about the effect of different types of radiofrequency with no reliable provision regarding mechanism of action. In a study by Higuchi et al. (2002), the investigators exposed rat DRG to continuous RF and pulsed RF. In both groups, a temperature of 38 °C for 2 min was targeted. When the animals were humanely killed 3 h after lesioning, the authors found increased c-Fos expression in the dorsal horn after pulsed, but not continuous RF application. Apparently, it seems mode-dependent rather than temperature effect. On the contrary, Van Zundert et al. (2005) performed continuous RF at 67 °C for 1 min, or pulsed RF for either 2 min or 8 min on 19 rats who underwent cervical laminectomies. The authors of this study found increased numbers of c-Fos immunoreactive cells in the dorsal horn of subject of the three groups, with no differences noted between groups.
These conflicting data suggests the need for a clinical trial that brings the radiofrequency technology out of the theory to a more definite action in terms of indication and effect.
There have been no prospective controlled trials on terminal radiofrequency (TRF) of the thoracic DRG. Stolker et al. conducted a prospective uncontrolled trial. They investigated the effect of RF on the thoracic DRG at 67 °C, and they treated 45 patients afflicted with thoracic segmental pain. They reported pain relief at 2 months up to 13 to 46 months (Stolker et al. 1994).
In our study design, it seemed unreasonable to assess the long-term response because of the nature of cancer pain with entitled plasticity and continuous change in type and source of pain.
Our study involved only pain of somatic pain and excluded neuropathic pain. The potential hazard of neural destruction caused by RF might intensify symptoms by inducing deafferentation pain.
It is based on Van Kleef and Spans (1995) suggestion that TRF-DRG was not suitable for neuropathic pain syndromes with sensory loss and should be only reserved for purely nociceptive pain syndromes.
The therapeutic effect of TRF is achieved by a partial nerve lesion to nociceptive afferents (Bogduk 2006). On the other hand, minor nerve injury can sometimes produce devastating pain, whereas modest or diffuse deafferentation does not (Moore et al. 2002). Clearly, the definitive ablation at DRG, at the current study, resulted in lower incidence, statistically insignificant, of allodynia and burning sensation.
The provision of adding steroid can be explained by the fact that pro-inflammatory cytokines secreted at the site of nerve injury are involved in the development and maintenance of central sensitization and neuropathic pain (Romundstad and andStubhaug 2007). Consequently, this explained the low incidence of burning pain in our candidates. These findings go with Van Kleef and Spans (1995) observations. The investigators evaluated the effectiveness of TRF-DRG (67 °C, 60 s) in patients presenting with chronic thoracic pain and reported significantly better short-term and long-term pain relief. However, in their report, 14 (33%) out of 43 patients experienced a mild burning pain in the treated dermatome for some days following treatment.
Patient activity is determined by a direct question that is used to assess patient satisfaction and change in function. It is not validated, and future studies should include validated outcome measures assessing not only pain, but the mood, function, and quality of life.
Finally, taken in context, our findings suggest that RF of the DRG is superior to RF of the TPN. However, given the inherent risk of performing interventional thoracic procedures, we cannot recommend it as a first-line treatment based on the results of one study. We believe it should be reserved for those patients refractory to pharmacotherapy and should be implemented with rehabilitation and psychological counseling, as indicated.
Conclusion
RF ablation of DRG is superior to RF ablation of TPN in relieving thoracic pain with more improvement of patients’ activity and similar adverse outcomes.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on a reasonable request.
Abbreviations
- RF:
-
Radiofrequency
- DRG:
-
Dorsal root ganglia
- TPN:
-
Thoracic paravertebral nerve
- MRI:
-
Magnetic resonance imaging
- INR:
-
International normalizing ratio
References
Bogduk N (2006) Pulsed radiofrequency. Pain Med 7(5):396–407
Caraceni A, Portenoy RK (1999) An international survey of cancer pain characteristics and syndromes. IASP Task Force on Cancer Pain. Pain. 82(32):263–274
Cohen SP, Larkin TM, Chang AS, Stojanovic MP (2004) The causes of false-positive medial branch (facet joint) blocks in soldiers and retirees. Mil Med 169:781–786
Cohen SP, Sireci A, Wu CL, Larkin TM, Williams KA, Hurley RW (2006) Pulsed radiofrequency of the dorsal root ganglia is superior to pharmacotherapy or pulsed radiofrequency of the intercostal nerves in the treatment of chronic postsurgical thoracic pain. Pain Phys 9:227–236
De Louw AJ, Vles HS, Freling G, Herpers MJ, Arends JW, Kleef M (2001) The morphological effects of a radio frequency lesion adjacent to the dorsal rootganglion (RF-DRG)-an experimental study in the goat. Eur J Pain 5(2):169–174
Hamann W, Abou-Sherif S, Thompson S, Hall S (2006) Pulsed radiofrequency applied to dorsal root ganglia causes a selective increase in ATF3 in small neurons. Eur J Pain 10:171–176
Higuchi Y, Nashold BS, Sluijter M, Cosman E, Pearlstein RD (2002) Exposure of the dorsal root ganglion in rats to pulsed radiofrequency currents activates dorsal dorsal horn lamina I and II neurons. Neurosurgery 50:850–856
