Abstract
Background
Rosai-Dorfman disease (RDD) is a rare but well-defined, histiocytic proliferative disorder with massive lymphadenopathy.
Case presentation
Herein we present the case of a 22-month-old girl with abdominal, neutrophilia, anemia, ascites, hepatosplenomegaly and fever. There were multiple enlarged mesenteric and para-aortic lymph nodes on abdominal ultrasonography and computer tomography scan. Microscopic examination of mesenteric lymph nodes showed dilation of the lymph sinuses occupied by lymphocytes, plasma cells, and many histiocytes. These histiocytes showed emperipolesis within their cytoplasm. With the diagnosis of RDD, prednisolone was started and good response was seen. However, splenomegaly and pancytopenia presented at follow up, and, after several hospital admissions, she died of sepsis.
Conclusions
RDD should be considered in the differential diagnosis of pediatric lymphadenomegaly. Although most patients experience favorable prognosis, some fatalities occur due to progression and dissemination of the disease.
Similar content being viewed by others
Background
Rosai-Dorfman disease (RDD), described by Rosai and Dorfman (Rosai and Dorfman 1969) in 1969, also known as Rosai-Dorfman-Destombes disease and sinus histiocytosis with massive lymphadenopathy, is a rare cause of adenopathy, which is more prevalent in children and young adults. It is a non-Langerhans cell histiocytosis which now belongs to the R group of the 2016 revised histiocytosis classification (Abla et al. 2018).
Clinical manifestations are due to accumulation of activated histiocytes within the affected tissues. Although in its classic form RDD usually presents with massive bilateral cervical lymphadenopathy (Mantilla et al. 2016), it is frequently multifocal and evaluation of other areas should be considered. The involved gastrointestinal tract in RDD is the least common extranodal involvements (Gaitonde 2007) which makes this case worth reporting.
Here, we present a 22-month-old girl who was referred to our hospital due to abdominal distention.
Case presentation
A 22-month-old girl, with unremarkable past and family medical history, referred to the hospital with abdominal distention and fever starting about 2 months prior to admission. Body temperature was 38.5 degrees centigrade with normal respiratory rate. In the examination of the abdomen, a mass was palpated just below her liver. There was splenomegaly in examination. Lung and Head/Neck examination was normal. Lab data showed leukocytosis (WBC: 34800 /mm3), hemoglobin 8.1 mg/dl (normochromic normocytic anemia), platelet 308,000 /mm3. Differential count showed neutrophilia (neutrophil 60%, lymphocyte 28%, eosinophil 7% and monocyte 5%). Biochemical tests showed LDH 701 U/l, creatinine 0.6 mg/dl, alkaline phosphatase 1110 U/l, GGT 201 U/l, AST 23 U/l, ALT 16 U/l, total protein 7.4 mg/dl and albumin 3.7 mg/dl. C-reactive protein and ESR were high (CRP 115 mg/l and ESR 96 mm/hr). Blood and urine cultures were negative.
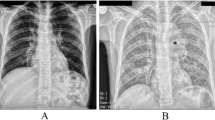
Abdominopelvic ultrasonography showed hepatosplenomegaly, severe ascites, and multiple enlarged mesenteric and para-aortic lymph nodes. CT scan of the abdomen showed multiple para-aortic lymphadenopathies forming conglomerate mass, as well as mesenteric lymphadenopathies up to 31 × 25 mm (Fig. 1). A few retro-crural lymph nodes were also seen up to 20 × 9 mm. With the impression of lymphoma, computed tomography (CT) scan-guided Tru-Cut biopsy was performed. Immunohistochemical profile showed extensive lymphoid and histiocytic infiltration with no definite evidence of lymphoma; complete excision of the lymph node for further evaluation was recommended.
The patient underwent exploratory laparotomy for lymph node biopsy. One large mesenteric lymph node was excised. During the surgery, approximately 600 mL of abdominal fluid was also drained. Cytologic examination showed neither malignant cell. Cell count of abdominal fluid showed about 2500 cells/mm3 with 50% neutrophils.
