Abstract
Introduction
Spinal metastases are a classic complication of lung cancer. New palliative treatment modalities have emerged. Among them are minimally invasive approaches such as balloon kyphoplasty. With the aim of evaluating the efficiency of balloon kyphoplasty in the control of spinal pain during these lesions, we report a series of 24 patients.
Methods and materials
Over a period of 6 years, we retrospectively studied 24 files of patients suffering from vertebral compression of metastatic pulmonary origin and treated by balloon kyphoplasty from January 2009 to December 2014 in the neurosurgery department of the North Hospital of Marseille (France).
Results
The mean age was 66.2 years (39–80 years) with a sex ratio of 5. Dorsal location was predominantly 17 cases. Balloon kyphoplasty involved one level in 14 patients. The general condition (Karnofski) was bad in 16 patients. Survival prediction was less than 6 months in 22 patients. The indication was mainly pain with a mean visual analog scale of 7.7. The evolution was marked by the regression of the painful symptomatology in all patients with a mean visual analog scale of 2.2 postoperatively. Postoperative complications were noted in two cases (pulmonary embolism, compression of the left iliac vein).
Conclusion
Our short series shows the efficacy and low morbidity of balloon kyphoplasty in the control of spinal pain secondary to vertebral metastases of bronchopulmonary cancers.
Similar content being viewed by others
Introduction
The occurrence of bone metastases is a common occurrence in bronchopulmonary cancers (BPC). Nearly 40% of patients have bone metastases at diagnosis or during the course of lung cancer, and in 40% of cases, these are spinal metastases [1]. The evolution of these spinal lesions is characterized in 50% of cases by the occurrence of bone events such as pain, fracture, malignant hypercalcemia and/or spinal cord compression (SC). SC is the most serious event, involving the functional prognosis. Pain secondary to tumor invasion of the vertebral column is a major detriment to the quality of life of these patients [2, 3].
While medical treatment may be effective in managing pain in some patients, mechanical pain due to pathologic fractures may require surgery. Traditionally, symptoms have been treated by decompression of the spinal cord through laminectomy. However, many patients with spinal tumors are at higher risk of complications from open surgery [3].
Recent advances in percutaneous procedures such as kyphoplasty and vertebroplasty, which indicated in patients with pain and instability, have created options for patients who were not previously considered candidates for surgery. [4, 5]
In this work, we report a series of 24 patients with spinal metastases of BPC with the aim of evaluating the effectiveness of balloon kyphoplasty in the control of spinal pain during these lesions.
Materials and methods
Twenty-four patients with vertebral compression of pulmonary metastatic origin were treated with kyphoplasty from January 2009 to December 2014 in the neurosurgery department of the North Hospital in Marseille, France.
The parameters studied were age, sex, lesion level, Karnofsky and Tokuhashi scores, pain assessment by visual analog scale (VAS): Pain was considered mild when the VAS was less than 4, moderate when the VAS was between 4 and 6, and severe when the VAS was greater than 6, indication, preoperative symptom delay, evolution: It was considered good when the postoperative VAS was less than 4; moderate when the VAS was between 4 and 6; and poor when the VAS was greater than 6, complications, and length of hospitalization.
The procedure consisted in creating a cavity in the vertebral body by inflating a balloon before injecting cement, polymethylmethacrylate (PMMA) through a transdermal cutaneous approach (Fig. 1).
Inclusion criteria
All patients with metastatic vertebral compression.
Exclusion criteria
All patients with metastatic vertebral compression of other than pulmonary origin and all patients who received other treatment methods than balloon kyphoplasty (vertebroplasty, open surgery, analgesic radiotherapy and conservative treatment).
The data collected were analyzed using SPSS version 21.0 software. The anonymity of the patients was preserved, and the study was exempted from the obligation to obtain ethical approval by the ethical committee of North Hospital (Marseille-France).
Results
The mean age was 66.2 years (range 51–80 years), with a sex ratio of 5 (20 male/4 female).
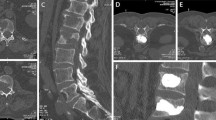
The location was dorsal in 17 cases, lumbar in 6 and sacral in 1 case. Figure 2 shows the number of vertebral levels involved in kyphoplasty, and Fig. 3 illustrates the 4-level kyphoplasty.
The general condition was moderate in 8 cases (Karnofsky: 50–70) and bad in 16 cases (Karnofsky: ≤ 40). The Tokuhashi index is summarized in Table 1.
The operative indication was essentially the pain present in all patients and persisting under major analgesics with a mean VAS of 7.7 and extremes ranging from 6 to 10. This pain was moderate in 4 cases (18.1%) and severe in 20 cases (81.9%).
The preoperative delay of symptoms was on average 12.4 days with extremes of 7 and 32 days.
The evolution was marked by the regression of pain in all patients with an average VAS of 2.2 postoperatively, VAS less than 4 in 21 patients and 4 in 3 patients.
Postoperative complications were noted in two cases (Fig. 4). These were one case of cement extravasation with compression of the right iliac vein and one case of pulmonary embolism.