Hogan Q, Haddox JD, Abram S, Weissman D, Taylor ML, Janjan N (1991) Epidural opiates and local anesthetics for the management of cancer pain. Pain. 46(3):271–279
Laird BJ, Scott AC, Colvin LA, McKeon AL, Murray GD, Fearon KC, Fallon MT (2011a) Pain, depression, and fatigue as a symptom cluster in advanced cancer. J Pain Symptom Manag 42(1):1–11
Laird BJ, Walley J, Murray GD, Clausen E, Colvin LA, Fallon MT (2011b) Characterization of cancer-induced bone pain: an exploratory study. Support Care Cancer 19(9):1393–1401
Moore KA, Kohno T, Karchewski LA, Scholz J, Baba H, Woolf CJ (2002) Partial peripheral nerve injury promotes a selective loss of GABAergic inhibition in the superficial dorsal horn of the spinal cord. J Neurosci 22(15):6724–6731
Organ LW (1976-1977) Electrophysiologic principles of radiofrequency lesion making. Appl Neurophysiol 39(2):69–76
Perez RS, Zuurmond WW, Bezemer PD, Kuik DJ, van Loenen AC, de Lange JJ, Zuidhof AJ (2003) The treatment of complex regional pain syndrome type I with free radical scavengers: a randomized controlled study. Pain 102:297–307
Portenoy RK, Lesage P (1999) Management of cancer pain. Lancet. 353(9165):1695–1700
Quigley MR, Bost J, Maroon JC, Elrifai A, Panahandeh M (1998) Outcome after microdiscectomy: results of a prospective single institutional study. Surg Neurol 49:263–267
Racz GB, Ruiz-Lopez R (2006) Radiofrequency procedures. Pain Pract 6(1):46–50
Romundstad L, andStubhaug A (2007) Glucocorticoids for acute and persistent postoperative neuropathic pain: what is the evidence? Anesthesiology. 107(3):371–373
Schneider RF, Villamena PC, Harvey J, Surick BG, Surick IW, Beattie EJ (1993) Lack of efficacy of intrapleural bupivacaine for postoperative analgesia following thoracotomy. Chest. 103(2):414–416
Siegel R, Ma J, Zou Z, Jemal A (2014) Cancer statistics. CA Cancer J Clin 64:9–29
Silvestri GA, Sherman C, Williams T, Leong SS, Flume P, Turrisi A (2002) Caring for the dying patient with lung cancer. Chest. 122(3):1028–1036
Smith HP, McWhorter JM, Challa VR (1981) Radiofrequency neurolysis in a clinical model neuropathological correlation. J Neurosurg 55(2):246–253
Stolker RJ, Vervest Ac M, Groen GJ (1994) The treatment of chronic thoracic segmental pain by radiofrequency percutaneons partial rhizotomy. J Neuro Surg 80:986–992
Stute P, Soukup J, Menzel M, Sabatowski R, Grond S (2003) Analysis and treatment of different types of neuropathic cancer pain. J Pain Symptom Manag 26(6):1123–1131
Swarm RA, Karanikolas M, Cousins MJ (2005) Anaesthetic techniques for pain control. In: Doyle DD, Hanks G, Cherny NI, Calman SK (eds) Oxford textbook of palliativemedicine, 3rd edn. Oxford University Press, NewYork, pp 378–396
Tanaka N, Sakahashi H, Sato E, Hirose K, Ishima T, Ishii S (2002) Intra-articular injection of high molecular weight hyaluronan after arthrocentesis as treatment for rheumatoid knees with joint effusion. Rheumatol Int 22:151–154
Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF, Billings JA, Lynch TJ (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363(8):733–742
Uchida K (2009) Radiofrequency treatment of the thoracic paravertebral nerve combined with glucocorticoid for refractory neuropathic pain following breast cancer surgery. Pain Phys 12(4):E277–E283
Van Kleef M, Spans F (1995) The effects of producing a radiofrequency lesion adjacent to the dorsal root ganglion in patients with thoracic segmental pain by radiofrequency percutaneous partial rhizotomy. Clin J Pain 11:325–332
Van Zundert J, de Louw AJ, Joosten EA, Kessels AG, Honig W, Dederen PJ, Veening JG, Vles JS, van Kleef M (2005) Pulsed and continuous radiofrequency current adjacent to the cervical dorsal root ganglion of the rat induces late cellular activity in the dorsal horn. Anesthesiology 102:125–131
White ML, El-Khoury GY (2002) Neurovascular injuries of the spinal cord. Eur J Radiol 42:117–126
Wong FC, Lee TW, Yuen KK, Lo SH, Sze WK, Tung SY (2007) Intercostal nerve blockade for cancer pain: effectiveness and selection of patients. Hong Kong Med J 13(4):266–270
Acknowledgements
Not applicable
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
Both the authors MA Elramely and W. Abdelmoneim participated in case selection, editing, and performing thoracic radiofrequency rhizotomy and thoracic paravertebral nerve radiofrequency techniques. MA Elramely collected the data as hemodynamics, pain assessment, and complication incidence. W. Abdelmoneim achieved statistics. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board (IRB) approval number is 201001415034.2 on July 7, 2015, and the clinical trial registration number is PACTR201511001257724. A written consent from the participants was taken individually. All patients were asked for a signed and informed consent after declaration of the technique and its possible benefits, risks, and side effects while for patients under 21 years old, an informed consent from their guardians was signed.
Consent for publication
Consent for publication was obtained from the participants.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elramely, M.A., Abdelwahab, W.A. Thoracic rhizotomy versus thoracic paravertebral nerve radiofrequency in thoracic cancer pain. Ain-Shams J Anesthesiol 13, 11 (2021). https://doi.org/10.1186/s42077-020-00125-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-020-00125-3