One abdominal lymph node measuring 1.5 × 1 × 1 cm was sent to the pathology lab. The cut sections showed homogenous solid creamy surface. Microscopic examination showed dilation of the lymph sinuses resulting in partial architectural effacement. The sinuses were occupied by the lymphocytes, plasma cells, and many histiocytes. These histiocytes had large vesicular nucleus and abundant lightly eosinophilic cytoplasm. Many of them had numerous intact lymphocytes (emperipolesis or lymphophagocytosis) within their cytoplasm (Fig. 2a-d). Immunohistochemistry was positive for CD68 and S100 in the histiocytes (Fig. 3a and b) and negative for CD1a. Other immunohistochemical markers were done (CD20, CD3, CD5, CD7, PAX-5, CD15, CD30 and Ki-67). Morphology and immunohistochemical profile showed extensive lymphoid and histiocytic infiltration with no definite evidence of lymphoma. The diagnosis of sinus histiocytosis, more probably RDD, was made.
a Microscopic section shows low power view of the lymph node with dilation of the sinuses occupied by the histiocytes and lymphocytes (hematoxylin and eosin stain, × 100). b Microscopic section shows the histiocytes with emperipolesis (arrow) (hematoxylin and eosin stain, × 400). c and d Arrows show emperipolesis and lymphophagocytosis (hematoxylin and eosin stain, × 1000)
She developed another episode of fever after the surgery. The differential diagnoses were post-surgery infection and fever as a manifestation of the disease; routine fever workups were requested. Blood culture showed the growth of Achromobacter xylosoxidans. When she was evaluated for other causes of lymphadenopathy, anti-cytomegalovirus antibody IgM was also detected. Polymerase chain reaction for CMV and EBV were performed on blood; CMV showed 2400 copies/ml of plasma and EBV was negative. rK39 strip test for leishmania was negative. Antibiotic therapy and gancyclovir were started for her. However, CMV infection presenting like this and explaining all her symptoms was unlikely.
To treat RDD, we administered prednisolone 40 mg/m2 and once weekly vinblastine for the patient and she initially responded quite well to it. The patient was discharged from the hospital. In her follow ups, all the lymph nodes and her liver had regressed in size. The leukocyte count became normal. However, her spleen, despite the initial good response, started to become larger.
She was admitted several times due to fever and neutropenia. Although neutropenia is an adverse effect of vinblastine, in this patient, it seemed that neutropenia was due to sequestration of the white blood cells in the spleen. The neutropenia did not resolve although we had discontinued the drug. The other reason which justifies this argument is that vinblastine results in isolated neutropenia; however our patient was suffering pancytopenia which refers to splenomegaly. Bone marrow aspiration and biopsy was normal.
In the last admission, she had pancytopenia. The spleen was so huge that it could be palpated up to near the pelvic brim. This time, she was evaluated for the autoimmune lymphoproliferative syndrome (ALPS), too. Both direct and indirect coombs tests were negative. The percentage of double-negative T cells was not indicative of ALPS either. Sirolimus was started as the next line management of RDD. Later, the patient developed with high-grade fever and pancytopenia. She was admitted in the hospital. Her condition was ill. Unfortunately the patient died and the cause of death was reported as sepsis and septic shock.
Discussion and conclusion
The patient presented above highlights a notably rare disease which may present with an abdominal protrusion. The etiology of the painless abdominal mass in our patient turned out to be a non-neoplastic abnormality which was a component of rare condition named as RDD. RDD, as conceived of here, is characterized by an idiopathic proliferation of the histiocytic cells in the lymphoid tissues (Abla et al. 2018). This patient presented with an abdominal distention and low-grade fever. Initially, the patient’s history, physical examination, and imaging studies suggested lymphoma as a possible etiology. However, histopathological evaluation of mesenteric lymph node has confirmed the diagnosis of RDD.
RDD is a rare but well-defined, histiocytic proliferative disorder with a prevalence of 1:200,000 people/year. It is more often seen in children and young adults, and is more common in males (Abla et al. 2018; Warpe and More 2014). Most of patients with RDD present with massive bilateral mobile and non-tender cervical lymphadenopathy. These nodes may at times become matted and prominent due to pericapsular fibrosis. Low grade fever is mostly present along with, normocytic normochromic anemia, elevated ESR, leukocytosis, and hyperglobulinemia, which are non-specific clinical findings (Warpe and More 2014; Rosai and Dorfman 1972). In our case, there were low grade fever, anemia, leukocytosis and high ESR with abdominal lymphadenopathy.
