Abstract
Introduction
Traumatic brain injuries (TBIs) are among the leading causes of death and disability in younger age groups. Current guidelines to prevent infection in compound depressed fractures of the skull recommend fragment removal and debridement, and the cranial defect usually is left for a secondary cranioplasty. However, recent studies demonstrated no difference in infection rates between primary and secondary reconstruction. Herein we point out our preliminary experience using a single-staged approach to surgical management of open depressed skull fractures.
Methods
This study included 72 patients between Egypt and Saudi Arabia with compound depressed fractures of the skull that underwent primary cranioplasty either by elevation or by titanium reconstruction within the first 72 h post-traumatic brain injuries. We report surgery-specific characteristics and overall complications over a 12-month follow-up period.
Results
Fifty-nine (82%) immediate primary cranioplasty patients were without complications. Twelve complications were seen in twelve patients. Infection accounted for only 2.8%, while the rest consisted of convulsions (6.9%), CSF rhinorrhea (4.2%), CSF leak, seroma, and re-operation (1.4%) each. One patient died after 20 postoperative days due to pulmonary embolism.
Conclusion
Neurosurgical expertise and readily available medical facilities within the civilian populations have significantly changed the traditional approach in calvarial CDF patients within the first 72 h post-trauma, where primary cranioplasty has proven to be a valid procedure with minimal morbidities compared to the traditional two-stage protocol.
Similar content being viewed by others
Introduction
Traumatic brain injuries (TBIs) are among the leading causes of death and disability in younger age groups. TBIs range from 67 to 317 in every 100,000 people, with a mortality rate of 4–8% in moderate head injuries and up to 50% in severe head injuries [1, 2]. TBIs include skull fractures (linear and depressed fractures), hematomas (subdural, epidural, intracerebral hematomas, and cerebral contusions), and diffuse brain injuries (concussion, diffuse axonal injury, and brain edema).
Depressed skull fractures may complicate up to 6% of TBIs, 90% of which are compound depressed fractures (CDF), where an open wound traverses the overlying skin and galea layers [3,4,5]. Surgical intervention has long been adopted for these injuries; however, CDFs are associated with an infection rate of 1.9–10.6% [5, 6].
Current guidelines to prevent infection in CDF cases recommend bone fragment removal, copious wound irrigation, and debridement in the primary setting, with the cranial defect usually left for the secondary cranioplasty procedure [4, 7]. The main reason for the delayed reconstruction was to reduce the rate of infection-related complications, such as osteomyelitis, meningitis, empyema, and brain abscess.
However, ongoing studies demonstrated no difference in infection rates between the primary and secondary reconstruction of CDFs, either with bone fragments or with synthetic implants, that primary cranioplasty is now considered a suitable surgical option with potential benefits in cost-effectiveness, safety, and cosmetic patient satisfaction [8,9,10,11,12].
Members of the Neurosurgery departments conducted this study at two different institutes within the middle east, namely, Ain Shams University Hospitals (ASUH), Cairo, Egypt, and Prince Mohamed Ibn Abdelaziz Hospital (PMAH), Riyadh, KSA, to evaluate the surgical outcome and rate of infection of the patients with calvarial CDFs that underwent primary cranioplasty either using autologous bone fragment replacement or using synthetic implants within 72 h of the injury. Herein we point out our preliminary experience using a single-staged approach to surgical management of open depressed skull fractures.
Patients and methods
Data collection
After receiving institutional review board approval from the Ethics Committee of scientific research, Faculty of Medicine, Ain Shams University, the authors of this study retrospectively analyzed the medical records and radiological images of 72 patients from January 2018 to December 2021. We included patients eligible for single-stage reconstruction for calvarial CDFs within 72 h of a TBI. We excluded patients with gunshot wounds, deeply comatosed on admission, or patients presenting more than 72 h post-trauma. All patients were operated on in the institutes mentioned above. Patients' records included demographic data (sex and age distribution), cause of injury, the elapsed time from injury to admission, location of CDFs, time from admission to surgery, Glasgow coma scale (GCS) on admission and discharge, and total hospital stay were all collected and analyzed. The primary investigation was the infection rate through clinical and lab assessment, while secondary investigations were associated with the intraoperative events, including the presence of a dural tear, the surgical procedure applied and type of repair, and the postoperative period of intravenous antibiotic administration and overall sequelae. All patients were followed over 12 months after discharge. The follow-up included clinical and radiological assessment in the form of labs and brain computed tomographic (CT) scans.