The average postoperative length of stay was 3.7 days.
Discussion
Spinal metastases are a classic complication of lung cancer [2].
Advances in the treatment of cancer, extending the life expectancy of patients with metastases, have increased the number of patients with complications of vertebral metastases, including compression fractures causing severe pain [4]. With no hope of healing for most of these patients, palliative care becomes paramount because conventional surgical treatment of these fractures is often too invasive, especially in the elderly [6]. In response, new palliative treatment modalities have emerged. These include minimally invasive approaches such as balloon kyphoplasty, which indicated in patients suffering from pain and instability [7, 8].
Spinal metastases occur most often in the thoracic spine (70%), followed by the lumbar spine (20%) and finally the cervical spine (10%) [9]. As in our series, the thoracic location was the most frequent (17/24), followed by the lumbar (6/24). However, we did not note a cervical location but rather a sacral one.
The functional impact of the disease was assessed by the Karnofsky index, and survival was evaluated by the Tokuhashi index. Indeed, these scores are important elements in therapeutic decision making because most of the patients with spinal metastases have an altered general state and a relatively short life expectancy averaging 10 to 11 months, indicating less aggressive palliative treatments, including balloon kyphoplasty [10, 11].
Balloon kyphoplasty is a minimally invasive, radiologically guided procedure. It is a modified version of vertebroplasty, involving the inflation of a balloon in a collapsed vertebral body to create a vacuum prior to the injection of PMMA. In addition to providing rapid pain relief, kyphoplasty reduces the incidence of acute fractures, allows controlled placement of cement under lower pressure, allows bone biopsy and leads to improved deformity, although this is not a goal in the case of vertebral metastases [12,13,14]. Although it does not improve survival outcomes in patients with metastases, palliation is a reasonable goal when life expectancy is short, and treatment of vertebral fractures may reduce the incidence of complications associated with bed rest, which may be particularly relevant for elderly patients [6].
Fourney et al. [8] studied the efficacy and safety of vertebroplasty and kyphoplasty in 56 patients with either vertebral metastases or multiple myeloma of the spine. Eighty-four percent of these patients reported complete or significant pain relief, with statistically significant improvements in median preoperative and postoperative VAS scores. In a series of five patients with tumors of the vertebral body who were treated with kyphoplasty, Gaitanis et al. [15] found that all patients experienced significant and immediate improvement in pain. In our series, we noted a regression of pain in all patients with a mean VAS that went from 7.7 preoperatively to 2.2 postoperatively. The results of these previous studies are consistent with our findings and demonstrate that kyphoplasty is an effective and safe procedure.
The injection of PMMA into the affected vertebral body allows immediate stabilization of the fracture. PMMA is also reported to have therapeutic effects on the underlying tumor cells in the affected vertebral body [6]. According to some authors [6, 16], PMMA has cytotoxic activity, thermal effects and ischemia. When injected into the affected vertebral body, the cement occupying the space will inhibit the growth of tumor cells. More importantly, the vascular structures, which are essential for the growth of the underlying tumor, are destroyed by the considerable exothermic reaction of the implant during polymerization, by the chemical and toxic effects of the monomer, by compressive effects on small nerves and by ischemic phenomena resulting from the blocking of small vessels by PMMA. In the future, it is not inconceivable that PMMA could be used as a delivery system for anti-cancer drugs.
The classic complications of percutaneous vertebroplasty are cement leakage into the spinal canal [17]. It is all the more frequent when spinal metastases are treated: up to 37.5% of patients treated [8] and pulmonary cement embolism, sometimes with severe consequences [18]. The two major mechanisms of leakage are insufficient polymerization of PMMA cement and excessive cement injection [18]. Balloon kyphoplasty reduces the risk of cement leakage, thanks to its principle of injecting the ideal volume of cement without pressure [8, 19, 20]. In our series of patients, we noted one case of cement leakage with asymptomatic compression of the left iliac vein and one case of medically treated pulmonary embolism.
Surgery for vertebral metastases can lead to complications and prolonged hospital stays when vertebrectomies are proposed [21]. The most common surgical problem is blood loss, which may require a transfusion (on average two blood concentrates; average blood loss 1500 ml). Infectious and neurological complications are also reported at 5% [22]. The average length of hospital stay for surgical series is 10 days; it varies (between 2 and 79 days) depending on the surgical procedure and the complications that occur [22]. This duration is short in the case of minimally invasive surgery; it was 3.7 days in our series (2–7 days).
One of the limitations of this study was that there was no control group that underwent conservative treatment or vertebroplasty. A comparison between balloon kyphoplasty and vertebroplasty would have been enlightening, especially with regard to the incidence of cement leakage. Another limitation of this study was its retrospective nature but also the lack of evaluation of balloon kyphoplasty in the restoration of vertebral height and stability.
Conclusions
Our short series shows the efficacy and low morbidity of balloon kyphoplasty in the control of spinal pain secondary to vertebral BPC metastases. The encouraging results of this study prompt us to suggest further large-scale prospective evaluations of balloon kyphoplasty in patients with vertebral metastases.
