Abstract
Background
Olfactory groove meningioma (OGM) is characterized by slow-growing tumors that are frequently bilateral as opposed to unilateral & asymmetrical and may cause progressive frontal lobe compression. We aimed to evaluate the value of extradural devascularization as a golden step in bilateral subfrontal approach in management of OGM.
Results
The mean operative time was 158.32 ± 24.88. Blood loss ranged from 500 to 1000 cc with a mean value of 763.64 ± 155.98. The number of patients requiring blood transfusion was 5 (22.7%). Based on Simpson classification, 19 (86.4%) patients had whole tumor excision (grade I, II) & 3 (13.6%) patients had grade III and IV. The incidence of complications among the studied patients is: CSF leak did not occur to any case, pneumocephalus occurred in 1 (4.5%) patient, anosmia occurred in 1 (4.5%) patient, focal CNS deficit occurred in 1 (4.5%) patient, wound infection occurred in 1 (4.5%) patient and hematoma occurred in 1 (4.5%) patient. Only 1 (4.5%) case died due to pulmonary embolism, whereas behavioral manifestations occurred in 9.09% of patients.
Conclusions
The extradural devascularization is a golden step in this approach in management of OGM associated with lower incidence of blood loss intraoperatively (total blood loss was 500–1000 mL, recurrence rate, mortality and additional neurological deficits postoperatively.
Similar content being viewed by others
Background
Olfactory groove meningiomas (OGMs), which comprise 4.5–18% of intracranial meningiomas, are arachnoid cell neoplasms of the frontoethmoidal suture & lamina cribrosa [1]. These meningiomas constitute 10% of all meningiomas in the brain and are believed to originate from arachnoid granulations' arachnoid cap cells in this area [2].
OGM is characterized by slow-growing tumors that are frequently bilateral as opposed to unilateral & asymmetrical and may cause progressive frontal lobe compression. Up to 15—20% of patients exhibit intra-tumoral calcifications [3]. OGM can harm vision by optic chiasma & optic nerve compression if large enough to project toward the sella [4].
Headache alone, or in conjunction with personality changes, visual impairment & anosmia are the most prevalent presenting symptoms [5]. Seizures & intracranial hypertension are uncommon early manifestations. OGMs anatomic placement may result in extended psychological symptoms before the appearance of more pronounced neurologic impairments. OGM are therefore among the largest brain tumors that produce optic chiasma and optic nerve compression leading to visual acuity impairments [6].
OGMs can expand substantially prior to the manifestation onset because of plasticity of the frontal lobe & their insidious growth. OGMs can negatively affect a patient's health & quality of life despite being histologically classified as benign tumors [3].
Magnetic resonance imaging (MRI) & brain computed tomography (CT) scans reveal the meningiomas' typical characteristics in the mid-subfrontal area, the edema around the brain & tumor's extent. In addition, MRI determines the tumor's relationship with the anterior cerebral arteries & optic nerves, as well as its extension into the ethmoidal sinus [7].
Endo-skull base methods are gaining popularity because of specialized training & emergence of strong endoscopic tools in this field of modern neurosurgery, with comparable morbidity & mortality rates [8]. Open techniques continue to be the global standard, including at our hospital and department, for surgery of OGM [9].
However the tumor size, the key vascular and neurological structures encasement, & their migration into the paranasal sinuses create considerable surgical problems during these procedures, surgical resection remain the treatment of choice for most OGMs [10].
Preoperative embolization may be essential to limit intraoperative bleeding as meningioma excision in particular is typically accompanied by high blood loss [11, 12]. This is an issue as considerable intraoperative bleeding, i.e., ≥ 2000 mL, is related to morbidity & mortality. Additionally, excessive bleeding during surgical procedures can necessitate blood donations of platelets, coagulation factors or red cells [13]. Extradural devascularization associated with total blood loss was 500–1000 mL.
There are a few researches discussing the extradural devascularization outcome in resection of giant OGM in bilateral subfrontal approach. Therefore, we aimed to evaluate the value of extradural devascularization as a golden step in bilateral subfrontal approach in management of OGM.
Methods
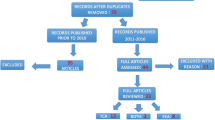
Study design and population
This retrospective study was performed on 22 cases aged > 18 years diagnosed with OGM more than 4.5 cm operated by bilateral subfrontal approach at Neurosurgery Department, Faculty of Medicine, Menoufia University hospitals.
Informed written consent was obtained from the patient or relatives of the patients. The research was performed after being approved by the institutional ethical committee.
