Abstract
Background
Lumbar discectomy has successful initial clinical outcome; its long-term success rate decreases to 40–80% due to chronic low back pain and recurrent disc herniation.
Objective
To evaluate the clinical results of Posterior Lumbar Interbody Fusion with a single unilateral stand-alone PEEK (Poly-Ether-Ether-Ketone) cage without pedicle screw fixation for single level lumbar disc herniation.
Methods
A retrospective study of 40 patients (24 men and 16 women) with lumbar disc herniation, was conducted in the period from January 2016 through January 2021. The follow-up continued till December 2021. All patients suffered from single level lumbar disc herniation and were treated with Posterior Lumbar Interbody Fusion with a single unilateral stand-alone PEEK cage without pedicle screw fixation.
Results
The affected levels were L2–3 in 2 cases, L3–4 in 8 cases, L4–5 in 18 cases and L5–S1 in 12 cases. On 18th month follow-up, significant decrease in leg pain, LBP and ODI scores was detected (p < 0.001).
Conclusions
This technique produced satisfying clinical enhancement in residual LBP, accepted radiological outcome such as maintaining the proper intervertebral disc space and prevention of recurrent disc herniation.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Low-back pain (LBP) is the primary reason of long-term disabilities globally, with an 18%-point incidence and 38% 1-year incidences [1]. Degenerative disc disease (DDD) or lumbar disc herniation (LDH) is the most prevalent cause of LBP [2].
Lumbar discectomy with Excision of the herniated nucleus pulposus, remains the best surgical treatment for this disease. Although Lumbar discectomy has successful initial clinical outcome, its long-term success rate decreases to 40–80% due to chronic low back pain and recurrent disc herniation [3]. Lumbar discectomy is combined with interbody fusion to avoid residual low back pain and prevent recurrent disc herniation [4]. The necessity and efficiency of interbody fusion after single level simple lumbar discectomy are still controversial [5].
Various procedures like transforaminal lumbar interbody fusion (TLIF), anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion (PLIF) and interbody cage devices have been developed for fusion [4]. Cloward first described PLIF for LDH [6]. A successful PLIF restores disc height, immobilizes the unstable degenerated motion segment, decompresses the nerve roots, and restores load bearing to anterior parts [7].
PLIF is usually a bilateral technique. Fixation with bilateral posterior pedicle screws supported with bilateral two interbody cages, has become routinely as a typical PLIF procedure [8, 9].
However, it is really hard to place two cages of the suitable size bilaterally one on each side without wide exposure. Extensive laminectomy and bilateral facetectomy may result in iatrogenic instability [10]. Therefore, several clinical reports advised pedicle screws fixation with PLIF to obtain satisfactory clinical and radiological results. [11, 12] The overexposure necessary for a circumferential fusion might result in unneeded damage to the lumbar musculoligamentous complex, that is considered one of the reasons of a residual LBP [13].
On the other hand, unilateral facetectomy is known not to cause obvious instability [14,15,16]. Is fixation with posterior pedicle screws mandatory for PLIF in patients with unilateral facetectomy?
Objective To evaluate the clinical results of Posterior Lumbar Interbody Fusion (PLIF) with a single unilateral stand-alone PEEK (Poly-Ether-Ether-Ketone) cage without pedicle screw fixation for single level lumbar disc herniation.
Methods
A retrospective study of 40 patients (24 men and 16 women) with lumbar disc herniation, was conducted in the period from January 2016 to January 2021, the follow-up continued till December 2021. The mean age at the time of surgery was 44 years (22–62 year). The affected levels were L2–3 in 2 patients, L3–4 in 8 patients, L4–5 in 18 patients and L5–S1 in 12 patients.
Preoperative assessment consisted of a comprehensive examination of the patients and their radiographic data which comprised plain anteroposterior and lateral standing radiographs with flexion and extension lateral films to assess disc space high and segmental stability. Magnetic resonance imaging (MRI) was done for all cases to determine level of LDH and site of neural compression.
