Abstract
Background
Although it is well known that performing decompressive craniectomy (DC) in cases of swollen middle cerebral artery infarction (SMCAI) improves patient outcomes, limited evidence presently exists on the likelihood of mortality and achieving functional outcome following DC. The aim of the present study was to identify the predictors of early in-hospital mortality and functional status six months after performing DC in a cohort of patients with SMCAI.
Material and methods
All patients that had suffered SMCAI and underwent DC were included in the study sample and their demographic information, along with clinical and radiological findings, and risk factors were recorded for further analyses, which were conducted using the commercial software STATA. Modified Rankin Scale score (mRS) served as an outcome measure at 6-month follow-up.
Results
DC was performed on 50 patients with SMCAI (72% of whom had left hemisphere infractions) aged 45.2 ± 10.2 years (range 24–67 years), 32 (64%) of whom were female and 18 (36%) were male. While the initial median Glasgow Coma Scale (GCS) score was 8 (range 4–13), clinical deterioration mostly occurred within the first five days, whereby DC was performed within 9 ± 7.2 h (range 2–36 h). Following surgery, 16 (32%) patients died while in hospital, whereas the remaining 34 were discharged after 135 days on average, and attended the 6-month follow-up, when the median mRS score of 3 (range 2–6) was recorded for this subsample.
Conclusions
Younger age, higher GCS score, presence of isochoric pupils, history of prior treatment (e.g., embolectomy or tissue plasminogen activator), and shorter interval between clinical deterioration and surgery are associated with a lower likelihood of mortality and a greater odd of a favorable functional outcome.
Similar content being viewed by others
Introduction
Stroke is posited to be the second leading cause of death worldwide following Cerebrovascular disease [1] and is of ischemic type in 85% of cases, whereby 50% of these strokes occur along the middle cerebral artery (MCA). Approximately 10–15% of the patients that suffer MCA infarction (MCAI) will develop intracranial hypertension and malignant cerebral edema (MCE), leading to swollen middle cerebral artery infarction (SMCAI), which is associated with high mortality rates [2, 3]. In this type of stroke, the onset of Malignant cerebral edema (MCE) is usually occurs within 2–5 days [4, 5] and is fatal in about 80% of cases despite optimal intensive care treatment [6,7,8]. Empirical evidence, however, indicates that when decompressive craniectomy (DC) is performed as soon patients’ condition starts to deteriorate, survival rates and functional outcomes can be improved. Theodor Kocher was the first to record surgical intervention aimed at relieving the intracranial pressure. While in 1901 Kocher recommended surgical trepanation in all cases of intracranial hypertension, this advice was related to traumatic brain injury (TBI), given that at the time ischemic stroke and the associated malignant edema were poorly understood. As a result, it took more than five decades for DC to be performed on a patient that had suffered ischemic stroke [9]. Since then, numerous studies on the effectiveness of DC in such cases have been conducted, including three European randomized controlled trials [10, 11] while the initial findings indicated that DC improves survival, a follow-up pooled analysis of the findings yielded by these trials revealed 22% mortality rate even with surgery [12]. As this procedure is now widely implemented, the factors that might contribute to post-DC mortality and different functional outcomes must be better understood, as this would facilitate the decision-making regarding treatment. For example, older age, and midline shift have been proposed as potential predictors of early mortality following SMCAI [13, 14]. Time from stroke onset to decompressive craniectomy and the degree of preoperative neurological impairment assessed using the National Institutes of Health Stroke Scale (NIHSS) [15] have also been shown to facilitate more accurate patient prognosis [10, 13, 16]. However, these results are based on individual investigations and cannot be generalized beyond the settings in which they were obtained [17]. Therefore, further research to evaluate the influence of vascular involvement, brain locality, or clinical neurological status prior to DC is warranted. The present study aims to contribute to this body of knowledge by examining the demographic, clinical, and radiological findings of patients with SMCAI that underwent DC as the potential determinants of early mortality and functional outcome at 6-month follow-up.
