Abstract
Background
Acute pain in post joint replacement surgeries is common, which makes the management of acute pain following joint replacement surgeries to be very important. Thus, this study was conducted to evaluate acute pain management of post TKR surgeries.
Results
Patients with negative pain management index (PMI) scores were classified as receiving inadequate analgesic treatment for their pain. Zero PMI was the most frequent score among the others with 195 (80.6%). The rest were − 1 (11 (4.5%)), 1 (27 (11.2%)), and 2 (9 (3.7%)), respectively. Only 4.5% (11/242) patients have negative PMI score, which could be considered as inadequate pain management in which these patients received inadequate analgesic treatment.
Conclusion
Acute pain management in post-TKR surgeries in both medical centers achieved an acceptable level, and majority of patients received an adequate analgesia in post-TKR surgeries.
Similar content being viewed by others
Background
Major orthopedic surgeries are divided into 3 major surgeries: total hip replacement (THR), TKR, and hip fracture surgeries (HFS). Acute pain post of these surgeries is common (Wylde et al. 2011). Managing acute pain following joint replacement surgeries is very important due to the following reasons: First, studies have shown that poor control of acute pain after TKR is closely correlated with the development of chronic pain, which illustrates the importance of a good control of acute pain after TKR (McCartney and Nelligan 2014). Second, joint replacement is one of the most widely used elective surgical procedures in the Middle East (Al-Taiar et al. 2013); in 1994, the number of TKR surgeries in Saudi Arabia was more than 12 procedures per year (Ahlberg 1994). The number of THR and TKR performed worldwide and in Saudi Arabia continued to increase, and the patients receiving these procedures seemed to be sicker than that in the past (McMinn et al. 2012). Third, joint replacement surgeries are primarily performed to relieve chronic joint pain (Hawker et al. 1998), and yet, some patients tend to experience chronic pain following joint replacement surgery, which refers to the failure of surgery for these patients. This therefore suggests that the use of effective acute pain management is crucial. The aim of this study is to evaluate acute pain management in post-TKR surgeries.
Method
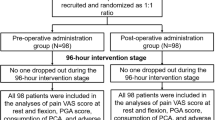
This is a prospective cohort study that was done in two medical centers in Saudi Arabia. This study has been approved by the Institutional Review Board (IRB) in both centers; consent forms were stacked to the data collection sheet, and all participants were asked to sign it after being informed about the study details and before starting the data collection process. All patients who underwent primary TKR surgery in the included medical centers aged 18 years old and above between the periods of October 2018 till July 2019 were involved in this study. In addition, prospective data collection sheet was used, which contained the numeric rating scale (NRS) consisting 11 numbers from 0 to 10 with 0 representing no pain and 10 representing the worst pain. All participants were instructed to select a number between 0 and 10 that best describes their current pain after 24 h of TKR surgery (this allows for the anesthetic effect to be cleared from the patients’ bodies). This scale was chosen as it is the most commonly used scale in clinical practice (Nair and Diwan 2020). Pain scores were then classified into four categories: no pain = 0, mild pain = 1 up to 4, moderate pain = 5 and 6, severe pain = 7 up to 10. On the other hand, analgesics were categorized into 4 groups (analgesic score): if no analgesia is prescribed, it is assigned as 0, and if non-opioid analgesics are prescribed (acetaminophen 1 g intravenous), it is denoted as 1; if weak opioid analgesics are prescribed (tramadol I.V or tablets), it is denoted as 2, whereas it is denoted as 3 if strong opioid analgesics are prescribed (epidural fentanyl). Then, for each patient, the PMI was calculated by subtracting the pain score from the analgesic score where a negative PMI is considered as inadequate pain management by the prescriber (McNeill et al. 2001). Pain management method in this study depended on the use of conventional procedure for acute pain management after total joint replacement including a great dependence on opioid, oral or intravenous (IV), and patient-controlled analgesia (PCA) with IV opioid or epidural infusion (Prasad 2020). In the current study, epidural fentanyl was the most common used opioid analgesic.
