Abstract
Background
A number of studies have yielded disparate findings regarding the relationship between implant density and curve correction in adolescent idiopathic scoliosis (AIS) surgery. This study compared the efficacy and safety of low-density (LD) versus high-density (HD) pedicular screw implants in the correction of deformity in AIS regarding clinical, radiological, and quality of life outcomes.
Methods
This study was a single-blind, parallel, randomized trial that enrolled 20 adolescent patients with idiopathic scoliosis scheduled for posterior spinal fusion surgery with all pedicle screw constructs. Patients were randomized into two groups of 10 patients each. The LD group included patients in whom the number of screws per fused spinal level had a density of 1.5 or less, while the HD group had a density greater than 1.5. The primary outcomes were the radiological findings of curve correction. The secondary outcomes included the correlation between implant density and curve correction, the amount of blood loss, operation time, number of screws, fusion level, hospital stay duration, and quality of life assessed by the Scoliosis Research Society 22r questionnaire.
Results
Radiologically, the postoperative main curves Cobb angles and their changes were comparable between both approaches without statistical correlation with the implant density (p˃0.05). The LD approach significantly shortened the operative time (p=0.015), number of screws (p=0.011), implant density (p<0.001), and hospital stay (p<0.001). However, quality of life scores before surgery and at final follow-up did not differ between the two techniques (p˃0.05).
Conclusions
The use of a low-density approach is an effective and safe methodology for attaining satisfactory deformity correction in AIS patients. Furthermore, this approach confers the additional advantage of reduced operative time, number of screws, implant density, and hospital stay in comparison to the high-density approach.
Trial registration Pan African Clinical Trial Registry, PACTR202404611444119. Registered 28 March 2024-Retrospectively registered, https://pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=29382
Similar content being viewed by others
Introduction
The use of pedicle screw constructions has gained popularity in the treatment of individuals with spinal deformity. Studies have demonstrated that using thoracic pedicle screw designs in patients with adolescent idiopathic scoliosis (AIS) leads to better radiographic outcomes compared to standard hook and hybrid structures [1,2,3,4,5]. Thoracic pedicle screws have been shown to result in enhanced 3D curve correction and a lower rate of revisions. Furthermore, studies have demonstrated that they can reduce the necessity for anterior surgery in cases of severe deformity and enhance pulmonary function values [6, 7].
Posterior spinal fusion carries the risk of several complications including medial breach of spinal canal with risk of neural injury, risk of injury of major blood vessels and internal organs, and violation of the pleural cavity. An example of an extremely severe instance would be a youngster with a straightforward AIS who experienced a significant complication due to a mispositioned pedicle screw. Furthermore, the mounting costs associated with an increasing number of implants and the necessity for additional procedures due to complications resulting from implant misplacement have prompted spinal surgeons to investigate whether comparable outcomes might be achieved with a reduced number of anchors. Despite these challenges, pedicle screw fixation is widely regarded as the most advanced technique for correcting spinal deformities. While the utilization of thoracic pedicle screw constructions is widespread in the management of thoracic scoliosis, there is still ongoing discussion regarding the specifics of pedicle screw instrumentation [8].
A robust correlation has been identified between the number of screws per vertebral level (implant density) and the correction of the main curve [9,10,11]. Studies have demonstrated that the use of high-density (HD) screws is associated with enhanced restoration of thoracic kyphosis and higher ratings on the quality of life questionnaire [12, 13]. Nevertheless, extensive research has demonstrated that the use of low-density (LD) implants, with a screw density of 1.5 or less, can yield comparable radiographic and clinical results, while also offering substantial cost savings, shorter hospital stays, reduced surgery time, and decreased blood loss [14, 15]. However, the ideal number of screws per level is still uncertain when treating flexible thoracic curves. This study aimed to assess the efficacy and safety of low-density versus high-density pedicular screw implants in the correction of deformity in AIS with regard to clinical, radiological, and quality of life outcomes.