Technical aspects
All patients with CDFs had prophylactic broad-spectrum intravenous antibiotics half an hour before the initial surgical incision for SSI prophylaxis. With patients under general anesthesia and their heads positioned on a rolled doughnut, the hair around the laceration was shaved, followed by scrubbing with 7.5% povidone-iodine and draping. When technically appropriate, the scalp flap was fashioned to include laceration; otherwise, the surgeon chose different cranial skin flaps on an individual patient basis (Bicoronal scalp flap for fractures on the forehead, trauma flap for temporal or frontotemporal fractures).
The dissection plane was through the relatively avascular loose areolar layer. The pericranial flaps were designed separately over the skull fracture, followed by copious gentamicin irrigation of wounds. The depressed bone fragments were elevated and, if intended for use, were soaked in a povidone-iodine solution of 10% for 5 min. Dural tears were repaired by the neurosurgeon either primarily or patched by dural grafts after debridement of any exposed, lacerated, or contused brain tissue. After dural closure, if soiled, the bone defect was usually decontaminated by diluted hydrogen peroxide-soaked gauze pads.
Whenever the elevated bone fragments were large enough to cover the skull defect, autologous primary cranioplasty was performed, fixing the pieces with titanium mini plates and screws if available or vicryl 0 sutures instead. However, we used 0.6-mm-thick titanium mesh plates for the cranioplasty in cases with multiple fragmentation or comminution. In frontal sinus posterior wall fractures, sinus cranialization and packing of the nasofrontal duct with muscle and fascia were performed before reconstruction. The cranioplasty site was covered by the designated pericranial flap before skin closure with staples or sutures.
Postoperative phase
Intravenous broad-spectrum antibiotics were continued for 3–7 days postoperative depending on the case, as per hospital protocol. Triple antibiotic therapy using metronidazole was used in patients with frontal sinus involvement. Lab investigations included a blood picture, and inflammatory mediators were routinely done postoperatively for all patients. Radiographic follow-up computed tomography (CT) head was done for all patients immediately postoperative, after 1 month, and again at 6 months postoperatively. Clinical follow-up protocol of all patients was done in the outpatient clinic setting weekly in the first month, every 2 weeks for 2 months, and then monthly for 12 months after surgery (ranging from 12 to 37 months).
Statistical analysis
Categorical data are presented as absolute values and percentages, continuous, normally distributed data as means and standard deviations (SD), while time intervals are presented as medians and interquartile ranges (IQR). A p value ≤ 0.05 was considered statistically significant. Data analysis was performed using Social Science Statistics (SSS).
Results
This retrospective study included the clinical and radiological records of 72 skull CDFs patients that had the chance to undergo primary cranioplasty in the same session of depressed bone elevation between January 2018 and December 2021. Forty-six (63.9%) patients were included from ASUH, while 26 (36.1%) patients were from PMAH.
Demographic data
Table 1 lists a detailed summary of patient-specific factors. The average age at immediate cranioplasty was 25.8 ± 13.8 years (range 2–71), with more than half the sample (51.4%) within the 20–40 age group. A male predominance (90.3% male) was observed in ASUH and PMAH patients. No statically significant difference was detected regarding patient characteristics between the two institutes.
Trauma and clinical presentation
Direct head trauma -DHT- (physical assault, interpersonal violence or falling objects) (n = 45, 62.5%) was the most common mode of trauma in our patient population, followed by road traffic accidents -RTA- (n = 21, 29.2%), while falling from height -FFH- came last in etiology (n = 6, 8.3%) (Table 2). There was no statistically significant difference between ASUH and PMAH regarding etiology.
Initial admission Glasgow Coma Score ranged from 6 to 15, (mean = 13.9 ± 1.9) with lower admission scores seen in PMAH with no statistically significant difference (Table 1). The time from trauma to surgery ranged from 2 to 72 h, with a median duration of 9 h (IQR 6–20). Fifty-nine patients were operated on within 24 h of the trauma, while 13 were operated after 24 h due to delayed presentation to the ER. However, none exceeded 72 h. We found a significant difference (p value = 0.014) in admission—OR interval between both institutes due to a lengthier booking system in PMAH (Table 1).