When the diameter of a tumor exceeded 4.5 cm, it was classified as a giant [14].
All patients subjected to full history taking (age, sex, complaint, comorbidities, present, past & family history). Clinical evaluation: through general and neurological examination according to standard patient information & routine laboratory examination: as (liver, renal functions, complete blood picture, coagulation profile & blood sugar). ECG and chest X-ray were done as well with the routine preoperative workup. Imaging studies as CT brain and MRI brain were done.
Operative management
After general anesthesia administration to each patient, we inserted a lumbar drain using a lumbar puncture needle and then sealed it. Preoperatively, 8 mg of dexamethasone, 1 gm of a 3rd generation cephalosporin antibiotic, & 17 mg/kg of phenytoin (loading doses) were provided intravenously to all patients. The patient was placed supine with the trunk & legs slightly flexed. The head was placed in a three-point fixation head holder and elevated above the heart 15° to help venous drainage. Eyes were protected. The vertex was tilted down 15–30° allowing the frontal lobes to fall away without traction. Bicoronal scalp incision was performed. Scalp flap including the pericranium was sharply dissected from the bone. To prevent the facial nerve frontal branch injury, the temporal fascia & adipose tissue were raised in one layer by constructing a plane between them & the deep temporalis fascia. After the skin flap was repositioned, 200 mL of mannitol was supplied. During surgery, somewhat more hydration was preserved.
Bilateral subfrontal bone flap was carefully separated from underlying dura, especially in the midline overlying the sagittal sinus. Extradural devascularization is a golden step in bilateral subfrontal approach in management of OGM, by using bipolar cauterization to coagulate the extradural vascular feeders of the meningioma as anterior ethoidal and posterior ethoidal arteries. Before reaching the cistern, and to achieve optimal brain relaxation, the lumbar drain was blocked until the dura opened & around 20 mL of cerebrospinal fluid (CSF) was drained. Following this step, the dura was incised on both sides proximally; superior sagittal sinus was secured and divided. In our experience, sinus scarification in this area did not result in any difficulties. Falcine dura was detached from the crista galli, and the frontal lobes were gradually fallen back. At this time, the operating microscope was used to open basilar cisterns to allow drainage of cerebrospinal fluid.
Because of the gravity effect, it was simple to retract the frontal lobes and approach the tumor. Always, we were avoiding the use of a fixed retractor on the frontal lobes. The lumbar drain & CSF drainage from nearby cisterns made this possible. The suction tip was sufficient for retraction. Initially, a meticulous extracapsular coagulation & internal debulking were conducted. The capsule was subsequently pushed toward the center, and a good plane between it and the surrounding brain tissue was established. Due to the fact that meningiomas have a dural origin and push the arachnoid in front of them, they are located in the subdural space outside the arachnoid. This is of considerable assistance while dissecting the tumor with regard to the arachnoid layer in order to avoid vascular damage. As expected, we first had difficulties visualizing the anterior communicating artery complex & optic chiasma, but we were ultimately able to see the anterior cerebral arteries, their branches, & the optic apparatus by the tumors' excision from anterior to posterior & with patience. Except for one tumor that was linked to vessels, we were able to successfully remove the tumor capsule from this essential neurovascular system. A small piece of the tumor was left behind in this patient.
With respect to the arachnoid plan, gradual debulking and dissection of the tumor was initiated from the anterior to posterior direction, starting at the deepest level of the tumor in the anterior fossa.
After tumor removal, dura was closed watertight, with dural hitching to the periosteum or to small holes in the bone edges. Additional dural defects were reconstructed with pericranium if needed or with artificial dura. The bone flap was held with several sutures through small holes made in the bone edges.
Due to tumor attachment to neurovascular systems, we were able to achieve grade 1, 2 Simpson resection in 19 cases & grade 3, 4 Simpson resection in 3 cases.
Follow-up: from first day of excision by CT brain and every 3 months after discharge clinically by neurological status and radiological by MRI brain with contrast.
Statistical analysis
SPSS version 26 was used for the statistical analysis (IBM Inc., Armonk, NY, USA). To determine whether the data followed a normal distribution, we utilized the Shapiro-Wilks test & histograms. Median & interquartile range (IQR) were used to represent quantitative data that did not fit a normal distribution. The quantitative parameters were shown as mean & standard deviation (SD). The qualitative factors were shown as frequencies and percentages (%).
Case 1
See Fig. 1.