Methods
Ethical considerations
The study was approved by the Research Ethical Committee, Faculty of Medicine, Beni-Suef University, Egypt. The researchers obtained informed written consent from all study participants or their parents. The trial was registered at the Pan African Clinical Trial Registry (Trial ID: PACTR202404611444119, Date: March 28, 2024; https://pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=29382). We ensured the confidentiality of all participants’ information.
Study design, setting, and date
This single-blinded, parallel-group, randomized, controlled clinical trial was conducted at Beni-Suef University Hospitals, Egypt, between June 2022 and January 2024.
Eligibility criteria
The study included adolescents aged 10–18 years diagnosed with AIS, with a Cobb angle of 40 degrees or greater and no previous spinal surgery or thoracoplasty. They were scheduled for posterior spinal fusion surgery with all pedicle screw constructs and a 9-month follow-up. We excluded patients with any of the following: non-idiopathic scoliosis, Cobb angle < 40 degrees, associated congenital anomalies, contraindication to anesthesia, or coagulopathy.
Randomization, allocation concealment, and blinding
Twenty patients were randomized into two groups (10 patients each) using a computer-generated table. The randomization sequence was concealed using sealed opaque envelopes [16]. Only the participants were blinded to the allocation of intervention.
Interventions
Patients were divided into two groups based on average screw density. The LD group included patients in whom the number of screws per fused spinal level had a density of 1.5 or less, while the HD group had a density greater than 1.5.
Prior to the procedure, a comprehensive medical history was obtained, a clinical examination was conducted, and a range of investigations was performed, which included complete blood count, coagulation profile, liver function tests, renal function tests, pulmonary function tests, and other relevant assessments.
Following the successful administration of anesthesia, the patients were positioned in the prone position. An anatomical exposure of the spine was achieved by performing a midline incision and using a subperiosteal dissection of the paraspinal muscles. Once the location of entry point was confirmed, screws were inserted using free hand technique. The two groups demonstrated disparate quantities of pedicle screws. The corrective maneuvers were identical for both groups. Allograft bone material and the discarded laminae and transverse processes were employed for the purpose of fusion.
Postoperative care
Following surgery, patients were placed in the intensive care unit (ICU) for the initial 24 h to facilitate close monitoring of their overall bodily functions, improve pain control, maintain proper hydration levels, and assess their degree of awareness. A patient-controlled analgesia system was employed for the management of postoperative pain. All patients were permitted to ambulate either on the same evening or the following morning.
Follow-up
Follow-up was performed at 2 weeks, 3 months, 6 months, and 9 months postoperatively. Both neurologic and radiologic evaluations were performed at each visit.
Measurement tools
The Lenke classification scheme was employed [17]. A PA whole spine X-ray was conducted on a single 36-inch poster−anterior, lateral, and bending views. The following data were collected preoperatively, immediately postoperatively, at 3 months, and 9 months post-procedure. All radiographs were subjected to analysis concerning the following parameters and measurements; upper-end vertebra, lower-end vertebra, apical vertebra, upper and lower instrumented vertebrae, vertebral rotation index using Nash Moe index of vertebral rotation, right and left bending Cobb angle, lumbar spine modifier (A/B/C), thoracic sagittal profile, main thoracic Cobb angle (MT), proximal thoracic Cobb angle (PT), thoracolumbar/lumbar Cobb angle (TL/L), thoracic kyphosis at (T5–T12), lumbar lordosis at (L1–S1), and Risser’s grade [18]. The Cobb angle is a measurement utilized to assess the degree of spinal curvature in patients diagnosed with scoliosis [19].
Perioperative data were recorded to determine the operating time, estimated blood loss, hospital stay, implant costs, number of fused levels, number of screws, and screw density.
Responses to the Arabic version of the SRS 22 score which includes 22 items and assesses five categories (pain, function, self-image, mental health, and satisfaction) were collected prior to surgery and at the final follow-up after nine months [20].