Materials and methods
This retrospective cohort study included 50 patients who were admitted to the neurology and/or neurosurgery department at Prince Mohammed Bin Abdulaziz Hospital, Kingdom Hospital, and Saudi German hospital at Riyadh, Saudi Arabia, between January 2017 and December 2020 due to SMCAI. The study sample was formed after excluding records of patients with GCS 3 and bilaterally dilated non-reactive pupils, patients with previous neurological deficits, and those with incomplete data. Upon admission, each of the 50 patients was treated with decompressive craniectomy (DC) while following the standard clinical pathway to ensure best medical treatment. To facilitate analyses, patients’ medical charts were reviewed, and age, gender, clinical status, and brain CT scan findings were recorded. As each individual was subjected to GCS assessment on admission, the GCS score was employed to capture clinical status, whereas the modified Rankin Scale (mRS) score served as a measure of functional status at 6-month follow-up, with mRS ≤ 3 indicating favorable outcome [18, 19]. Clinical records review further indicated that surgery was performed early (within 24 h from the diagnosis) in all patients with GCS < 13, in whom midline shift > 7 mm or contralateral ventricular dilatation was noted, while delayed surgery (after 24 h from the diagnosis) was performed if patient’s GCS declined by more than 2 points (when initial GCS at presentation was > 13) or when the midline shift increased above 10 mm. The time of stroke onset was obtained from the emergency medical services records while pre- and post-operative cerebral CT (performed using a multidetector scanner with coronal and sagittal reconstructions) was obtained from the department to which the patient was admitted. The images were assessed by a radiologist, neurologist and neurosurgeon to identify the size of infarction, contralateral ventriculomegaly, midline shift, and hemorrhagic infarction. As 16 patients died during the study period, only 34 were available for the follow-up, which was conducted on outpatient setting at the corresponding stroke clinic and neurosurgery departments at least six months after the DC. For all patents, age, gender, comorbidities (hypertension, heart disease, and diabetes mellitus), anisocoric pupils, and GCS before surgery, time from MCAI onset to DC, side of the lesion, contralateral ventriculomegaly, midline shift, and hemorrhagic infarction were recorded, along with previous treatment with tissue plasminogen activator and/or thrombectomy, and were considered as potential predictors of mortality.
Statistical analyses
The gathered patient data was subjected to statistical analyses utilizing the commercial software package STATA. Depending on the data type, mean ± standard deviation (SD) and/or median with interquartile ranges and proportions were calculated as appropriate. In order to determine the outcome predictors, we compared the mean, median, or proportion between the two groups comprising of surviving and deceased patients using t-test, chi-squared, Wilcoxon test, and Kruskal–Wallis rank test. For the correlation between the treatment and outcome variables, univariate logistic regression was conducted, whereby stratification and multivariate regression analyses were performed in order to eliminate any cofounder effects (a 2-sided p value < 0.05 was considered statistically significant).
Results
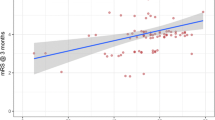
Our sample comprised of 50 patients with SMCAI that underwent DC, aged 45.2 ± 10.2 years (range 24–67 years), 32 (64%) of whom were female and 18 (36%) were male. While clinical deterioration from the onset of stroke was observed from Day 1 until Day 9, in most cases it took place during the first 5 days, with a median value of 3, as shown in Fig. 1. Following the deterioration, patients were taken into surgery within 2–36 h (with the mean of 9 ± 7.2 h). While the speech-dominant hemisphere (left side) was affected in 36 (72%) patients and in 20% of cases the pupils were isochoric, the most common vascular risk factors were hypertension (44%), diabetes mellitus (18%), and cardiac disease (12%). previous treatment with tissue-plasminogen activator was completed in (16%). The GCS at presentation ranged from 4 to 13 (with a median of 8), while the median mRS score was 3 (ranging from 2 to 6). As shown in Table 1, the most common surgery-related complications were sunken flap (18%), infection (16%), hydrocephalus (16%). Unfortunately, 16 (32%) patients died at the hospital 2.6 ± 1.6 days after decompressive craniectomy, leaving only 34 (68%) patients for the follow-up. When the surviving group’s characteristics were compared to those of the deceased patients, statistically significant difference in their age was noted, as the former were younger (42.9 ± 9.4 vs. 50.1 ± 10.4 years). Survival was also more likely if an individual had higher GCS, isochoric pupils, had received treatment previously, and was given surgical intervention within the first 24 h from the onset of clinical deterioration, as shown in Table 2. The correlations between prognostic factors and functional outcome after DC are reported in Table 3, indicating that older age, lower GCS, delayed intervention from deterioration, contralateral ventriculomegaly, diabetes mellitus, cardiac problems, postoperative sunken flap were the most reliable outcome predictors for poor functional outcome while younger age, higher GCS, and presence of isochoric pupils, were the most reliable outcome predictors for good functional status (Fig. 2), but multivariate logistic regression analysis of the statistically significant predictors in the univariate analysis led to fade out of this significance except for the GCS (Table 4). Over all favorable outcome was identified in 28 cases (56%), prognostic factors for prediction of favorable outcome are reported in Table 5 indicating that younger age, higher GCS, right side DC, early detection of deterioration, earlier intervention and early cranioplasty are reliable predictors for favorable outcome while older Patient with DM and/or cardiac diseases and lower GCS with delayed intervention is usually associated with unfavorable outcome. Figures 3 and 4 show cases example for the criteria of the patient with favorable and unfavorable outcome respectively.