The etiology of RDD is not clear and may be either familial or infection-induced. It has been implied to result from an immune response to an infectious agent or an aberrant response of macrophages to cytokines (Warpe and More 2014). Historically, clonality studies recommended that lesional RDD cells were polyclonal, reactive, and nonneoplastic. Studies have connected RDD with viral infections such as herpes viruses, Epstein-Barr virus, cytomegalovirus, and HIV, although a clear link has not been proven. In our case also the patient had concurrent CMV infection (Abla et al. 2018).
Most patients with RDD manifest with bilateral, massive, and painless cervical lymphadenopathy with or without intermittent fevers, night sweats, and weight loss. Extranodal involvement has been reported in 43% of RDD cases (Foucar et al. 1990; Al-Khateeb 2016). Extranodal manifestations consist of skin (10%), central nervous system (< 5%), ophthalmic (11%), head and neck (11%), intrathoracic (2%), genitourinary (4%), gastrointestinal (1%), and bone (5–10%) (Abla et al. 2018). Our case presented with hepatosplenomegaly, ascites and abdominal lymphadenopathy which are rare clinical manifestations of this disease.
Histologically, RDD in both its nodal and extranodal manifestations is characterized by sinus expansion, with proliferated large histiocytes, which show single bland-appearing nuclei with well-defined nuclear membranes, homogeneous chromatin, and single nucleoli. The cytoplasm is abundant, eosinophilic to amphophilic, and shows the hallmark feature of this disease, emperipolesis, which consists of the passage of intact, often multiple lymphocytes through the cell within intracytoplasmic vesicles (Rosai and Dorfman 1969; Abla et al. 2018; Mantilla et al. 2016). Consistent features, regardless of the site, include the cytomorphology of the large pale histiocytes and their immunophenotype. Nodal RDD is often accompanied by numerous plasma cells in the medullary cords and around the venules, with varying proportions of IgG4/IgG plasma cells (Abla et al. 2018). In contrast to nodal disease, these findings are often less noticeable in extranodal sites, which may confuse the diagnosis. The lesional histiocytes are positive for both CD68 and S-100 proteins while negative for CD1a, which helps differentiate this condition from Langerhans cell histiocytosis and Erdheim-Chester disease (Abla et al. 2018; Mantilla et al. 2016). Other differential diagnoses may include Hodgkin lymphoma, melanoma, xanthomas, lysosomal storage diseases, and several infectious and inflammatory conditions, such as histoplasmosis, leishmaniasis, inflammatory myofibroblastic tumor, and IgG4-related disease. An important point of making the diagnosis of nodal RDD is investigation for superimposed pathology, either within the node itself or other associated conditions. The presence of RDD histology is necessary, but not adequate, for the diagnosis of RDD, which depends on the proper clinical and radiologic background and exclusion of primary malignant disorders in relation to which RDD histology may represent a minor reactive process (Abla et al. 2018; Mantilla et al. 2016; Gaitonde 2007). Histopathological features indicative of malignancy were not described in our patient.
The differential diagnoses on imaging in our case include lymphoma, metastasis, granulomatous infection like tuberculosis, and Langerhans cell histiocytosis. Multiple para-aortic lymphadenopathies forming a conglomerate mass, besides mesenteric lymphadenopathies on non-contrast CT scan, all suggested lymphoma. Abdominal RDD usually resembles lymphoma (Brown and Skarin 2004) on imaging and even intraoperatively (Mantilla et al. 2016). However, there are some distinctly differentiating histopathological factors.
Most patients with RDD have spontaneous regression and do not require specific treatment (Pulsoni et al. 2002; Komp 1990). However, patients with extensive or progressive disease need treatment. Surgery is usually needed for cosmetic purposes only, or may be indicated when there is life or function-threatening obstructions like pressure effects in CNS involvements (Adeleye et al. 2010). We followed the patient after surgery and confirmed the diagnosis. She had progressed with massive splenomegaly and combination of sirolimus and corticosteroid which is recommended in the literature. The patient, consequently, presented with pancytopenia and sepsis. Associated immunological abnormalities, younger age group, extra-nodal involvement, especially the kidney and liver, are poor prognostic signs according to medical literature (Jabali et al. 2005; Oka et al. 2009).