Study outcomes
The primary outcomes were the radiological findings of the Cobb angle in the main thoracic (MT) and thoracolumbar/lumbar (TL/L) curves. The secondary outcomes included the correlation between implant density and curve correction, the amount of blood loss, operation time, number of screws, fusion level, hospital stay duration, and quality of life assessed by the SRS 22r questionnaire.
Statistical analysis
Data were coded and entered using the Statistical Package for the Social Sciences (SPSS) version 28 (IBM Corp., Armonk, NY, USA). Data were summarized by calculating means and standard deviations for quantitative variables and frequencies and percentages for categorical variables. Group comparisons were performed using unpaired t test for normally distributed quantitative data and Mann–Whitney test for non-normally distributed data. Paired t test was used to compare before and after measurements within each group. Chi-squared test (χ2) was used to compare categorical data. The exact test was used instead when the expected frequency was less than 5. The Spearman’s correlation coefficient was used to analyze correlations between quantitative variables. P values less than 0.05 were considered statistically significant.
Results
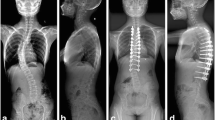
Twenty patients were randomly divided into two groups. Group LD patients were operated on with low-density implants (≤1.5 screw density), while Group HD patients were operated on with high-density implants (˃1.5 screw density) (Fig. 1).
Patients’ characteristics including age, sex, Lenke classification (Lumbar, thoracic modifiers and PT-MT-TL/L curves), Risser grade, vertebral rotation, and shoulder level did not differ significantly between groups (p=0.308, 1, 0.777, 0.332, 1, 0.628, 0.137, 1, and 0.276, respectively) (Table 1).
Table 2 shows that the preoperative, postoperative, and change/correction of Cobb angle in the MT curve and TL/L curve as well as the amount of blood loss were comparable between the two groups (p=0.241, 0.422, 0.888, 0.533, 0.120, 0.822, and 0.529, respectively). Meanwhile, the mean operating time was significantly shorter in the LD group than in the HD group (228 ± 37.8 vs. 276 ± 42 min, p=0.015). The mean number of screws in the LD group was statistically smaller than in the HD group (15.80 ± 3.43 vs. 20.40 ± 3.86, p=0.011). The mean implant density was statistically less dense in the LD group compared to the HD group (1.26 ± 0.24 vs. 1.76 ± 0.16, p<0.001). The mean of hospital stays was shorter in the LD group compared to the HD group (2.90 ± 0.32 vs. 4.40 ± 0.84 days, p<0.001). The mean number of fused levels was comparable between both groups (p=0.18).
Table 3 shows no statistically significant association between implant density and Cobb angles in MT and TL/L curve post-correction (p=0.959 and 0.618, respectively) (Figs. 2 and 3).
Using the SRS 22r questionnaire, we found no statistically significant differences between both groups in terms of pain, function/activity, mental health, self-image, and satisfaction either preoperatively (p=0.734, 0.704, 0.479, and 0.347, respectively) or at the final follow-up (p=0.808, 1.000, 0.214, 0.075, and 0.530, respectively) (Table 4).
Discussion
The relationship between implant density and correction of AIS curves has been extensively researched over the past several decades. However, research has produced conflicting results. This study aimed to compare the efficacy and safety of low-density pedicular screw implants versus high-density pedicular screw implants in the correction of deformity in adolescent idiopathic scoliosis regarding clinical, radiological, and SRS 22r questionnaire.
In our study, the results demonstrated that the LD pedicular screw implants exhibited comparable deformity correction to the HD approach, with no statistically significant correlations between curve correction and implant density. The LD approach resulted in statistically shorter operative times, fewer screws, higher implant densities, and shorter hospital stays. Nevertheless, there was no significant difference in the quality-of-life scores before surgery and at the final follow-up between the two techniques.