Fracture site and associated injuries
Thirty (41.7%) cases had a CDF located on the left side, twenty-eight (38.9%) located on the right side and 14 (19.4%) cases were bilateral. The frontal sinus was violated in six (8.3%) cases, three of which had preoperative CSF rhinorrhea while two fractures (2.7%) extended to involve the orbital roof. (Table 1) We found cerebral contusion to be the most associated injury involving 24 (33.3%) cases. Initial CT findings showed different-sized epidural hemorrhages in 12 (16%) patients and superior sagittal sinus violation in three (4.2%) cases; two of whom presented with motor weakness. Dural violation was found in 37 (51.4%) (Table 2).
Surgery-specific characteristics
Regarding the surgeries, 38 (52.8%) cases had the chance of reconstruction with either mini plates (n = 23) or titanium meshes (n = 15) (Fig. 1), with a statistically significant difference (p value < 0.00001) for PMAH in synthetic reconstruction. In the remaining 34 (47.2%) cases, we replaced the fractured bone fragments and fixed them by impaction or sutures as suitable (Table 3). Associated dural tears were all repaired either directly or with peri-cranial grafts. Epidural and cerebral contusions were evacuated whenever required.
A of a 38-year-old male patient admitted with a direct head trauma in the workplace. a 3D Ct showing a frontal CDF. b Axial cut brain CT showing a right extradural hematoma. c Intraoperative clinical picture of titanium mesh cranioplasty. d Postoperative axial cut CT bone window with adequate contour. e Postoperative CT brain showing evacuated hematoma
Outcomes
The postoperative hospital stay had a median duration of 6 days (IQR 5–7.5). Prolonged stays (≥ 2 weeks) were observed in only five patients; three of whom had low GCS on admission, another suffered hemiplegia and is currently on steady physiotherapy sessions, and the fifth died after 20 days due to pulmonary embolism.
Regarding the Glasgow Coma Scale, 44 patients were 15/15 preoperatively and remained the same post-surgery. The remaining 28 patients were initially graded as mild (n = 18) 13–14, moderate (n = 6) 9–12 and severe (n = 3) 3–8, who eventually all improved except three patients that remained the same and one patient that died as mentioned above, making the total number of patients to be discharged with a GCS 15, sixty-five patients (90.3%), five (7%) with a GCS 14, and one (2.7%) with a GCS 11.
Complications
Fifty-nine (82%) immediate primary cranioplasty patients were without any complications. Twelve complications were seen in twelve patients. Complications (18%) consisted of only two infection cases (2.5%) together with convulsions (n = 5), CSF leak (n = 4), seroma (n = 1), and re-operation (n = 1).
Infection
The two infection cases (2.5%) presented postoperatively with brain abscesses. The first case had a penetrating initial injury caused by a sharp object causing brain contusions and a dural tear and was operated on, only four hours post the insult and received triple ABS for 1 week, and the patient was discharged. However, a follow-up CT done after 2 weeks revealed an abscess at the surgical bed. Surgical abscess drainage was done followed by intravenous antibiotics for 6 weeks. The second case (Fig. 2) initially presented with SAH and brain contusions with a 13 GCS on admission. This patient improved markedly after the primary cranioplasty; however, 2 months later, the patient suffered a continuous headache, and upon investigation, we detected a brain abscess at the surgical bed. The decision was made to remove the hardware with surgical debridement and follow a 6-week intravenous antibiotics course. A second cranioplasty was done later, and the patient has been asymptomatic throughout a 2-year follow-up period. Both these cases had deeply indriven soiled bone fragments.
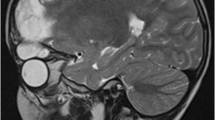
A 29-year-old male patient that presented with a left frontoparietal CDF after a motor vehicle accident (a), that was treated with a craniotomy and primary immediate titanium mesh cranioplasty (b). Two months later the patient complained of an ongoing headache, where a brain MRI revealed a brain abscess (c). Debridement and hardware removal was done (d) followed by 6 weeks of antibiotics. One year later, another titanium mesh cranioplasty was done after the infection subsided (e–f)
Overall complications
Convulsions consisted of only a single attack postoperatively and were controlled by antiepileptic drugs with no recurrent attacks. CSF leakage was observed from the wound of a single patient and as persistent rhinorrhea in three of the cases with frontal sinus involvement, all of whom responded to conservative management with total cessation after 3 days. Postoperative subcutaneous seroma formation was observed in only one case and resolved entirely with no recollection after tapping. Finally, one case had to be returned to the operating room on the second postoperative day as missed bone fragments were discovered in the postoperative CT.