Availability of data and materials
Not applicable.
Abbreviations
- BPC:
-
Bronchopulmonary cancers
- SC:
-
Spinal cord compression
- VAS:
-
Visual analog scale
- PMMA:
-
Polymethylmethacrylate
References
Jacoulet P. Bone metastases of bronchopulmonary cancers. J Respir Dis Actual. 2015;7:445–54.
La Combe B, Gaillard S, Bennis S, Chouaid C. Management of spinal metastases of bronchopulmonary cancer. J Respir Dis. 2013;30:480–9.
Chi JH, Gokaslan ZL. Vertebroplasty and kyphoplasty for spinal metastases. Curr Opin Support Palliat Care. 2008;2:9–13.
Astur N, Avanzi O. Balloon kyphoplasty in the treatment of neoplastic spine lesions: a systematic review. Glob Spine J. 2019;9(3):348–56.
Hariri O, Takayanagi A, Miulli DE, Siddiqi J, Vrionis F. Minimally invasive surgical techniques for management of painful metastatic and primary spinal tumors. Cureus. 2017;9(3):1114.
Qian Z, Sun Z, Yang H, Yong Gu, Chen K, Guizhong Wu. Kyphoplasty for the treatment of malignant vertebral compression fractures caused by metastases. J Clin Neurosci. 2011;18:763–7.
Berenson J, Pflugmacher R, Jarzem P. Cancer Patient Fracture Evaluation (CAFE) Investigators. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol. 2011; 12:225–35.
Fourney DR, Schomer DF, Nader R. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg. 2003;98:21–30.
Klimo P, Schmidt MH. Surgical management of spinal metastases. Oncologist. 2004;9:188–96.
Hsiang J. An unconventional indication for open kyphoplasty. Spine J. 2003;3:520–3.
North RB, LaRocca VR, Schwartz J, North CA, Zahurak M, Davis R, McAfee PC. Surgical management of spinal metastases: analysis of prognostic factors during a 10-year experience. J Neurosurg. 2005; (Spine 2): 564–573.
Becker S, Tuschel A, Chavanne A. Balloon kyphoplasty for vertebra plana with or without osteonecrosis. J Orthop Surg (Hong Kong). 2008;16:14–9.
Hillmeier J. Balloon kyphoplasty. Orthopade. 2010;39:665–72 ([in German with English abstract]).
Yang T, Liu S, Lv X. Balloon kyphoplasty for acute osteoporotic compression fractures. Interv Neuroradiol. 2010;16:65–70.
Gaitanis IN, Hadjipavlou AG, Katonis PG. Balloon kyphoplasty for the treatment of pathological vertebral compressive fractures. Eur Spine J. 2005;14:250–60.
Yang HL, Sun ZY, Wu GZ. Do vertebroplasty and kyphoplasty have an antitumoral effect? Med Hypotheses. 2011;76:145–6.
Ryu SK, Park CK, Kim MC, Kang JK. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg 2002; (Spine 1) 96, 56–61.
Charvet A, Metellus P, Bruder N, Pellissier D, Grisoli F, Gouin F. Cement pulmonary embolism during vertebroplasty. French Ann Anesthesia Reanim. 2004;23:827–30.
Atalay B, Caner H, Gokce C, Altinors N. Kyphoplasty: 2 years of experience in a neurosurgery department. Surg Neurol. 2005;64:72–6.
Boszczyk BM, Bierschneider M, Schmid K, Grillhösl A, Robert B, Jaksche H. Microsurgical interlaminary vertebro- and kyphoplasty for severe osteoporotic fractures. J Neurosurg. 2004; (Spine 1) 100: 32–37.
Fuentes S, Métellus P, Pech-Gourg G, Adetchessi T, Dufour H, Grisoli F. Open focus kyphoplasty treatment of spinal metastases. Neurosurgery. 2007;53:49–53.
Holman PJ, Suki D, McCutchein Wolinsky JP, Rhines LD, Gokaslan ZL. Surgical management of metastatic disease of the lumbar spine: experience with 139 patients. J Neurosurg. 2005; (Spine 2): 550–63.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All the authors meet the 4 criteria of the International Committee of Medical Journal Editors (ICMJE): 1. Substantial contributions to research design or methods or to acquisition, analysis or interpretation of data; 2. preliminary writing of the article or its critical review involving significant contribution to the intellectual content; 3. final approval of the version to be published; 4. commitment to assume accountability for all aspects of the research by ensuring that the issues related to the accuracy or integrity of any part of the work are examined in a manner that appropriate and resolute. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study was exempted from the obligation to obtain ethical approval by the ethical committee of North Hospital, Marseille-France (Phone: + 33 04 91 38 00 00).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Faye, M., Barry, L.F., Sy, E.H.C.N. et al. Spinal metastases of bronchopulmonary cancers: interest of balloon kyphoplasty in the control of mechanical rachialgia. Egypt J Neurosurg 37, 13 (2022). https://doi.org/10.1186/s41984-022-00153-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-022-00153-1