The objective of surgical intervention for AIS is to achieve optimal correction and successful fusion in both the coronal and sagittal planes while maintaining trunk balance [21]. Research has demonstrated that the number of fixation points plays a pivotal role in the efficacy of correction, regardless of the corrective techniques employed. Furthermore, a greater number of anchor points leads to a higher degree of curve correction. When a specific condition is met, reducing the use of screw implants does not affect the ability of deformity correction [22]. The quantity of anchor points is of great importance for the pedicle screw implants. Nevertheless, the incremental number of anchor points in the all-pedicle screw implant has a negligible impact on the final curve correction, primarily due to the enhanced pull out force of a single screw.
Consistent with our study, Morr et al. [23] found that the HD and LD approaches had similar major curve correction rates of 66.9% and 66.6%, respectively. Li et al. [24] found no statistically significant differences in the pre- and postoperative MT Cobb angle between the HD group and the LD group. Bharucha et al. [25] found that the HD group had a 66% major Cobb angle correction, while the LD group had a 63% correction. Skalak et al. [26] reported that increased implant density was not a significant factor in improving curve correction in AIS. Kemppainen et al. [27] argued that effective correction of spinal curves can be achieved with LD pedicular constructs. They found no significant difference in the degree of curve correction between HD and LD pedicular constructs. On the other hand, Larson et al. [28] conducted found that HD implants resulted in a significantly higher percentage of curve correction for Lenke 1, 2 curves. However, no relationship was observed between implant density and curve correction in Lenke 5 curves.
Several studies [24, 27, 29, 30] have shown that the density of pedicle screw implants does not affect curve correction in patients with AIS, those with a large thoracic curve, as long as they have a higher degree of curve flexibility. These findings suggest that decreasing the density of the implants is still helpful, especially for individuals with Lenke 1 AIS. Chen et al. [14] revealed a good correlation between the density of implants and the correction of thoracolumbar or lumbar coronal Cobb curves, without considering curve flexibility. However, the study did not find a significant association between screw density and correction index, after excluding the influence of flexibility using the method described by Vora et al. Clements et al. [1] found a correlation between the correction of major spinal curves and the use of high-density implants within the determined Cobb values.
The association between major surgical complications and both increased blood loss and allogeneic transfusion is well established. There is also conflicting evidence regarding the factors that contribute to increased blood loss in pediatric spinal deformity surgery [31, 32]. Increased blood loss is often correlated with higher preoperative Cobb angles, longer fusion structures, and the inclusion of osteotomies. Chang et al. [14] suggested that a reduced number of screws may lead to a reduction in bleeding and a shorter operative time. Moreover, Kilinc et al. [33] demonstrated that LD constructed fewer fused segments, lower intraoperative estimated surgical blood loss, and shorter operative time, potentially reducing the risk of complications due to fewer implants. In the current study, the mean amount of blood loss was reduced in the LD group compared to the HD group, although the difference was not statistically significant. This may be due to the relatively small number of patients included in the study, which may have been insufficient to identify significant differences.
In the current study, the LD approach significantly reduced operative time, number of screws, hospital stay, and implant density. Kemppainen et al. [27] found that the use of fewer screws than typically used in posterior pedicle screw fusion for AIS can achieve excellent curve correction, stability, and balance. The use of limited screw density constructs resulted in a reduction in operative time, as well as a reduction in risk and cost. Shen et al. [34] also found a significant reduction in operative time between the HD and LD groups, with the HD group taking 331 min and the LD group taking 278 min. In contrast, Bharucha et al. [25] found no significant difference in operative time between the HD and LD groups, with both groups taking 184 and 202 min, respectively. Li et al. [24] found no statistically significant difference in operative time between the HD and LD groups, with both groups taking an average of 201 and 195 min, respectively. Morr et al. [23] found similar results, with no statistically significant difference in operative time between the HD and LD groups (192 vs. 183 min).