The inclusion criteria were:
-
Severe LBP and leg pain refractory to conservative therapy for 3 months.
-
MRI of the lumbar spine showing evidence of single level LDH with neural compression.
-
Plain radiographs revealed wide disc space.
The Exclusion Criteria were:
-
LBP only.
-
Multilevel LDH.
-
Instabilities in the dynamic lateral X-ray
-
Narrow disc space in the lateral X-ray.
-
Recurrent lumbar disc herniation.
Surgical technique
This procedure was done under general anesthesia with the Patient in the prone position. A midline posterior incision was done, the paravertebral muscles were subperiosteally dissected and laterally retracted to expose the lamina and facet joints. Following the laminectomy, a partial medial UF was done. Adequate foraminotomy was done and the facet joints were preserved as much as possible. The thecal sac and traversing nerve root were mobilized and medially retracted. Using pituitary rongeurs, a rotate-cutter, shavers and down-biting curved curettes, the disc content and endplates were excised as much as feasible. Using down-biting curettes and a specifically constructed curved rotate-cutter, the disc content and endplates on the contralateral side should be as thoroughly removed as feasible. The disc space distraction was done by inserting and manipulating disc spreaders. We utilized a single PEEK cage (Medi Tech, Egypt) as a hollow ramp; a rectangular implant with rounded sides and varied heights (13 mm, 11 mm, and 9 mm) that allows for simple insertion. The cages were chosen with consideration for the intervertebral disc height.
Prior to cage implantation, Cancellous bone obtained from Laminectomy was utilized to fill the PEEK cages' chambers as much cancellous bone as feasible was transplanted into the anterior sides of the intervertebral disc space.
To prevent posterior displacement of the cage, we used a large cage as we can and the cage was inserted to the disc space and carefully pushed to the contralateral side with the impactor to be deep, transverse and firm. After achieving full hemostasis, the incision was closed in layers.
On the first day after surgery, all cases were permitted to walk with a lumbar orthosis, that was worn for one to two months.
Each case's age, gender, degree and length of surgery, and hospital stay were documented. All cases were followed up during the second week, 2nd month, 6th month, 12th month, and 18th month after surgery. In the early period after surgery and on the 12th month, all of the cases had X-ray imaging. On the 12th month, CT scans of the lumbar vertebra were used to examine the stability and fusion of PLIF cases. Regarding CT imaging, the height of IVDS and fusion rates were measured.
The Oswestry disability index (ODI) and visual analogue scale (VAS) scores were assessed preoperatively and 18 months postoperatively.
The VAS score was determined by asking the case to place the level of discomfort on a horizontal scale from 0 to 10, with 0 indicating no pain and 10 indicating the most severe pain.
ODI is a global instrument that measures disability as follows: 0–20; minimal disability, 20–40; mild disability, 40–60; intermediate degree of disability, 60–80; disabling pain and 80–100; bedridden with severe pain.
Statistical Methods
Data were statistically presented in terms of range, mean and frequencies. Comparison of the pre and postoperative means to estimate the significance was performed utilizing the paired “t” test. All statistical analysis were done utilizing SPSS (Statistical Package for the Social Science version 15; SPSS Inc., Chicago, IL, USA).
Results
The affected levels were L2–3 in 2 cases, L3–4 in 8 cases, L4–5 in 18 cases and L5–S1 in 12 cases. Table 1.
On 18th month follow-up, significant decrease in leg pain, LBP and ODI scores was detected (p <0.001). Table 2.
The mean operation duration was 50 min. The mean estimated blood loss was 150 ml. Mean hospital stay was 1 day. Neither a significant complication nor neurologic damage was noticed during the procedure or after it. On the postoperative 10th day, one case developed superficial surgical site infection and was treated with antibiotics. No recurrence was recorded.
Depending on a comparison before surgery with one-year CT imaging, the height of the IVDS was maintained in every case. CT imaging revealed the progression of fusion in 80% of cases. Radiological instability was not detected.