Case 1: favourable outcome GOS 5 41 years old female patient known hypertensive on medications, came to the Emergency department with acute onset right side body weakness, headache and dizziness, on arrival to the hospital she was conscious with sensory dysphasia, the initial CT brain A revealed left T/P acute ischemic stroke with lower trunk left MCA territory distribution without midline shift, admitted under observation, on the 3rd day of her admission her GCS dropped to GCS 10, an urgent CT brain B revealed evolutional change at the infarction core with midline shift of about 5 mm, underwent emergency surgical decompressive craniectomy and duroplasty that was performed within 5 h from the time of deterioration and the patient was sent to ICU, on the second postoperative day patient weaned from ventilator, GCS 14, FU CTA brain was done (C, D) and revealed nice decompression. On the third POD, patient improved more and discharged from ICU and FU CT brain revealed lax brain at both one, two weeks PO (E, F), then Cranioplasty was performed after 19 days from DC, and post-cranioplasty follow up CT brain (G, H) showed no adverse effects and satisfactory reconstruction
Case 2: 55 years old female patient came to the Emergency department with acute onset left side body weakness, confused, the initial CT brain A revealed right acute ischemic stroke with lower trunk right MCA as well as small ACA territory distribution without midline shift, admitted under observation, on the 2nd day of her admission her GCS dropped to GCS 11, with unequal pupils an urgent CT brain B revealed evolutional change at the infarction core with midline shift of about 12 mm, underwent emergency surgical decompressive craniectomy and duroplasty that was performed within 2 h from the time of deterioration and the patient was sent to ICU, on the 2nd postoperative day he GCS 8t, FU CT brain was done (C, D, F) and revealed satisfactory decompression. After extubation her GCS was 11. FU CT brain revealed lax brain at two weeks PO (E), after two weeks patient developed left LL swelling and Doppler US revealed DVT, IVC filter G was inserted and started on anticoagulants, unfortunate she developed massive pulmonary embolism and passed away 18 days postoperatively
Discussion
Although DC surgery is frequently performed on patients with SMCAI, as it is believed that Decompressive craniectomy has an effective role in decreasing the mean intracranial pressure and may decrease mortality rates, and increase the favorable outcome [20] but the outcome is still uncertain, as many such individuals die within days following DC [12]. The benefits of DC with respect to improving patients’ functional status and quality of life (QoL) are also questionable, as there is limited information on the predictors of short-term mortality and functional status after DC Among other predicting factors, timing of surgery and preoperative clinical condition were evaluated where Early intervention and preoperative clinical condition, patients’ age, site of infarct, and preoperative midline shift had been evaluated [21]. In accordance with our results, an association between age and early death after DC for patients with SMCAI has been reported by several authors [4, 9, 19] while others countered these findings [15, 21]. It is also worth noting that, in a European study conducted by Jüttler and his colleagues [22], about 22% of SMCAI patients (many of whom were aged below 60) were deceased within 30 days following DC [10, 23, 24]. Similar findings were obtained in a North American setting by Frank Jeffrey and colleagues [25], who noted 21% mortality rate for their cohort (aged up to 75 years) while majority of our cases involved left side, we failed to establish a link between the impacted hemisphere [26] (dominant vs. non-dominant) and mortality or functional outcome. Our findings are in line with those yielded by several authors, including Gupta and colleagues [27]. They are also supported by the evidence yielded by the DESTINY [22], DECIMAL [11, 24], and HAMLET [10, 23, 24] trials, and also the Swedish malignant middle cerebral artery infarction study [28], indicating that the QoL and outcome are independent of hemisphere involvement.