We have described a patient who suffered painless abdominal mass and fever due to a rare disease named RDD. The other clinical presentations were hepatosplenomegaly, ascites, anemia and neutrophilia. Sinus histiocytosis with massive lymphadenopathy is a rare etiology in patients with abdominal lymphadenopathy. Also hepatosplenomegaly and ascites are other rare clinical presentations. This case scenario suggests that such non-neoplastic etiologies, like RDD, in any patient with para-aortic and mesenteric lymphadenopathy should be considered after exclusion of other common possibilities like malignant lymphoma.
Availability of data and materials
They are available if needed.
Abbreviations
- RDD:
-
Rosai dorfman disease
- ALPS:
-
Autoimmune lymphoproliferative syndrome
- CT:
-
Computed tomography
References
Abla O, Jacobsen E, Picarsic J et al (2018) Consensus recommendations for the diagnosis and clinical management of Rosai-Dorfman-Destombes disease. Blood. 131:2877–2890
Adeleye AO, Amir G, Fraifeld S, Shoshan Y, Umansky F, Spektor S (2010) Diagnosis and management of Rosai-Dorfman disease involving the central nervous system. Neurol Res 32:572–578
Al-Khateeb TH (2016) Cutaneous Rosai-Dorfman disease of the face: a comprehensive literature review and case report. J Oral Maxillofac Surg 74:528–540
Brown JR, Skarin AT (2004) Clinical mimics of lymphoma. Oncologist. 9:406–416
Foucar E, Rosai J, Dorfman R (1990) Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): review of the entity. Semin Diagn Pathol 7:19–73
Gaitonde S (2007) Multifocal, extranodal sinus histiocytosis with massive lymphadenopathy: an overview. Arch Pathol Lab Med 131:1117–1121
Jabali Y, Smrcka V, Pradna J (2005) Rosai-Dorfman disease: successful long-term results by combination chemotherapy with prednisone, 6-mercaptopurine, methotrexate, and vinblastine: a case report. Int J Surg Pathol 13:285–289
Komp DM (1990) The treatment of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease). Semin Diagn Pathol 7:83–86
Mantilla JG, Goldberg-Stein S, Wang Y (2016) Extranodal Rosai-Dorfman disease: Clinicopathologic series of 10 patients with radiologic correlation and review of the literature. Am J Clin Pathol 145:211–221
Oka M, Kamo T, Goto N et al (2009) Successful treatment of Rosai-Dorfman disease with low-dose oral corticosteroid. J Dermatol 36:237–240
Pulsoni A, Anghel G, Falcucci P et al (2002) Treatment of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): report of a case and literature review. Am J Hematol 69:67–71
Rosai J, Dorfman RF (1969) Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol 87:63–70
Rosai J, Dorfman RF (1972) Sinus histiocytosis with massive lymphadenopathy: a pseudolymphomatous benign disorder. Analysis of 34 cases. Cancer. 30:1174–1188
Warpe BM, More SV (2014) Rosai-Dorfman disease: a rare clinico-pathological presentation. Australas Med J 7:68–72
Acknowledgements
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Funding
None.
Author information
Authors and Affiliations
Contributions
Dr. Mohammad Hossein Anbardar is the primary author who led the study and did the histopathological examination. Dr. Samaneh Hamzehloo and Dr. Fatemeh Fazeli researched on the disease and write the paper. Dr. Mohammad Hadi Imanieh and Dr. Soheila Zareifar are managed the clinical aspects of the patient and study. Dr. Mohammadhossein Bahmanzadegan Jahromi and Dr. Amir Mohammad Ghorbani collect the patient data. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
It is approved.
Consent for publication
It is taken.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Anbardar, M.H., Hamzehloo, S., Fazeli, F. et al. Rosai-Dorfman disease: a rare presentation with para-aortic and mesenteric lymphadenopathy, hepatosplenomegaly and ascites. Surg Exp Pathol 3, 27 (2020). https://doi.org/10.1186/s42047-020-00076-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42047-020-00076-x