Discussion
Simple Lumbar Discectomy is a commonly performed and highly approved procedure for LDH. Some authors observed satisfactory initial results with success rates of over 90% [17, 18] while others observed less favorable long-term results with success rates ranging from 40 to 79% [3, 19,20,21,22].
Residual LBP and recurrent LDH were significant factors in determining the long-term outcome of Simple Lumbar Discectomy; Residual low back pain after simple discectomy was documented in 44% of cases by Frymoyer et al. [20], 27% of cases by Kotilainen [23], 21% of cases by Loupasis [3], 54% of cases by Nachlas [24], and 47% of cases by Vaughan et al. [25], and 61% of the non-fusion group by Takeshima et al. [26]. The frequency of residual low back pain after simple discectomy is definitely high (21–61%). Caldwell and Sheppard reported an incidence of 8% for recurrent LDH [27], Eie reported 10% [28], Loupasis et al reported 7.3%, Rish reported 18% [29], Takeshima et al reported 18% [26], Tominaga et al reported 12.5% [30], and Vaughan et al reported 15.4% [25]. Their frequency of recurrent LDH (7.3–18%) is not low.
This retrospective study was conducted on forty patients suffering from single level LDH with preserved intervertebral disc space height. Patients with fracture pars and instability were excluded neural decompression with laminectomy and discectomy was done followed by PLIF by the inserting of the appropriately sized cages in the intervertebral disc space without pedicle screw fixation.
Cloward pioneered the PLIF procedure, which has the benefit of restoring IVD height, sagittal plane alignment, and anterior column weight bearing [9, 10, 31]. After the development of several cages for PLIF, both surgery and its results have undergone significant improvement. The majority of surgeons advocate supplementing PLIF with posterior pedicle screw fixation [11, 31, 32]. To achieve a circumferential fusion of the segment, though, additional exposing and disturbance of the posterior parts would be required. According to much research, iatrogenic soft tissue damage is associated with unfavorable long-term clinical consequences [33]. Wide exposure and extensive intra-operative dissection of paraspinal muscles may result in denervation and atrophy. The injured muscle tissue works as a source of pain, which increases the likelihood of "failed back syndrome" [34]. Bilateral aggressive facetectomy can lead to instability and postoperative pain. Wide exposure and circumferential fusion might thus create iatrogenic flat back syndrome in individuals with persistent LBP and LDH.
For the management of a degenerative lumbar condition, an interbody fusion with a cage alone is gaining popularity [13]. Conversely, several spine surgeons have questioned PLIF with stand-alone cages owing to the requirement to remove a substantial percentage of the posterior spinal support components. In several biomechanical experiments, bilateral PLIF without extra posterior instrumentation resulted in considerable destabilizing of the fused segment [35]. In bilateral PLIF, large bilateral bony and ligamentous structures are often needed for the precise placement of implants of the correct size. No reports exist of segmental destabilization after unilateral facetectomy without pedicle screw fixation [16]. However, in our study we utilized unilateral single PEEK cage and made limited laminectomy and facetectomy.
According to a cadaveric study, the destruction of posterior stabilizing structures: posterior longitudinal ligament, the lamina and intervertebral disc, after simple lumbar discectomy resulted in remarkable instability of all test measurements, notably flexion-extension. Using only PLIF, reduces mean angular displacement and percentage of range of motion (ROM) regaining stiffness to near intact levels [36].
Blume reported in 1985; unilateral PLIF utilizing a bone dowel and cancellous bone chip preserved the integrity of the posterior ligament elements. In contrast, PLIF with bone only without cages may result in disc space collapse over time [37] (Fig. 1).