Sample size calculations
According to the Health Affairs of Ministry of National Guard in the Kingdom of Saudi Arabia 2018, about 5000 joint replacement procedures have been performed over the last 10 years with an average of 500 joint replacements annually. Consequently, 500 represent the target population of this study; so, the sample size according to Modified Cochran Formula at 95% confidence interval and 0.05 significance level was 217 as the minimum sample size.
Data analysis
The data was analyzed using SPSS (version 20) at a significance level of 0.05. Descriptive analysis was used to describe the sample of population. Chi-square test and ANOVA were used to determine the presence of any significant differences between various groups.
Results
A total of 242 patients participated in this study. Patients’ demographic characteristics are shown in Table 1. It was clear that the mean age for all participants was 65.86 ± 8.67 years old, and most of them were females 137 (56.6%). Body mass index (BMI) mean of the study population was 32.46 ± 5.51. Moreover, 70.2% of the patients were reported to suffer severe pain with only 8.3% of them having mild pain.
PMI was obtained by subtracting pain scores from the types of analgesia. Frequency analysis was used to get the counts of negative scores of PMI. Table 2 shows the describing PMI scoring among the participants in this study. Patients with negative PMI scores were classified as receiving inadequate analgesic treatment for their pain. Zero was the most common frequency scoring among the others with 195 (80.6%). The rest were − 1 (11 (4.5%)), 1 (27 (11.2%)), and 2 (9 (3.7%)), respectively. Only 4.5% (11/242) of the patients have negative PMI that were considered having inadequate pain management, inadequate analgesic treatment, underestimated for their pain level, and were accordingly undertreated. Cumulatively, 14.9% (36/242) were overestimated for their pain levels and were accordingly overtreated. The data are presented graphically in Fig. 1.
Table 3 describes the PMI among analgesic intake with pain score. Inadequate analgesia pain management among analgesic intake was also described in the same table. However, the most negative PMI was indicated in weak opioids with nine patients who have received inadequate analgesia as weak opioid, followed by non-opioids with two patients who received non-opioid analgesia.
Discussion
TKR requires extensive bone dissection and manipulation of soft tissue; hence, patients may have severe pain in the early postoperative period that requires an effective pain management to improve patients’ recovery (Armanious et al. 2020). The evidence available on post-TKR pain management is inadequate to develop realistic, accurate, and routine protocols for pain management (Chang and Cho 2012). In the current study, around 70% of the patients have reported severe pain in day 1 of post-TKR, which is higher than the reported percentage in literature. The percentage of patients with severe pain after TKR as reported by a recent review article was 58% during day 1 of post-operation and 45% in day 3 of post-operation (Grosu et al. 2014). Up to the author’s knowledge, this study is the first to use PMI for assessing acute pain management of post-TKR. According to Mitera et al. (2010a), PMI is obtained by subtracting pain scores from the types of analgesia. The negative scores of PMI among the participants in this study showed that the patients received inadequate analgesic treatment for their pain. Inadequate pain management was seen in 4.5% (11/242) of the patients. Having a negative PMI could be considered as inadequate pain management, and these patients received inadequate analgesic treatment, underestimated for their pain level (Singh et al. 2016) and accordingly undertreated. On the other hand, some studies claimed that a negative PMI does not necessarily indicate inadequate pain management, but rather due to pain interference in these patients (Sakakibara et al. 2018).