A Sagittal MRI with contrast shows preoperative large OGM. B Coronal MRI with contrast shows preoperative large OGM. C Axial MRI with contrast shows preoperative large OGM. D Immediate postoperative CT brain with contrast shows postoperative excision of OGM with no residual. E Sagittal MRI with contrast shows postoperative complete excision of OGM with no residual. F Coronal MRI with contrast shows postoperative complete excision of OGM with no residual. G Axial MRI with contrast shows postoperative complete excision of OGM with no residual
Case 2
See Fig. 2.
Case 3
A Axial MRI with contrast shows preoperative large OGM. B Coronal MRI with contrast shows preoperative large OGM. C Sagittal MRI with contrast shows preoperative large OGM. D Preoperative CT brain shows preoperative large OGM. E Immediate postoperative CT brain with contrast shows postoperative excision of OGM with no residual
Results
Table 1 shows that patients' age ranging from 25 to 75 years with a mean of 44.14 ± 14.27, 45.5% were males, and 54.5% were females.
Table 2 shows the clinical presentation among the studied patients, 100% of patients had headache, 63.6% of patients had anosmia, 54.5% of patients had mental disturbance, 9.1% of patients had visual disturbance, and 4.5% of patients had seizures.
Table 3 shows the operative data among the studied patients, and the mean intraoperative time was 158.32 ± 24.88. The blood loss ranged from 500 to 1000 cc with a mean value of 763.64 ± 155.98. The number of patients requiring blood transfusion was 5 (22.7%).
Table 4 shows radiological findings among the studied patients, and tumor diameter ranged from 5 to 12 cm with a mean value of 8.82 ± 2.08 cm. Bony hyperostosis occurred in 6 (27.3%) patients, tumor calcification occurred in 4 (18.2%) patients, and extension in paranasal sinuses occurred in 5 (22.7%) patients.
Table 5 shows according to Simpson classification, total tumor removal (grade I, II) was achieved in 19 (86.4%) patients, and grade III& IV was achieved in 3 (13.6%) patients.
Table 6 shows the incidence of complications among the studied patients, CSF leak did not occur to any case; pneumocephalus occurred in 1 (4.5%) patient, anosmia occurred in 1 (4.5%) patient, focal CNS deficit occurred in 1 (4.5%) patient, wound infection occurred in 1 (4.5%) patient, and hematoma occurred in 1 (4.5%) patient. Only 1 (4.5%) case died due to pulmonary embolism. The behavioral manifestations occurred in 9.09% of patients.
Discussion
Cushing and Eisenhardt [15] described for the first time in 1938 the surgical concepts of OGM management. While a multitude of distinct & updated techniques have been created since then, there is still no consensus regarding the most effective approaches [3].
Over time, the strengths & drawbacks of prevalent techniques have been well defined. With wide exposure of the anterior cerebral region, bilateral procedures facilitate the hyperostosis removal from the cribriform region & the radical resection of the tumor [16]. However, it results in delayed vital structures vision, including the visual apparatus & the anterior cerebral/communicating arteries. In both subcarinal & subfrontal methods, the frontal sinuses are frequently required to be opened, which raises the infection risk [3].
It is generally known that tumor volume is a significant factor in technique selection, with bilateral operations providing larger operational areas enabling larger tumor excision. The tumor volume was inversely and positively correlated with GTR for bilateral & unilateral procedures, respectively, but only the latter was shown to be statistically significant. While these patterns appear contradictory, in practice they may not be entirely significant [17].
Herein, we aimed to evaluate the value of extradural devascularization as golden step in bilateral subfrontal approach in management of OGM. If possible, early devascularization & debulking should be applied to all intracranial tumor surgeries in order to ease dissection of the tumor capsule.
Our research describes a group of individuals who were surgically treated for giant olfactory groove meningiomas using a bilateral subfrontal approach. The subfrontal approach without frontal lobe tissue removal was first described by Tonnis in 1938 [18] & subsequently utilized by a number of publications [6, 19].
This technique allows for direct access to the tumor without excessive brain retraction, reaching the primary tumor attachment and vascular feeders of the meningioma, preoperative devascularization by bipolar coagulation, thereby dividing the ethmoidal arteries and small meningeal feeding vessels, devascularizing, and debulking the tumors from the inferior aspect.
In patients with severe bone involvement, it may be necessary to drill the front cranial base and do secondary reconstruction using a vascularized pericranial flap [20].
Predissection devascularization by bipolar coagulation is a golden step to decrease bleeding loss during operation, decrease the need for blood transfusion, decrease time of surgery and for better removal of the tumor [21].