Male patient, 46 years old, presented with LBP and bilateral sciatica. a, b sagittal and axial MRI T2 images revealed L4–5 LDP causing neural compression. c plain X-ray LSS lateral view revealed L4–5 discectomy and PLIF with a stand-alone cage. Postoperatively, LBP and bilateral sciatica were completely resolved (Excellent outcome)
Zhao et al. described the oblique placement of a one threaded interbody fusion cage for the treatment of degenerative spondylolisthesis. [38] They observed that a unilateral facetectomy enabled enough decompression for the secure placement of the cage device, even as preserving the essential posterior supporting spinal structures. They observed that PLIF with a single long threaded cage placed obliquely via a unilateral facetectomy and hemi-laminectomy, was significantly stiffer than PLIF done with two posterior cages placed via a bilateral laminectomy and facetectomy [39] (Fig. 2)
Male, 42 years, presented with LBP and Lt femoralgia. a, b sagittal and axial MRI T2 images revealed L2–3 LDP causing neural compression. c, d preoperative plain X Ray LSS Lateral and A-P views. e, f postoperative plain X Ray LSS, A-P and Lateral views showing L2–3 laminectomy and discectomy with PLIF with a stand-alone cage. L4–5 laminectomy with foraminotomy was done at this stenosed level
Abumi et al observed that a bilateral facetectomy increased significantly flexion and axial rotation, while a unilateral facetectomy did not affect significantly in motions, particularly in rotation [40].
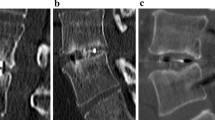
With our surgical approach, an ipsilateral total facetectomy was not necessary. For a PLIF with one cage, a partial hemi-laminectomy or total laminectomy and medial UF were sufficient. We believe that additional posterior transpedicular screw fixation is not required as far as the facet joints are preserved and the other posterior structures can maintain their natural ROM in flexion and rotation. To increase solid bone fusion, an extra bone graft could be inserted to the contralateral disc space prior to the insertion of the cage without the danger of posterior retropulsion. We had no cases of cage posterior retropulsion. The possibility of posterior retropulsion of stand-alone cages can be avoided by inserting a cage with appropriate size (Fig. 3).
Female patient, 42 years old, presented with LBP and Rt sciatica. a, b preoperative X Ray LSS; lateral, A-P views. c Preop axial CT scan. d, e sagittal and axial MRI T2 images revealed L4–5 LDP causing neural compression. f, g plain X-ray LSS lateral and A-P view revealed L4–5 discectomy and PLIF with a stand-alone cage. h, i postoperative sagittal and axial MRI T2 images revealed L4–5 discectomy and PLIF with a stand-alone cage. j, k postoperative CT LSS revealed L4–5 discectomy and PLIF with a stand-alone cage. Postoperatively, LBP and bilateral sciatica were completely resolved (Excellent outcome)
In this study, the rate of radiological bone fusion was marginally decreased than that of other PLIF procedures. A sound fusion is believed to be a therapeutic success factor for individuals with mechanical LBP. However, there was no correlation among fusion rates and clinical findings in our cases. In previous research, the clinical findings did not necessarily correspond to the radiographically firm fusion [41].
According to Agazzi et al., a PLIF with a stand-alone cage may restore the disc height, preserve the sagittal balance and improve the clinical outcome despite the lack of solid fusion [13].
In patients with posterior fixation, the fusion rates are 89–100% [14, 42,43,44,45,46].
In our study, the rates of clinical improvement and radiological stability are comparable to fusion cases. As previously noted, clinical improvements are not fully correlated with fusion rates [14, 42,43,44,45,46].
In our study, intervertebral disc height was maintained in all cases. The cage size that would be inserted into the intervertebral disc space after discectomy has great importance. Goh et al. concluded that cages as large as possible are essential to restore the stiffness of the facetectomized functional spine units especially in torsion motion [47].
None of the cases were found to have segmental instability. Long-term follow-ups of these cases may give further information on these potential problems.
Another possible complication of lumbar fusion surgery is adjacent segment disease. Its occurrence ranges from 5.2 to 29.6% [48,49,50]. In our study, radicular complaints were not seen in PLIF cases; hence, an MRI was unnecessary. It is also documented that not all adjacent segment disease cases are clinically symptomatic [4]. According to the data from our study, it is unable to comment on adjacent segment disease.
Postoperatively, individuals with LDH have shown improved LBP outcomes [25, 29, 51]. In our research, an enhancement in VAS and ODI scores was detected. The leg pain and LBP enhanced significantly.