Another benefit of an LD approach was its association with a reduced number of pedicle screws that need to be placed. Furthermore, intermittently positioned pedicle screws result in a considerably more significant reduction in cost than commonly believed. The exclusion of the upper and lower vertebrae, which must be instrumented to serve as the upper and lower instrumented vertebrae, respectively, in both LD and HD, results in a notable reduction in the number of pedicle screws. In a construct comprising 11 vertebral levels in the fusion, with the exclusion of the upper and lower instrumented vertebrae, the number of pedicle screws would be 8 and 18 in an LD and HD, respectively. This represents a reduction of 55.6% in the number of implants. Similarly, in a structure comprising five tiers, the quantities would be two and six screws, resulting in a reduction of 66.6% in implantation [11].
Furthermore, screw mispositioning has been associated with vascular and neurological damage, with a prevalence of 1.8–5.1% of screws being mispositioned in pediatric deformities [35]. If 10 spinal levels are fused and two screws are placed at each level, there is a possibility of one mispositioned screw per patient. Although the clinical significance of asymptomatic mispositioned implants is uncertain, using fewer implants reduces the amount of radiation during screw placement surgery. This also theoretically reduces the risk of implant malposition, the need for revision surgery to correct malposition, and the likelihood of vascular or neurological injury.
The SRS 22r questionnaire indicated that both groups exhibited improvement at the final follow-up, with no statistically significant difference between the two groups. Similarly, Morr et al. [23], Shen et al. [34], and Bharucha et al. [25] found that both approaches showed improvement in their ratings at the final 2-year follow-up. Ketenci et al. [13] observed enhanced results specifically in the self-image area of the SRS, while obtaining equivalent outcomes in the overall SRS scores.
Several studies were conducted retrospectively, based on medical records. These studies were susceptible to bias. This study represents the inaugural randomized, registered trial to assess radiological, perioperative, and quality-of-life outcomes in AIS.
The current study had a small sample size and a relatively brief follow-up period of 9 months. To address these limitations, future research should employ larger, multicenter trials with calculated sample sizes and longer follow-up periods.
Conclusions
A low-density approach is an effective and safe method for achieving satisfactory deformity correction in AIS patients. There is no correlation between curve correction and implant density. Furthermore, this approach confers the additional advantage of reduced operative time, number of screws, implant density, and hospital stay in comparison to the high-density approach.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AIS:
-
Adolescent idiopathic scoliosis
- HD:
-
High-density
- ICU:
-
Intensive care unit
- LD:
-
Low-density
- MT:
-
Main thoracic Cobb angle
- PT:
-
Proximal thoracic Cobb angle
- SRS:
-
Scoliosis research society
- TL/L:
-
Thoracolumbar/lumbar Cobb angle
References
Clements DH, Betz RR, Newton PO, Rohmiller M, Marks MC, Bastrom T. Correlation of scoliosis curve correction with the number and type of fixation anchors. Spine (Phila Pa 1976). 2009;34:2147–50.
Di Silvestre M, Bakaloudis G, Lolli F, Vommaro F, Martikos K, Parisini P. Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80 degrees: pedicle screws versus hybrid instrumentation. Eur Spine J. 2008;17:1336–49.
Fu G, Kawakami N, Goto M, Tsuji T, Ohara T, Imagama S. Comparison of vertebral rotation corrected by different techniques and anchors in surgical treatment of adolescent thoracic idiopathic scoliosis. J Spinal Disord Tech. 2009;22:182–9.
Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29:2040–8.
Suk SI, Kim WJ, Kim JH, Lee SM. Restoration of thoracic kyphosis in the hypokyphotic spine: a comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord. 1999;12:489–95.
Kim YJ, Lenke LG, Bridwell KH, Cheh G, Whorton J, Sides B. Prospective pulmonary function comparison following posterior segmental spinal instrumentation and fusion of adolescent idiopathic scoliosis: is there a relationship between major thoracic curve correction and pulmonary function test improvement? Spine (Phila Pa 1976). 2007;32:2685–93.
Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: is anterior release necessary? Spine (Phila Pa 1976). 2005;30:2061–7.
Lenke LG, Kuklo TR, Ondra S, Polly DW Jr. Rationale behind the current state-of-the-art treatment of scoliosis (in the pedicle screw era). Spine (Phila Pa 1976). 2008;33:1051–4.
Delikaris A, Wang X, Boyer L, Larson AN, Ledonio CGT, Aubin CE. Implant density at the apex is more important than overall implant density for 3D Correction in thoracic adolescent idiopathic scoliosis using rod derotation and en bloc vertebral derotation technique. Spine (Phila Pa 1976). 2018;43:E639–47.
Sariyilmaz K, Ozkunt O, Karademir G, Gemalmaz HC, Dikici F, Domanic U. Does pedicle screw density matter in Lenke type 5 adolescent idiopathic scoliosis? Medicine (Baltimore). 2018;97: e9581.
Luo M, Wang W, Shen M, Luo X, Xia L. Does higher screw density improve radiographic and clinical outcomes in adolescent idiopathic scoliosis? A systematic review and pooled analysis. J Neurosurg Pediatr. 2017;19:448–57.
Liu H, Li Z, Li S, Zhang K, Yang H, Wang J, et al. Main thoracic curve adolescent idiopathic scoliosis: association of higher rod stiffness and concave-side pedicle screw density with improvement in sagittal thoracic kyphosis restoration. J Neurosurg Spine. 2015;22:259–66.
Ketenci IE, Yanik HS, Demiroz S, Ulusoy A, Erdem S. Three-dimensional correction in patients with lenke 1 adolescent idiopathic scoliosis: comparison of consecutive versus interval pedicle screw instrumentation. Spine (Phila Pa 1976). 2016;41:134–8.
Chen J, Yang C, Ran B, Wang Y, Wang C, Zhu X, et al. Correction of lenke 5 adolescent idiopathic scoliosis using pedicle screw instrumentation: does implant density influence the correction? Spine (Phila Pa 1976). 2013;38:E946–51.
Min K, Sdzuy C, Farshad M. Posterior correction of thoracic adolescent idiopathic scoliosis with pedicle screw instrumentation: results of 48 patients with minimal 10-year follow-up. Eur Spine J. 2013;22:345–54.
Doig GS, Simpson F, Delaney A. A review of the true methodological quality of nutritional support trials conducted in the critically ill: time for improvement. Anesth Analg. 2005;100:527–33.
Pasha S, Ho-Fung V, Eker M, Nossov S, Francavilla M. Three-dimensional classification of the Lenke 1 adolescent idiopathic scoliosis using coronal and lateral spinal radiographs. BMC Musculoskelet Disord. 2020;21:824.
Charles YP, Diméglio A, Canavese F, Daures JP. Skeletal age assessment from the olecranon for idiopathic scoliosis at Risser grade 0. J Bone Joint Surg Am. 2007;89:2737–44.
Kuklo TR, Potter BK, Lenke LG. Vertebral rotation and thoracic torsion in adolescent idiopathic scoliosis: what is the best radiographic correlate? J Spinal Disord Tech. 2005;18:139–47.
Berven S, Deviren V, Demir-Deviren S, Hu SS, Bradford DS. Studies in the modified scoliosis research society outcomes Instrument in adults: validation, reliability, and discriminatory capacity. Spine (Phila Pa 1976). 2003;28:2164–9.
Seo SH, Hyun SJ, Lee JK, Cho YJ, Jo DJ, Park JH, et al. Selection of optimal lower instrumented vertebra for adolescent idiopathic scoliosis surgery. Neurospine. 2023;20:799–807.
Larson AN, Aubin C-E, Polly DW, Ledonio CGT, Lonner BS, Shah SA, et al. Are more screws better? A systematic review of anchor density and curve correction in adolescent idiopathic scoliosis. Spine Deform. 2013;1:237–47.