By looking at Table 3, it was apparent that most negative PMI was indicated in weak opioids with nine patients reported having severe pain and received weak opioid instead of strong opioid, while another two patients reported moderate pain and received a non-opioid analgesia. Zero PMI means that the pain management is adequate, not over or undertreated (Parvizi and Bloomfield 2013). The most frequent PMI score among the others was zero score with 80.6% of patients (195/242), meaning that majority of patients were given the appropriate analgesia according to the level of the reported pain. On the other hand, 14.9% (36/242) were overestimated for their pain levels and accordingly were overtreated; nine of these patients were reported having mild pain and were prescribed with a strong opioid, which showed the PMI of 2, while another 20 patients with the PMI score of 1 were reported with moderate pain and were prescribed a strong opioid. The remaining seven patients were prescribed with weak opioid since they were reported having mild pain. Another study done to assess pain management in cancer patients using PMI indicated that 25.8% from one thousand patients have a negative PMI, which was explained as inadequate pain management due to undertreatment (Mitera et al. 2010b). In this study, a negative PMI was seen in only 4.5% (11/242), which is a good indication for adequate acute pain management of post TKR in the involved medical centers.
Conclusion
This is a prospective observational study that is aimed to evaluate acute pain management of post-TKR surgeries in two medical centers. Acute pain management post-TKR surgeries in both medical centers achieved an acceptable level, and majority of patients have received an adequate analgesia in post TKR surgeries.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TKR:
-
Total knee replacement
- NRS:
-
Numeric Rating Scale
- PMI:
-
Pain management index
- THR:
-
Total hip replacement
- HFS:
-
Hip fracture surgeries
- PCA:
-
Patient-controlled analgesia
- BMI:
-
Body mass index
- PSMMC:
-
Prince Sultan Military Medical City
- KAAUH:
-
King Abd Allah University Hospital
- PNU:
-
Princess Noura University
- IRB:
-
Institutional Review Board
References
Ahlberg A (1994) Knee joint replacement in Saudi Arabia-present and future. Ann Saudi Med 14:281–281. https://doi.org/10.5144/0256-4947.1994.281
Al-Taiar A, Al-Sabah R, Elsalawy E, Shehab D, Al-Mahmoud S (2013) Attitudes to knee osteoarthritis and total knee replacement in Arab women: a qualitative study. BMC Res Notes 6(1):406. https://doi.org/10.1186/1756-0500-6-406
Armanious SH, Botros JM, Ganzoury IME, Abdelhameed GA (2020) Adductor canal block versus femoral nerve block in unicompartmental knee arthroplasty: a randomized, double blind, prospective, comparative study. Ain-Shams J Anesthesiol 12(1):1–8. https://doi.org/10.1186/s42077-020-00077-8
Chang CB, Cho WS (2012) Pain management protocols, peri-operative pain and patient satisfaction after total knee replacement: a multicentre study. J Bone Joint Surg Br Vol 94(11):1511–1516. https://doi.org/10.1302/0301-620X.94B11.29165
Grosu I, Lavand’homme P, Thienpont E (2014) Pain after knee arthroplasty: an unresolved issue. Knee Surg Sports Traumatol Arthrosc 22(8):1744–1758. https://doi.org/10.1007/s00167-013-2750-2
Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R et al (1998) Health-related quality of life after knee replacement. Results of the knee replacement patient outcomes research team study. J Boint Joint Surg Am 80(2):163–173 URL: https://journals.lww.com/jbjsjournal/Abstract/1998/02000/Health_Related_Quality_of_Life_after_Knee.3.aspx
McCartney CJ, Nelligan K (2014) Postoperative pain management after total knee arthroplasty in elderly patients: treatment options. Drugs Aging 31(2):83–91. https://doi.org/10.1007/s40266-013-0148-y
McMinn DJW, Snell KIE, Daniel J, Treacy RBC, Pynsent PB, Riley RD (2012) Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ 344:e3319. https://doi.org/10.1136/bmj.e3319
McNeill JA, Sherwood GD, Starck PL, Nieto B (2001) Pain management outcomes for hospitalized Hispanic patients. Pain Manage Nurs 2(1):25–36. https://doi.org/10.1053/jpmn.2001.22039