Recurrent disc herniation is another significant factor influencing the long-term prognosis of LDH cases. Its occurrence is estimated to range between 7.3 and 18.0% after simple discectomy [3, 4, 29]. Rish suggested spinal fusion as the first procedure for LDH [29]. Satoh et al. demonstrated PLIF might prevent repeated LDH [4]. They indicated fusion in cases with massive herniation and the presence of segmental instability [4]. No recurrent LDH was reported in our cases that underwent PLIF. We believe that, PLIF procedure without instrumentation should be used from the start in patients with preserved intervertebral disc height, for the prevention of recurrent disc herniation.
Polyether ether ketone (PEEK) cages give better load transfer and increased fusion on computed tomography (CT) images, the cage radiolucency should result in better assessment of fusion [52].
Conclusions
Unilateral PLIF with single PEEK cage without posterior pedicle screw fixation after single level lumbar discectomy was safe and effective method in cases with single level LDH with preserved intervertebral disc height. This technique produced satisfying clinical enhancement in residual LBP, accepted radiological outcome such as maintaining the proper intervertebral disc space and prevention of recurrent disc herniation.
Availability of data and materials
Not applicable.
Abbreviations
- LBP:
-
Low-back pain
- DDD:
-
Degenerative disc disease
- LDH:
-
Lumbar disc herniation
- TLIF:
-
Transforaminal lumbar interbody fusion
- ALIF:
-
Anterior lumbar interbody fusion
- PLIF:
-
Posterior lumbar interbody fusion
- PEEKCage:
-
Poly-Ether-Ether-Ketone cage
- MRI:
-
Magnetic resonance imaging
- IVDS:
-
Intervertebral disc space
- ODI:
-
The Oswestry disability index
- VAS:
-
Visual analogue scale scores
- ROM:
-
Range of motion
References
Hoy D, Bain C, Wiliams G. A systematic review of the global prevelance of low back pain. Arthritis Rheum. 2012;64:2028–37.
Nozomu I, Espinoza Orías AA. Biomechanics of intervertebral disc degeneration. Orthop Clin N Am. 2011;42:487–99.
Loupasis GA, Stamos K, Katonis PG, Sapkas G, Korres DS, Hartofilakidis G. Seven- to 20-year outcome of lumbar discectomy. Spine. 1999;24:2313–7.
Satoh I, Yonenobu K, Hosono N, Ohwada T, Fuji T, Yoshikawa H. Indication of posterior lumbar interbody fusion for lumbar disc herniation. J Spinal Disord Tech. 2006;19:104–8.
Sun Z, Li W, Chen Z, Guo Z, Qi Q, Zeng Y. Decompression alone versus decompression with instrumented fusion for young patients with single-level lumbar disc herniation: a short-term prospective comparative study. Chin Med J. 2014;127(11):2037–42.
Cloward RB. The treatment ruptured intervertebral disc by vertebral body fusion. J Neurosurg. 1953;10:154–68.
Axelsson P, Johnsson R, Stromqvist B, Arvidsson M, Herrlin K. Posterolateral lumbar fusion. Outcome of 71 consecutive operations after 4 (2–7) years. Acta Orthop Scand. 1994;65:309–14.
Fritzell P, Hagg O, Wessberg P, Nordwall A. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine. 2002;27:1131–41.
Brislin B, Vaccaro AR. Advances in posterior lumbar interbody fusion. Orthop Clin N Am. 2002;33:367–74.
Lin PM, Cautilli RA, Joyce MF. Posterior lumbar interbody fusion. Clin Orthop Relat Res. 1983;180:154–68.
Lin PM. Posterior lumbar interbody fusion (PLIF): past, present, and future. Clin Neurosurg. 2000;47:470–82.
Hacker RJ. Comparison of interbody fusion approaches for disabling low back pain. Spine. 1997;22:660–5 (discussion 665–6).
Agazzi S, Reverdin A, May D. Posterior lumbar interbody fusion with cages: an independent review of 71 cases. J Neurosurg. 1999;91(2 Suppl):186–92.