Ample body of evidence indicates that preoperative GCS score is a reliable QoL predictor. Thus, as expected, in our study, the GCS score on admission was negatively correlated with functional impairment and was a significant predictor of early mortality. Other authors also suggested using the NIHSS score [10], whereby Kim and colleagues identified an NIHSS score > 18 on admission as an independent predictor of life-threatening brain swelling [29]. As isochoric pupils were also identified in our study as a significant survival predictor, we attribute this link to a more rapid intervention in such cases. However, we have failed to establish a link between the degree of midline shift at the time of DC and early mortality, even though this relationship was reported by Puetz and colleagues, who also noted that a postoperative midline shift of < 5 mm was associated with a favorable outcome [19]. Thus, given these discordant findings, it appears that the management plan needs to be determined for each individual SMCAI patient [18]. Nonetheless, a shorter interval between SMCAI onset and DC tends to improve survival as well as QoL [4, 6], as confirmed in our study. In accordance with this finding Refaat and Abdallah [21] had proven the role of early decompressive craniectomy in reduction of the mortality rate and improving functional outcome [21, 30].
Study limitations
The relatively small sample size precludes firm conclusions.
Conclusions
According to our retrospective study of 50 SMCAI patients that underwent DC, younger age, higher GCS, presence of isochoric pupils, and history of previous treatment (embolectomy or tissue plasminogen activator), as well as shorter interval between clinical deterioration and surgery, can be considered as predictive factors for greater survival and more favorable functional outcomes in this population.
Availability of data and materials
Data is available on requests.
Abbreviations
- DC:
-
Decompressive craniectomy
- SMCAI:
-
Swollen middle cerebral artery infarction
- mRS:
-
Modified Rankin Scale score
- GCS:
-
Glasgow Coma Scale score
- h:
-
Hours
- MCA:
-
Middle cerebral artery
- MCE:
-
Malignant cerebral edema
- TBI:
-
Traumatic brain injury
- MCAI:
-
Middle cerebral artery infarction
- NIHSS:
-
National Institutes of Health Stroke Scale
- CT:
-
Computerized tomography scan
- SD:
-
Standard deviation
- QoL:
-
Quality of life
- IRR:
-
Incidence rate ratio
References
Katan M, Luft A. Global burden of stroke. New York: Thieme Medical Publishers; 2018. p. 208–11.
Huttner HB, Schwab S. Malignant middle cerebral artery infarction: clinical characteristics, treatment strategies, and future perspectives. Lancet Neurol [Internet]. 2009;8(10):949–58. https://doi.org/10.1016/S1474-4422(09)70224-8.
Moulin DE, Lo R, Chiang J, Barnett H. Prognosis in middle cerebral artery occlusion. Stroke. 1985;16(2):282–4.
Sakai K, Iwahashi K, Terada K, Gohda Y, Sakurai M, Matsumoto Y. Outcome after external decompression cerebral infarction for massive. 1997.
Frank JI. Large hemispheric infarction, deterioration, and intracranial pressure. Neurology. 1995;45(7):1286–90.
Berrouschot J, Sterker M, Bettin S, Kiister J. Mortality of space-occupying (malignant) middle cerebral artery infarction under conservative intensive care. Intensive Care Med. 1998;24:620–3.
Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. Malignant middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 1996;53(4):309–15.
Rieke K, Schwab S, Krieger D, von Kummer R, Aschoff A, Schuchardt V, et al. Decompressive surgery in space-occupying hemispheric infarction: results of an open, prospective trial. Crit Care Med. 1995;23(9):1576–87.
Scarcella G. Encephalomalacia simulating the clinical and radiological aspects of brain tumors: a report of 6 cases. J Neurosurg. 1956;13(4):278–92.
Hofmeijer J, Kappelle LJ, Algra A, Amelink GJ, Van Gijn J, Van Der Worp HB. Surgical decompression for space-occupying cerebral infarction (the Hemicraniectomy After Middle Cerebral Artery infarction with Life-threatening Edema Trial [HAMLET]): a multicentre, open, randomised trial. Lancet Neurol [Internet]. 2009;8(4):326–33. https://doi.org/10.1016/S1474-4422(09)70047-X.
Vahedi K, Vicaut E, Mateo J, Kurtz A, Orabi M, Guichard J, et al. Sequential-design, multicenter, randomized, controlled trial of early decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL trial). Stroke. 2007;38(9):2506–17.
Lammy S, Al-Romhain B, Osborne L, St George EJ. 10-Year institutional retrospective case series of decompressive craniectomy for Malignant Middle Cerebral Artery Infarction (mMCAI). World Neurosurg. 2016;96:383–9.
Chen C, Cho D, Tsai S. Outcome and prognostic factors of decompressive hemicraniectomy in malignant middle cerebral artery infarction. J Chin Med Assoc [Internet]. 2007;70(2):56–60. https://doi.org/10.1016/S1726-4901(09)70302-8.
Mckenna A, Wilson CF, Caldwell SB, Curran D. Functional outcomes of decompressive hemicraniectomy following malignant middle cerebral artery infarctions: a systematic review. Br J Neurosurg. 2011;2012(26):310–5.