Morr S, Carrer A, Alvarez-García de Quesada LI, Rodriguez-Olaverri JC. Skipped versus consecutive pedicle screw constructs for correction of Lenke 1 curves. Eur Spine J. 2015;24:1473–80.
Li M, Shen Y, Fang X, Ni J, Gu S, Zhu X, et al. Coronal and sagittal plane correction in patients with Lenke 1 adolescent idiopathic scoliosis: a comparison of consecutive versus interval pedicle screw placement. J Spinal Disord Tech. 2009;22:251–6.
Bharucha NJ, Lonner BS, Auerbach JD, Kean KE, Trobisch PD. Low-density versus high-density thoracic pedicle screw constructs in adolescent idiopathic scoliosis: do more screws lead to a better outcome? Spine J. 2013;13:375–81.
Skalak TJ, Gagnier J, Caird MS, Farley FA, Li Y. Higher pedicle screw density does not improve curve correction in Lenke 2 adolescent idiopathic scoliosis. J Orthop Surg Res. 2021;16:276.
Kemppainen JW, Morscher MA, Gothard MD, Adamczyk MJ, Ritzman TF. Evaluation of limited screw density pedicle screw constructs in posterior fusions for adolescent idiopathic scoliosis. Spine Deform. 2016;4:33–9.
Larson AN, Polly DW Jr, Diamond B, Ledonio C, Richards BS 3rd, Emans JB, et al. Does higher anchor density result in increased curve correction and improved clinical outcomes in adolescent idiopathic scoliosis? Spine (Phila Pa 1976). 2014;39:571–8.
Yang S, Jones-Quaidoo SM, Eager M, Griffin JW, Reddi V, Novicoff W, et al. Right adolescent idiopathic thoracic curve (Lenke 1 A and B): does cost of instrumentation and implant density improve radiographic and cosmetic parameters? Eur Spine J. 2011;20:1039–47.
Quan GM, Gibson MJ. Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation: does higher implant density improve correction? Spine (Phila Pa 1976). 2010;35:562–7.
Jain A, Njoku DB, Sponseller PD. Does patient diagnosis predict blood loss during posterior spinal fusion in children? Spine (Phila Pa 1976). 2012;37:1683–7.
Hassan N, Halanski M, Wincek J, Reischman D, Sanfilippo D, Rajasekaran S, et al. Blood management in pediatric spinal deformity surgery: review of a 2-year experience. Transfusion. 2011;51:2133–41.
Kilinc BE, Tran DP, Johnston C. Comparison of implant density in the management of Lenke 1B and 1C adolescent idiopathic scoliosis. Acta Ortop Bras. 2019;27:33–7.
Shen M, Jiang H, Luo M, Wang W, Li N, Wang L, et al. Comparison of low density and high density pedicle screw instrumentation in Lenke 1 adolescent idiopathic scoliosis. BMC Musculoskelet Disord. 2017;18:336.
Larson AN, Santos ER, Polly DW Jr, Ledonio CG, Sembrano JN, Mielke CH, et al. Pediatric pedicle screw placement using intraoperative computed tomography and 3-dimensional image-guided navigation. Spine (Phila Pa 1976). 2012;37:E188–94.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
HM, AM, HE, AK, and OR have full access to all the data in the study and take responsibility for the integrity of the data. HM and AM contributed to study concept and design; AM, HE, and AK contributed to acquisition of data; HM, AM, and OR carried out analysis of data; AM, HE, and AK drafted the manuscript; HM and OR performed critical revision of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethical Committee, Faculty of Medicine, Beni-Suef University, Egypt. The researchers obtained informed written consent from all study participants or their parents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mostafa, H.E., Moustafa, A.S.S., El Zayat, H.H. et al. Comparative study of low-density versus high-density pedicular screw implantations in management of adolescent idiopathic scoliosis: a randomized clinical trial. Egypt J Neurosurg 39, 52 (2024). https://doi.org/10.1186/s41984-024-00308-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-024-00308-2