Kotil K, Ali Akçetin M, Savaş Y. Clinical and radiologic outcomes of TLIF applications with or without pedicle screw: a double center prospective pilot comparative study. J Spinal Disord Tech. 2013;26:359–66.
Ivanov AA, Faizan A, Ebraheim NA, Yeasting R, Goel VK. The effect of removing the lateral part of the pars interarticularis on stress distribution at the neural arch in lumbar foraminal microdecompression at L3–L4 and L4–L5: anatomic and finite element investigations. Spine. 2007;32:2462–6.
Tender GC, Baratta RV, Voorhies RM. Unilateral removal of pars interarticularis. J Neurosurg Spine. 2005;2:279–88.
Hanley EN, Shapiro DE. The development of low back pain after excision of a lumbar disc. J Bone Joint Surg Am. 1989;71:719–21.
Spengler DM. Results with limited excision and selective foraminotomy. Spine. 1982;7:604–7.
Barr JS, Kubik GS, Molloy MK, et al. Evaluation of end results in treatment of ruptured lumbar intervertebral discs with protrusion of nucleus pulposus. Surg Gynecol Obstet. 1967;125:250–6.
Frymoyer JW, Hanley EN, Howe J. Disc excision and spine fusion in the management of lumbar disc disease: a minimum ten-year follow-up. Spine. 1978;3:1–6.
Naylor A. Late results of laminectomy for lumbar disc prolapse. A review after ten to twenty-five years. J Bone Joint Surg Br. 1974;56:17–29.
Salenius P, Laurent LE. Results of operative treatment of lumbar disc herniation. A survey of 886 patients. Acta Orthop Scand. 1977;48:630–4.
Kotilainen E. Long-term outcome of suffering from clinical instability after microsurgical treatment of lumbar disc herniation. Acta Neurochir. 1998;140:120–5.
Nachlas IW. End-results study of treatment of herniated nucleus pulposus by excision with fusion and without fusion. J Bone Joint Surg Am. 1952;34:981–8.
Vaughan PA, Malcolm BW, Maistelli GL. Results of L4–L5 disc excision alone versus disc excision and fusion. Spine. 1988;13:690–5.
Takeshima T, Kambara K, Miyata S, et al. Clinical and radiographic evaluation of disc excision for lumbar disc herniation with and without posterolateral fusion. Spine. 2000;25:450–6.
Caldwell OA, Sheppard WB. Criteria for spine fusion following removal of a protruded nucleus pulposus. J Bone Joint Surg Am. 1948;30:971–80.
Eie N. Comparison of the results in patients operated upon for ruptured lumbar discs with and without spinal fusion. Acta Neurochir. 1978;41:107–13.
Rish BL. A comparative evaluation of posterior lumbar interbody fusion for disc disease. Spine. 1985;10:855–7.
Tominaga S, Date K, Ouchi K, et al. Comparison between nonfusion and fusion group for lumbar discopathy—effects of intervertebral fusion. Rinshou Seikei Geka. 1988;23:236–46 (Japanese).
Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine. 1997;22:210–9 (discussion 219–20).
Brantigan JW, Steffee AD, Geiger JM. A carbon fiber implant to aid interbody lumbar fusion. Mechan Test Spine. 1991;16(6 Suppl):277–82.
Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: preliminary clinical results. J Neurosurg. 2002;97(1 Suppl):7–12.
Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993;18:575–81.
Shirado O, Zdeblick T, McAfee P, Warden KE. Biomechanical Evaluation of posterior stabilization of the spine and posterior Lumbar interbody arthrodesis for Lumbosacral Isthmic spondylolisthesis. A calf spine model. J Bone Joint Surg Am. 1991;73:518–26.
Bhatia NN, Lee KH, Bui CN, Luna M, Wahba GM, Lee TQ. Biomechanical evaluation of an expandable cage in single segment posterior lumbar interbody fusion. Spine. 2012;37:E79-85.