Brott T, Adams HP, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20:864–70.
Lam WWM, Leung TWH, Chu WCW, Yeung DTK, Wong LKS, Poon WS. Early computed tomography features in extensive middle cerebral artery territory infarct: prediction of survival. J Neurol Neurosurg Psychiatry. 2005;76:354–7.
Yu JW, Choi J, Kim D, Cha J, Huh J. Outcome following decompressive craniectomy for malignant middle cerebral artery infarction in patients older than 70 years old. J Cerebrovasc Endovasc Neurosurg. 2012;14(2):65–74.
Neugebauer H, Creutzfeldt CJ, Hemphill JC III, Heuschmann PU, Jüttler E. DESTINY-S: attitudes of physicians toward disability and treatment in malignant MCA infarction. Neurocrit Care. 2014;21:27–34.
Puetz V, Campos CR, Eliasziw M, Hill MD, Demchuk AM. Assessing the benefits of hemicraniectomy: what is a favourable outcome? Lancet Neurol. 2007;6:580.
Elsayed A, Elsayed A. Decompressive craniectomy in malignant hemispheric infarction: favorable outcome and disability. Egypt J Neurol Psychiatry Neurosurg. 2019;55(25):1–5.
Refaat M, Abdallah OY. Decompressive craniectomy in malignant middle cerebral artery infarctions: outcome of 25 cases. Egypt J Neurosurg. 2018;33(19):1–5.
Juttler E, Schwab S, Schmiedek P, Unterberg A, Hennerici M, Woitzik J, et al. Decompressive surgery for the treatment of malignant infarction of the middle cerebral artery (DESTINY). Stroke. 2007;38(9):2518–25.
Hofmeijer J, Amelink GJ, Algra A, Van Gijn J, Macleod MR, Kappelle LJ, et al. Hemicraniectomy after middle cerebral artery infarction with life-threatening Edema trial (HAMLET). Protocol for a randomised controlled trial of decompressive surgery in space-occupying hemispheric infarction. Trials. 2006;7:1–7.
Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol. 2006;6:215–22.
Frank JI, Schumm LP, Wroblewski K, Chyatte D, Rosengart A, Kordeck C, et al. Hemicraniectomy and Durotomy Upon Deterioration From Infarction-Related Swelling Trial (HeADDFIRST): a randomized pilot clinical trial. Stroke. 2015;45(3):781–7.
Schneck MJ. Hemicraniectomy for hemispheric infarction and the HAMLET study: a sequel is needed. Lancet Neurol. 2009;8(4):303–4.
Gupta R, Connolly ES, Mayer S, Elkind MSV. Hemicraniectomy for massive middle cerebral artery territory infarction a systematic review. Stroke. 2004;35:539–44.
Malm J, Bergenheim A, Enblad P, Hardemark HG, Koskinen L-OD, Naredi S, et al. The Swedish Malignant Middle cerebral artery infarction study: long-term results from a prospective study of hemicraniectomy combined with standardized neurointensive care. Acta Neurol Scand. 2006;113(3):25–30.
Kim H, Tak S, Woo Y, Rim S, Seong I, Wook K. Predictors of malignant brain edema in middle cerebral artery infarction observed on CT angiography. J Clin Neurosci [Internet]. 2015;22(3):554–60. https://doi.org/10.1016/j.jocn.2014.08.021.
Paliwal P, Kazmi F, Bao MBB, Teoh HL, Yeo LLL, Seet RCS, et al. Early decompressive hemicraniectomy for malignant middle cerebral artery infarction in asian patients: a single centre study. World Neurosurg [Internet]. 2017. https://doi.org/10.1016/j.wneu.2017.12.157.
Acknowledgements
Not applicable.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
SA: Conception and design of the work, Data collection, Data analysis and interpretation, Drafting the article Manuscript editing and review. MB: Literature search, Manuscript preparation, Manuscript editing and review, Critical revision. MMT: Critical revision. ME: Literature search, Manuscript editing and review. AE: Literature search, Manuscript editing. MH: Literature search. SE: Literature search. HE: Data acquisition, Data analysis and interpretation.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (Kingdom hospital ethical committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
For this type of study formal consent is not required.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abouhashem, S., Bafaquh, M., Assem, A. et al. Functional outcome and mortality prediction after decompressive craniectomy in patients with malignant middle cerebral artery infarction. Egypt J Neurosurg 38, 51 (2023). https://doi.org/10.1186/s41984-023-00232-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-023-00232-x