In the same context with our findings, Wei et al. [22] did a case report giant OGM resection with extradural devascularization and discovered that the tumor was totally excised with 500–1000 ml of total blood loss.
During the primary phase, the tumor of our patient was extremely vascular. Once the ethmoidal arteries from the base were cauterized and divided at the cribriform plate, there was a significant reduction in bleeding. The frontal lobe function preservation was an advantage of this strategy. The devascularization success may be influenced by the tumor size as well as location & region of dura attachment. When the connection is large or buried behind a large tumor, intradurally frontal or pterional approaches may be problematic for excision [23].
The extradural method as initially reported by Cushing [15] and later by Derome and Guiot [24] could cut off the blood supply surrounding the crista galli before the dura was opened for tumor removal. Typically, the branches of the ethmoidal arteries [25] are the primary blood vessels feeding these tumors. The extradural route via a frontal or front-orbital craniotomy appears to be a good technique for the ethmoidal blood supply devascularizing prior to tumor excision [26].
Inevitably, the frontal sinus will be exposed, increasing the risk of meningitis is a disadvantage [27]. Our findings revealed that anosmia is an early symptom of OGM, which was found in 63.6% of patients. The olfactory function loss is progressive, comparable to that observed in the elderly, and initially just one side is affected.
It appears that lateralized assessment of olfactory function is required for an early diagnosis [28]. Olfaction maintenance during surgery is tough. Although the olfactory tract remains anatomically continuous following meningioma resection [29], 4.5% of patients may develop postoperative anosmia due to a functional lesion of the fila olfactoria or ischemia resulting from loss of blood supply to the olfactory neurons during operation. In the study by Bassiouni et al. [29] comparing various surgical approaches, there was no difference in the preservation of olfaction. Limited frontal lobe retraction is necessary to avoid future injury to the olfactory nerves.
45% of patients presented with anosmia, according to El-Sisi et al. [27] findings about the outcome of bilateral subfrontal approach to giant OGM. Only 2 of 11 individuals with preoperative unilateral normal olfactory function have preserved olfaction after surgery.
Regarding our findings, total removal (grade I, II) was achieved in 19 (86.4%) patients and grade III& IV was achieved in 3 (13.6%) patients.
In the same context, El-Sisi et al. [27] found that 67–100% of patients with olfactory meningiomas have been reported to have undergone full resection.
Moreover, in our series, subtotal removal grade III&IV was found in 3 (13.6%) patients.
These tumors' recurrence rate ranges from 5 to 41%; however, numerous authors have reported a very low or nonexistent recurrence rate following a mean follow-up time of 4.4–9 years [30].
Meningioma recurrence may emerge from insufficient resection or occur even after extensive resection after a lengthy follow-up period [31]. The tumor excision strategy does not appear to affect tumor recurrence [32].
In contrast, Hentschel et al. [33] ran a OGM series. 11 cases were operated, and each case was completely excised. Two patients underwent subtotal extraction, and both instances were recurring. Also, Nakamura et al. [34] found that the technique has no effect on the rate of tumor clearance. The rate of tumor eradication Simpson grades I & II was 92.7% utilizing frontal lateral approach and 91.2% using the frontal method. In the series OGM performed by El-Bahy [35], subtotal removal was achieved in 4 patients (22.2%) & entire removal of Simpson grades I & II was achieved in 78% (14 of 18 cases).
CSF leakage is a significant issue for anterior skull base tumors, particularly enormous olfactory groove meningioma. CSF was not detected in any cases.
Compared to El-Bahy [35] series of 18 cases, 3 out of 18 patients (16.7%) experienced CSF leaks that resolved with repeated lumbar puncture & medical treatment.
In our present study, only 1 (4.5%) case died due to pulmonary embolism. The mortality rates vary from 0 to 17% in the recent literature. This came in line with EL-Sisi et al. [27] who found on the 17th postoperative day, one fatality due to a major pulmonary embolism, but none directly related to surgery.
Conclusions
Based on our findings, it can be concluded that extradural devascularization is a valuable step in the management of OGM using bilateral subfrontal approach and that careful monitoring is necessary to prevent complications and ensure a good postoperative outcome. The extradural devascularization is a golden step in management of OGM associated with lower incidence of blood loss intraoperatively (total blood loss was 500–1000 mL), recurrence rate, additional neurological impairments & mortality postoperatively. This approach may be considered as a good choice for these tumors more than 4.5 cm in diameter.