Blume HG. Unilateral posterior lumbar interbody fusion: simplified dowel technique. Clin Orthop Relat Res. 1985;193:75–84.
Zhao J, Hai Y, Ordway NR, Park CK, Yuan HA. Posterior lumbar interbody fusion using posterolateral placement of a single cylindrical threaded cage. Spine. 2000;25:425–30.
Zhao J, Wang X, Hou T, He S. One versus two BAK fusion cages in posterior lumbar interbody fusion to L4–L5 degenerative spondylolisthesis: a randomized, controlled prospective study in 25 patients with minimum two-year follow-up. Spine. 2002;27:2753–7.
Abumi K, Panjabi MM, Kramer KM, Duranceau J, Oxland T, Crisco JJ. Biomechanical evaluation of lumbar spinal stability after graded facetectomies. Spine. 1990;15:1142–7.
Turner JA, Ersek M, Herron L, Haselkorn J, Kent D, Ciol MA, et al. Patient outcomes after lumbar spinal fusions. JAMA. 1992;268:907–11.
Brantigan JW, Steffee AD, Lewis ML, Quinn LM, Persenaire JM. Lumbar interbody fusion using the Brantigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system: two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine. 2000;25:1437–46.
Freeman BJ, Licina P, Mehdian SH. Posterior lumbar interbody fusion combined with instrumented posterolateral fusion: 5-year results in 60 patients. Eur Spine J. 2000;9:42–69 (discussion 40).
Commarmond J. One-segment interbody lumbar arthrodesis using impacted cages: posterior unilateral approach versus posterior bilateral approach. Rev Chir Orthop Reparatrice Appar Mot. 2001;87:129–34.
Ames CP, Acosta FL Jr, Chi J, Iyengar J, Muiru W, Acaroglu E, et al. Biomechanical comparison of posterior lumbar interbody fusion and transforaminal lumbar interbody fusion performed at 1 and 2 levels. Spine. 2005;30:E562–6.
Sasso RC, Shively KD, Reilly TM. Transvertebral transsacral strut grafting for high-grade isthmic spondylolisthesis L5–S1 with fibular allograft. J Spinal Disord Tech. 2008;21:328–33.
Goh JC, Wong HK, Thambyah A, Yu CS. Influence of PLIF cage size on lumbar spine stability. Spine. 2000;25:35.
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine. 2004;29:1938–44.
Soh J, Lee JC, Shin BJ. Analysis of risk factors for adjacent segment degeneration occurring more than 5 years after fusion with pedicle screw fixation for degenerative lumbar spine. Asian Spine J. 2013;7:273–81. https://doi.org/10.4184/asj.2013.7.4.273.
Ninomiya K, Iwatsuki K, Ohnishi Y, Ohkawa T, Yoshimine T. Adjacent lumbar disc herniation after lumbar short spinal fusion. Case Rep Orthop. 2014;2014: 456940. https://doi.org/10.1155/2014/456940.
Young HH, Love GJ. End results of removal of protruded lumbar intervertebral discs with and without fusion. Am Acad Orthop Surg Inst Course Lect. 1959;16:213–6.
Vadapalli S, Sairyo K, Goel VK, et al. Biomechanical rationale for using polyetheretherketone (PEEK) spacers for lumbar interbody fusion—a finite element study. Spine. 2006;31:E992–8.
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
AGE carried out the clinical practice, surgical practice, data collection and analysis and contributed in writing the paper. YBE designed the study frame work, contributed in the writing process and editing. OSS contributed in the clinical practice, surgical practice, analyzing and presenting data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the faculty of medicine, Menoufia University. The Institutional Review Board (IRB) approval number and date; Neus 6, 10/2022.
Consent for publications
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elnaggar, A.G., Elsisi, Y.B. & Shereef, O.S. Posterior lumbar interbody fusion using single PEEK cage without pedicle screw fixation for lumbar disc herniation; Initial experience in Menoufia University Hospital. Egypt J Neurosurg 39, 2 (2024). https://doi.org/10.1186/s41984-023-00262-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-023-00262-5