Abstract
Background
Mild traumatic brain injury (TBI) occupies majority of head traumas in most emergency units. Although patients with mild TBI can be reviewed and discharged on head injury advice, a sizeable number require admission for observation or intervention due to operable intracranial lesions. The aim of the study was to establish the prevalence of operable lesions in patients with mild TBI.
Materials and methods
This was a prospective study of consecutive adult patients with mild TBI who had cranial computerized tomography (CT) done at the National Trauma Centre, Abuja. All participants gave informed consent and the study had ethical clearance in the Hospital.
Results
One hundred and three mild TBI patients with cranial CTs were recruited aged 16–76 years with mean age of 32.25\(\pm\)12.35 years. With intention to treat, twenty (20.4%) of them were diagnosed with operable intracranial lesions on CT scans, 19 males and 2 females. Majority of them (14; 66.7%) were young adults within 20–40 years of age. The lesions were 16 extradural haematomas (76.2%), 3 subdural haematomas (14.3%) and 2 depressed skull fractures (9.5%) of the operable cohort.
Conclusions
Significant number of patients with mild TBI had operable intracranial lesions. Therefore, there is need to screen patients with mild TBI appropriately in order to avoid missed operable lesions.
Similar content being viewed by others
Introduction
Trauma is a leading cause of death in the world, and brain injury contributes a significant proportion of that mortality, hence it is a public health emergency [1]. Traumatic Brain Injury (TBI) can be defined as an acquired nondegenerative insult to the brain from an external mechanical force, that leads to permanent or temporary impairment of cognitive, physical, and psychosocial functions, with an associated diminished or altered state of consciousness [2, 3]. Whereas minor head injury “(MHI) is defined as blunt head injury with a Glasgow Coma Scale score of 13–15 at presentation” [4] or as a blunt injury to the head which is accompanied with temporary loss of consciousness, amnesia or disorientation/confusion with a Glasgow Coma Score of 13–15 [5].
In Nigeria, there is no national epidemiological data. However, mild TBI is also the most common form of head injuries reported in hospitals. [6, 7]. Mild TBI constitute about 80–90% of all TBIs, and may have intracranial pathologies requiring neurosurgical intervention in about 10% of cases, 1% of which could be life-threatening [8]. The “need for neurosurgical intervention” is defined as either death or need for any of the following procedures within 30 days of the acute head injury: craniotomy, monitoring of intracranial pressure, or the need for intubation for the treatment of head injury [6]. The exact percentage of such injuries with operable lesions is yet to be established in our environment. The aim of this study was to establish the prevalence of intracranial lesions that require neurosurgical intervention due to mild head trauma following computerized tomography (CT) scan. This includes intention to treat irrespective of whether an intervention took place or not. However, in this index study we were limited to only operable intracranial lesions like haematomas, and skull fractures.
Materials and methods
The study was a prospective descriptive study. Participants were adult patients above 16 years of age who presented with mild TBI within 24 h to the National Trauma Centre, Abuja and had cranial CT. Patients’ demography, mechanism of injury, history of either loss of consciousness, disorientation or amnesia and GCS 13-15 were part of data collected. Data was entered into IBM SPSSR and analyzed using version 25.0. The study was approved by the Institutional Review Board of the hospital. All patients that participated gave consent either by themselves or through their relatives.
Results
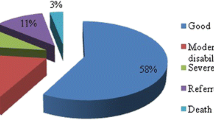
One hundred mild TBI patients with cranial CTs were recruited aged 16–76 years with mean age of 32.25 \(\pm\) 12.35 years. With intention to treat, twenty-one (20.4%) of them were diagnosed with operable intracranial lesions on CT scan, 19 males and 2 females. In this cohort, majority of them (14; 66.7%) were young adults within 20–40 years of age. The most common mechanism of injury was road traffic accident (RTA)—66.7%, followed by assaults (14.3%), falls (9.5%), and undescribed injury mechanism (9.5%). See Table 1 for details. About eighty percent of the patients with operable lesions had history of loss of consciousness, however only about 35% had history of amnesia. The lesions were 16 extradural haematomas (76.2%), 3 subdural haematomas (14.3%), and 2 depressed skull fractures (9.5%) in the study cohort. Surgeries done were 12 craniotomies for evacuation of extradural haematomas (57.1%), 2 elevations of depressed skull fractures (9.5%) and 2 craniectomies for evacuation of acute subdural haematoma (9.5%). See Table 2 for frequency of operable lesions with their spread and comparison in Fig. 1.
Discussion
The results of our index study revealed about 20% operable intracranial lesions with the intention to treat among patients with mild TBI. This was higher than 10% of patients with mild TBI reported to have intracranial pathologies requiring neurosurgical intervention and 1% of which could be life-threatening [8]. This difference could be due to difference in selection criteria for ordering CT scan in patients with mild TBI or the lack of universal insurance coverage in our setting resulting in fewer patients being able to afford CT scan among eligible patients thereby increasing the specificity of the investigation. The most common mechanism of injuries for mild TBI patients with operable lesions was road traffic crashes (66.7%) with no significant difference between the subtypes in our study. This is similar to findings in some previous studies, Chobdari et al. in Iran reported, where automobile accidents (especially drivers) were the most frequent cause of mild TBI (35.5%) and falls the least cause (9.4%) [9]. On the other hand, falls and sport injuries have been reported to have the most common cause of mild TBI in studies in Turkey and China [10, 11]. Extradural haematomas (16) were the most frequent operable intracranial lesions in our study (76.2% of the subgroup), while subdural haematomas (~ 3% of the general study but 14.3% of the subgroup), which was the second frequent in our study was the most frequent in a similar study in Iran (31.7%) and depressed skull fracture the least frequent (1.9%) with similarity in the mechanisms of injury [9]. On the other hand, where most prevalent mechanism is fall or sports injuries, they tend to have lower percentage of significant brain injuries or lesions requiring neurosurgical interventions. Kavalci et al. [10] in a prospective study conducted in a city hospital in Turkey found subarachnoid haemorrhage as the most frequent CT scan finding. In China, Yang et al. [12], falling was the most common mechanism of injury (43.68%) and skull fracture the most common injury (8%) while those who underwent surgery were 1.76%.