Mitera G, Fairchild A, DeAngelis C, Emmenegger U, Zurawel-Balaura L, Zhang L et al (2010a) A multicenter assessment of the adequacy of cancer pain treatment using the pain management index. J Palliat Med 13(5):589–593. https://doi.org/10.1089/jpm.2009.0342
Mitera G, Zeiadin N, Kirou-Mauro A, DeAngelis C, Wong J, Sanjeevan T et al (2010b) Retrospective assessment of cancer pain management in an outpatient palliative radiotherapy clinic using the Pain Management Index. J Pain Symptom Manag 39(2):259–267. https://doi.org/10.1016/j.jpainsymman.2009.07.005
Nair AS, Diwan S (2020) Pain scores and statistical analysis—the conundrum. Ain-Shams J Anesthesiol 12(1):1–2. https://doi.org/10.1186/s42077-020-00085-8
Parvizi J, Bloomfield MR (2013) Multimodal pain management in orthopedics: implications for joint arthroplasty surgery. Orthopedics 36(2):7–14. https://doi.org/10.3928/01477447-20130122-51
Prasad GK (2020) Post-operative analgesia techniques after total knee arthroplasty: a narrative review. Saudi J Anaesth 14(1):85. https://doi.org/10.4103/sja.SJA_494_19
Sakakibara N, Higashi T, Yamashita I, Yoshimoto T, Matoba M (2018) Negative pain management index scores do not necessarily indicate inadequate pain management: a cross-sectional study. BMC Palliat Care 17(1):1–7. https://doi.org/10.1186/s12904-018-0355-8
Singh H, Banipal RPS, Singh B (2016) Assessment of adequacy of pain management and analgesic use in patients with advanced cancer using the brief pain inventory and pain management index calculation. J Glob Oncol 3(3):235–241. https://doi.org/10.1200/JGO.2016.004663
Wylde V, Rooker J, Halliday L, Blom A (2011) Acute postoperative pain at rest after hip and knee arthroplasty: severity, sensory qualities and impact on sleep. Orthop Traumatol Surg Res 97(2):139–144. https://doi.org/10.1016/j.otsr.2010.12.003
Acknowledgements
The authors would like to acknowledge gratefully all surgeons at the surgical departments in both medical centers. The authors also would like to acknowledge Dr. Ameerah Shabbab Al-Harthi, a senior physical therapist at Prince Sultan Military Medical City, for her guidance and help. A great appreciation goes out to all the inpatients’ nurses in both medical centers, especially, the inpatients’ nurses at building 5 (ward 2) and building 2 from level 3 till level 7 at Prince Sultan Military Medical City, for their cooperation and guidance through the journey of this research.
Funding
This research did not receive any specific grant from any funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All listed authors meet the International Committee of Medical Journal Editors criteria. We attest that all authors contributed significantly to the creation of this manuscript. ‘MA’ and ‘SAS’ have contributed in the idea creation for this research; they have designed the methodology. ‘MA’ wrote the manuscript after the analysis, and study findings have been discussed by all contributing authors. Moreover, all authors have been involved in revising this manuscript critically. ‘AA’ and ‘MFA’ have been involved in the implementation of this research and adjusting the methodology to suit the relevant guidelines and regulation. ‘MA,’ ‘AA,’ and ‘MFA’ have been involved in data collection and follow up records for all patients through the study period. Finally, all authors have reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the Institutional Review Board (IRB) in both centers; the first IRB was obtained from Research Ethics Committee, Scientific Research Center, Prince Sultan Military Medical City, Riyadh, Kingdom of Saudi Arabia-11149 with a reference number (HP-01-R-079). Meanwhile, the second IRB was obtained from Institutional Review Board (IRB) 2018 of Princess Nourah bin Abdulrahman University, Riyadh, Kingdom of Saudi Arabia with a reference number (H-01-R-059). Consent forms were stacked to the data collection sheet, and all participants were asked to sign it after being informed about the study details and before starting the data collection process.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alameri, M.A., Sulaiman, S.A.b.S., Moh’d Talaat Ashour, A. et al. Assessment for acute pain management in post-total knee replacement (TKR): a prospective cohort study in two Saudi Arabian medical centers. Ain-Shams J Anesthesiol 12, 63 (2020). https://doi.org/10.1186/s42077-020-00111-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-020-00111-9