Discussion
Most of the previous studies shunning early repair of skull CDFs were based on war injuries, which differ significantly from those in a civilian population where early diagnosis, availability of neurosurgical facilities, and the prompt debridement of fractures in the early hours post-trauma play as significant factors in reducing the anticipated co-morbidities [12, 13]. Comparing our demographic data with the series done by Miller and Jennett [14], Braakman [3], and Wylen et al. [5] reveals a remarkable similarity in the preponderance of young patients (average = 25.8 years), with a striking predominance of male cases (90.3%), violation of dura matter in more than half the sample (51.4%) and the average admission GCS (13.9). Similarly, direct head trauma (62.5%) as an etiology was noted in our study to be in accordance with the Ceylon series of Cabraai and Abeysuriya [15], in which assaults caused 50% of cases.
In this study, 82% of patients were operated on within the first 24 h post-trauma, comparable to the percentage described by Wylen et al. [5]. However, we found a statistically significant difference in OR admission time between the two institutes owing to the lengthier booking system in PMAH, which resulted in patients taking longer to go to the OR. Preoperative CTs delineated cerebral contusions as the most commonly associated injury with CDFs, (33.3%), which was lower than that reported by Oktay et al. (42%) [16]; however this value was higher than Wylen et al. (19%) [5].
Our way of handling patients with CDFs has gradually changed in the last decade. The traditional approach was to remove bone fragments, debride the wound, and treat the intracranial pathologic findings, leaving a cranial defect to be repaired later, with infection being the primary clinical concern. However, this study included 72 CDF patients across two prominent institutes in the middle east treated by immediate cranioplasty either through replacing the original bone fragments or by using a mini mesh. Only two cases (2.8%) developed a postoperative infection due to deeply seated indriven bone fragments from the primary trauma, with only one of them necessitating removal of hardware and undergoing a secondary cranioplasty in a delayed fashion, while the other responded to systemic ABS and tapping. This result confirms earlier findings by Kriss et al. [17] who reported two infection (2.5%) instances after immediately treating 79 CDF patients.
Epilepsy presented in 6.9% of our patient population, which is lower than that observed by the Glasgow series [14] (18.7%) and Braakman [3] (11.5%), and all five patients were controlled on antiepileptics and developed no further fits after their single attack. Similarly, cases with persistent CSF rhinorrhea had frontal sinus and orbital roof fractures in the initial presentation which resolved without a lumbar drain. Our postoperative hospital stays matched that of Marbacher et al. [7] in being under 2 weeks for most cases.
The primary rationale for attempting primary cranioplasty of skull CDFs is the potential benefit of protecting the brain from the altered electroencephalographic environment that a cranial defect imposes [18, 19]. Delayed cranioplasty patients often suffer from headaches, epilepsy, sinking skull flap syndromes, or even paradoxical brain herniation [19,20,21]. From our experience, the procedure of early reconstruction is technically easier than delayed reconstruction and is associated with a very low infection rate while avoiding issues like soft tissue contracture and scar plats and altogether reduces the financial burden on the patient and on the health care system. We prefer this treatment protocol to the classical approach and encourage wider multicenter long-term studies to validate these outcomes further.
Conclusion
Neurosurgical expertise and readily available medical facilities within the civilian populations has significantly changed the traditional approach in calvarial CDF patients within the first 72 h post-trauma where primary cranioplasty has proven to be a valid procedure with minimal morbidities compared to the traditional two stage protocol.
Abbreviations
- TBI:
-
Traumatic brain injury
- ASUH:
-
Ain Shams University Hospital
- PMAH:
-
Prince Mohamed Ibn Abdelaziz Hospital
- CDF:
-
Compound depressed fracture
- CT:
-
Computed tomography
- CSF:
-
Cerebrospinal fluid
- GCS:
-
Glasgow coma scale
- DHT:
-
Direct head trauma
- RTA:
-
Road traffic accident
- FFH:
-
Fall from height
- SSI:
-
Surgical site infection
- EDH:
-
Extradural hematoma
- SSS:
-
Superior sagittal sinus
- SDH:
-
Subdural hematoma
- SAH:
-
Subarachnoid hemorrhage
References
Ghajar J. Traumatic brain injury. Lancet. 2000;356(9233):923–9.