Availability of data and materials
Data and material are available on a reasonable request from the author.
Abbreviations
- OGM:
-
Olfactory groove meningioma
- IQR:
-
Interquartile range
- SD:
-
Standard deviation
- BMI:
-
Body mass index
- DM:
-
Diabetes mellitus
- Hb:
-
Hemoglobin
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computed tomography
- CSF:
-
Cerebrospinal fluid
References
Guinto G. Olfactory groove meningiomas. World Neurosurg. 2015;83:1046–7. https://doi.org/10.1016/j.wneu.2014.12.044.
Ikhuoriah T, Oboh D, Abramowitz C, et al. Olfactory groove meningioma: a case report with typical clinical and radiologic features in a 74-year-old Nigerian male. Radiol Case Rep. 2022;17:4492–7. https://doi.org/10.1016/j.radcr.2022.08.077.
Feng AY, Wong S, Saluja S, et al. Resection of olfactory groove meningiomas through unilateral vs. bilateral approaches: a systematic review and meta-analysis. Front Oncol. 2020;10:560–8. https://doi.org/10.3389/fonc.2020.560706.
Loe ML, Maliawan S. Spontaneous recovery of medial prefrontal syndrome following giant olfactory groove meningioma resection: a case report. Bali Med J. 2019;8:380–4.
Niklassen AS, Jørgensen RL, Fjaeldstad AW. Olfactory groove meningioma with a 10-year history of smell loss and olfactory recovery after surgery. BMJ Case Rep. 2021;14:125–9. https://doi.org/10.1136/bcr-2021-244145.
Fountas KN, Hadjigeorgiou GF, Kapsalaki EZ, et al. Surgical and functional outcome of olfactory groove meningiomas: lessons from the past experience and strategy development. Clin Neurol Neurosurg. 2018;171:46–52. https://doi.org/10.1016/j.clineuro.2018.05.016.
Patel B, Desai R, Pugazenthi S, et al. Identification and management of aggressive meningiomas. Front Oncol. 2022;12:851–75. https://doi.org/10.3389/fonc.2022.851758.
Farooq G, Rehman L, Bokhari I, et al. Modern microsurgical resection of olfactory groove meningiomas by classical bicoronal subfrontal approach without orbital osteotomies. Asian J Neurosurg. 2018;13:258–63. https://doi.org/10.4103/ajns.AJNS_66_16.
Khan DZ, Muskens IS, Mekary RA, et al. The endoscope-assisted supraorbital “keyhole” approach for anterior skull base meningiomas: an updated meta-analysis. Acta Neurochir (Wien). 2021;163:661–76. https://doi.org/10.1007/s00701-020-04544-x.
Marenco-Hillembrand L, Bamimore MA, Webb R, et al. Unilateral supraorbital keyhole craniotomy avoiding the frontal sinus for large and giant olfactory-groove meningiomas: a case series. World Neurosurg. 2022. https://doi.org/10.1016/j.wneu.2022.11.015.
Raper DM, Starke RM, Henderson F Jr, et al. Preoperative embolization of intracranial meningiomas: efficacy, technical considerations, and complications. AJNR Am J Neuroradiol. 2014;35:1798–804. https://doi.org/10.3174/ajnr.A3919.
Ilyas A, Przybylowski C, Chen CJ, et al. Preoperative embolization of skull base meningiomas: a systematic review. J Clin Neurosci. 2019;59:259–64. https://doi.org/10.1016/j.jocn.2018.06.022.
Hsu S-Y, Huang Y-H. Characterization and prognostic implications of significant blood loss during intracranial meningioma surgery. Transl Cancer Res. 2016;5:797–804.
Gambacciani C, Grimod G, Sameshima T, et al. Surgical management of skull base meningiomas and vestibular schwannomas. Curr Opin Oncol. 2022;34:713–22. https://doi.org/10.1097/cco.0000000000000904.
Cushing H. Meningiomas: their classification, regional behavior, life history, and surgical end result. Springfield Charles C Thomas. 1938;111:735–45.
Omay SB, Schwartz TH. Endoscopic and minimally invasive meningioma surgery. In: Meningiomas: comprehensive strategies for management. 2020. p. 97–108.
Lemée JM, Corniola MV, Da Broi M, et al. Extent of resection in meningioma: predictive factors and clinical implications. Sci Rep. 2019;9:59–64. https://doi.org/10.1038/s41598-019-42451-z.
Tönnis W. Zur operation der meningeome der siebbeinplatte. Zentralbl Neurochir. 1938;1:1–7.