There is usually a dilemma as to which category of patients with mild TBI should have brain CT scan done for efficient use of resources, cost saving and avoidance of radiation hazard consequent on over use of CT scan. This is the reason why clinical decision rules were developed. Decision rules help the emergency physician to determine who with mild TBI should go for cranial CT scan or not by using a set of criteria that has been validated. The significant findings (~ 20%) of operable intracranial lesion in our study underscore the need to apply any of the validated clinical decision rules in determining which patient should scanned. However, our centre is still in the process of adopting an easy clinical decision rule for routine practice.
Conclusions
Mild TBI can be associated with significant operable intracranial lesions especially when most of such injuries are results of road traffic crashes as demonstrated by our study. Proper evaluation should be done all times to exclude significant injuries that would require neurosurgical interventions, so as not to pass off dangerous cases as safe due to high GCS.
Recommendations
We recommend that all accident and emergency units or trauma departments review and adopt a clinical decision rule to effectively screen patients with mild TBI. This would make it easy for resident doctors and emergency physicians to be acquainted with the clinical decision rule for efficient usage.
Availability of data and materials
Data is available on reasonable request.
Abbreviations
- CT:
-
Computerized tomography
- TBI:
-
Mild traumatic brain injury
- RTA:
-
Road traffic accident
- MHI:
-
Minor head injury
- GCS:
-
Glasgow coma scale
References
American Association for the Surgery of Trauma. 2020 [cited 2020 Nov 12]. Available from: https://www.aast.org/resources/trauma-facts#:~:text= In the United States%3A 1 Trauma, Sheet from the NVIPC at CDC More
Dawodu ST. Traumatic brain injury (TBI)—definition, epidemiology, pathophysiology: overview, epidemiology, primary injury [Internet]. 2019 [cited 2020 Oct 4]. Available from: https://emedicine.medscape.com/article/326510-overview#showall
Pervez M, Kitagawa RS, Chang TR. Definition of traumatic brain injury, neurosurgery, trauma orthopedics, neuroimaging, psychology, and psychiatry in mild traumatic brain injury [Internet]. vol. 28, Neuroimaging Clinics of North America. W.B. Saunders; 2018 [cited 2020 Oct 4]. pp. 1–13. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1052514917301181
Smits M, Dippel DWJ, Nederkoorn PJ, Dekker HM, Vos PE, Kool DR, van Rijssel DA, Hofman PA, et al. Minor head injury: CT-based strategies for management—a cost-effectiveness analysis. J Radiol. 2010;254(2):532–40.
Stiell IG, Clement CM, Rowe BH, Schull MJ, Brison R, Cass D, et al. Comparison of the Canadian CT head rule and the New Orleans criteria in patients with minor head injury. J Am Med Assoc. 2005;294(12):1511–8.
Bouida W, Marghli S, Souissi S, Ksibi H, Methammem M, Haguiga H, et al. Prediction value of the Canadian CT head rule and the New Orleans criteria for positive head CT scan and acute neurosurgical procedures in minor head trauma: a multicenter external validation study. Ann Emerg Med. 2012;61:521–7.
Kavalci C, Aksel G, Salt O, Yilmaz MS, Demir A, Kavalci G, et al. Comparison of the Canadian CT head rule and the new orleans criteria in patients with minor head injury. World J Emerg Surg. 2014;9(1):1–5.
Vos PE, Alekseenko Y, Battistin L, Ehler E, Gerstenbrand F, Muresanu DF, et al. Mild traumatic brain injury. Eur J Neurol. 2012;19:191–8.
Chobdari N, Sharifi MD, Kakhki BR, Shamsaei S, Disfani HF, Hashemian AM. Evaluation of sensitivity and the specificity of Canadian CT head rule and New Orleans criteria in patients with head injury. Australas Med J. 2018;11(3).
Kavalci C, Aksel G, Salt O, Serkan Yilmaz M, Demir A, Kavalci G, et al. Comparison of the Canadian CT head rule and the new orleans criteria in patients with minor head injury [Internet]. 2014 [cited 2020 Jun 21]. Available from: http://www.wjes.org/content/9/1/31
Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001;357(9266):1391–6.
Yang X-F, Meng Y-Y, Wen L, Wang H. Criteria for performing cranial computed tomography for Chinese patients with mild traumatic brain injury: Canadian computed tomography head rule or new orleans criteria. J Craniofac Surg. 2017;00(00):1–4.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
SPKK, conceptualized, gathered and analyzed the data, wrote the original draft and effected all contributions and corrections. ASY supervised the research, reviewed draft critically for intellectual content and approved the version for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Study was approved by the hospital’s research and ethics committee and all eligible participants, or their wards gave informed consent.
Consent for publication
Consent for publication was obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kpuduwei, S.P.K., Yusuf, A.S. Prevalence of operable intracranial lesions from mild traumatic brain injury in a National Trauma Centre. Egypt J Neurosurg 39, 5 (2024). https://doi.org/10.1186/s41984-024-00268-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-024-00268-7