Schouten JW, Maas AI. Epidemiology of traumatic brain injury. In: Winn HR, editor. You- man’s Neurological Surgery. Volume 4. 6th ed. Philadelphia: Saunders; 2012. p. 3270–6.
Braakman R. Depressed skull fracture: data, treatment, and follow-up in 225 consecutive cases. J Neurol Neurosurg Psychiatry. 1972;35:395–402.
Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, et al. Surgical management of depressed cranial fractures. Neurosurgery. 2006;58(3 Suppl):S56–60 (discussion Si-Siv).
Wylen EL, Willis BK, Nanda A. Infection rate with replacement of bone fragment in compound depressed skull fractures. Surg Neurol. 1999;51:452–7.
Jennett B, Miller JD. Infection after depressed fracture of skull. Implications for management of nonmissile injuries. J Neurosurg. 1972;36:333–9.
Marbacher, et al. Primary reconstruction of open depressed skull fractures with titanium mesh. J Craniofac Surg. 2008;19:490–5.
Ehrlich G, Kindling S, Wenz H, Hänggi D, Schulte DM, Schmiedek P, et al. Immediate titanium mesh implantation for patients with postcrani otomy neurosurgical site infections: safe and aesthetic alternative procedure? World Neurosurg. 2017;99:491–9.
Prakash A, Harsh V, Gupta U, Kumar J, Kumar A. Depressed fractures of skull: an institutional series of 453 patients and brief review of literature. Asian J Neurosurg. 2018;13:222–6.
AbdelFatah MA. Management of bone fragments in nonmissile compound depressed skull fractures. Acta Neurochir. 2016;158:2341–5.
Outcome of Primary Bone Fragment Replacement in Pediatric Patients with Depressed Skull Fracture Kadir Oktaya Ebru Guzelb Emre Unalc Tevfik Yilmazd Ali Ihsan Oktene Aslan Guzela, c Pediatr Neurosurg DOI: https://doi.org/10.1159/000495807
Sande GM, Galbraith SL, McLatchie G. infection after depressed fracture in the West of Scotland. Scott Moo J. 1980;25:227–9.
Meirowsky AM. Compound fractures of the convexity of the skull. In: Coates JB, Meirowsky AM, eds. Neurological Surgery of Trauma. Washington, DC: US Govt. Printing Office 1965
Jennett, B., and Miller, D. Infection after depressed fracture of skull. J Neurosurg. 1971.
Cabraal SA, Abeysuriya SC. The management of compound depressed fractures of the skull. Ceylon Med J. 1969;14:105–15.
Oktay et al. Outcome of primary bone fragment replacement in pediatric patients with depressed skull fracture. Pediatr Neurosurg 2019.
Kriss FC, Taren JA, Kahn EA. Primary repair of compound skull fractures by replacement of bone fragments. J Neurosurg. 1969;30:698–702.
Aydin S, Kucukyuruk B, Abuzayed B, Sanus GZ. Cranioplasty: review of materials and techniques. J Neurosci Rural Pract. 2011;2(2):162–7.
Zegers T, Ter Laak-Poort M, Koper D, Lethaus B, Kessler P. The therapeutic effect of patient-specific implants in cranioplasty. J Craniomaxillofac Surg. 2017;45(1):82–6.
Kurland DB, Khaladj-Ghom A, Stokum JA, Carusillo B, Karimy JK, Gerzanich V, Sahuquillo J, Simard JM. Complications associated with decompressive craniectomy: a systematic review. Neurocrit Care. 2015;23(2):292–304.
Ramakrishnan V, Dahlin R, Hariri O, Quadri SA, Farr S, Miulli D, Siddiqi J. Anti-epileptic prophylaxis in traumatic brain injury: a retrospective analysis of patients undergoing craniotomy versus decompressive craniectomy. Surg Neurol Int. 2015;6:8.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The database used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
H.E. and M.M.A. are the principal neurosurgeons in the study and follow up of patients. A.M.E.—Data collection. M.S.K.A.—Data collection and writing and revision of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research received institutional review board approval from the Ethics committee of scientific research, Faculty of Medicine, Ain Shams University. (FMASU R 93 / 2022).
Consent for publication
Not applicable.
Competing interests
All the authors declare no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elsabaa, A.M., Eldawoody, H., Abdelwahed, M.S.K. et al. Primary cranioplasty for calvarial compound depressed fractures; 2 centers experience. Egypt J Neurosurg 38, 50 (2023). https://doi.org/10.1186/s41984-023-00235-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-023-00235-8