Alam S, Uddin ANW, Sharif MS, et al. Microsurgical excision of olfactory groove meningiomas, comparative studies of different surgical approaches. Bangladesh J Med Sci. 2020;10:9–19.
Mahmoud MW, Moataz AE, Elhawary E. Predicting the outcome of microsurgical resection of olfactory groove meningiomas (OGMs): experience at Benha University Hospital. Med J Cairo Univ. 2019;87:3839–44.
Iampreechakul P, Tirakotai W, Lertbutsayanukul P, et al. Pre-operative embolization of intracranial and extracranial tumors: a review of 37 cases. J Med Assoc Thai. 2016;99:91–119.
Wei CP, Wang AD, Tsai MD. Resection of giant olfactory groove meningioma with extradural devascularization. Skull Base. 2002;12:27–31. https://doi.org/10.1055/s-2002-21570-1.
Babu R, Barton A, Kasoff SS. Resection of olfactory groove meningiomas: technical note revisited. Surg Neurol. 1995;44:567–72. https://doi.org/10.1016/0090-3019(95)00196-4.
Derome PJ, Guiot G. Bone problems in meningiomas invading the base of the skull. Clin Neurosurg. 1978;25:435–51. https://doi.org/10.1093/neurosurgery/25.cn_suppl_1.435.
Moscote-Salazar LR, Dolachee AA, Narvaez-Rojas A, et al. Preoperative embolization of skull–base tumors: indications, utility, and concerns. J Acute Dis. 2019;8:89–102.
Setty P, Fernandez-Miranda JC, Wang EW, et al. Residual and recurrent disease following endoscopic endonasal approach as a reflection of anatomic limitation for the resection of midline anterior skull base meningiomas. Oper Neurosurg (Hagerstown). 2021;21:207–16. https://doi.org/10.1093/ons/opab244.
El-Sisi YB, Rashed MES, Hanafy AM, et al. The outcome of bilateral subfrontal approach of large olfactory groove meningioma. Menoufia Med J. 2015;28:93–105.
Parma V, Boesveldt S. Measurement of olfaction: screening and assessment. In: Sensory science and chronic diseases: clinical implications and disease management. Springer; 2021. p. 45–63.
Bassiouni H, Asgari S, Stolke D. Olfactory groove meningiomas: functional outcome in a series treated microsurgically. Acta Neurochir (Wien). 2007;149:109–21. https://doi.org/10.1007/s00701-006-1075-z. (discussion 21).
Yonekawa Y. Operative neurosurgery: personal view and historical backgrounds. (5) Meningioma. No Shinkei Geka. 2009;37:71–90.
Nakasu S, Fukami T, Jito J, et al. Recurrence and regrowth of benign meningiomas. Brain Tumor Pathol. 2009;26:69–72. https://doi.org/10.1007/s10014-009-0251-2.
Gil Z, Spektor S, Abergel A, et al. The subcranial approach for tumors involving the anterior skull base. Harefuah. 2003;142:416–20.
Hentschel SJ, DeMonte F. Olfactory groove meningiomas. Neurosurg Focus. 2003;14:4–12. https://doi.org/10.3171/foc.2003.14.6.4.
Nakamura M, Struck M, Roser F, et al. Olfactory groove meningiomas: clinical outcome and recurrence rates after tumor removal through the frontolateral and bifrontal approach. Neurosurgery. 2007;60:844–52. https://doi.org/10.1227/01.Neu.0000255453.20602.80.
El-Bahy K. Validity of the frontolateral approach as a minimally invasive corridor for olfactory groove meningiomas. Acta Neurochir (Wien). 2009;151:1197–205. https://doi.org/10.1007/s00701-009-0369-3.
Acknowledgements
Nil.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
YBE and MAH conceived and supervised the study; SEA and YBE were responsible for data collection. MAH and SEA analyzed and interpreted the data. All authors provided comments on the manuscript at various stages of development. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate:
It was approved by the ethics committee of Faculty of Medicine, Menoufia University, and it was started at January 2022 and ended by December 2022. An informed written consent was obtained from the participants.
Consent for publication
All patients gave their consent for publication in the journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elsisi, Y.B., Hossen, M.A. & Al Emam, S.E. Outcome of extradural devascularization in resection of giant olfactory groove meningioma in bilateral subfrontal approach. Egypt J Neurosurg 38, 28 (2023). https://doi.org/10.1186/s41984-023-00205-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-023-00205-0