Abstract
Background
Meningioma arising from locations in the vicinity of the optic nerve or chiasm may affect the visual function and sometimes the presentation of such tumors. Decompression of the optic nerve or chiasm can give a chance for the visual function to recover.
Methods
Thirty patients who had visual function affection and underwent meningioma excision are followed up for a period of 1 year with regular follow of their visual function periodically.
Results
In this study, females were more prevalent than males, 24 out of 30, age ranged from 24 to 72 years at the time of surgery, half the patients (15) presented with visual deterioration, the other patients presented with headache, seizure, proptosis, or accidentally discovered.
Twenty-two patients improved concerning their visual function over time, 6 patients had a stationary course, and 2 patients deteriorated postoperatively.
Conclusion
Follow-up of patients after surgical excision of meningioma compressing the anterior optic pathway showed gradual improvement in vision in follow-up period up to 1 year, although the improvement in visual function showed a surge in early postoperative period, with continuous less steep improvement afterwards till the end of the observation period.
Surgical excision of meningiomas compressing the anterior visual pathway gives chance for recovery of visual function, more in younger patients, patients with a shorter period of visual deterioration, and patients with mild affection of the preoperative visual status.
No statistically significant influence of tumor site, size, degree of excision, and surgical approach on the postoperative visual outcome in this series.
Similar content being viewed by others
Introduction
Meningiomas are benign, slow-growing tumors, but their expansion may result in compression of the nearby structures such as meningiomas in the vicinity of the anterior visual pathways [1].
Excision of meningioma tumors was initially associated with significant mortality and morbidity; today, a number of factors such as advanced microsurgical techniques, intraoperative electrophysiological monitoring of cranial nerve functions, improved neuro-anesthesia regimens, and postoperative supportive care have reduced operative as well as postoperative mortality and morbidity [2].
Optic nerve compression is variable depending on the size and the location of the tumor; bilateral optic nerve involvement and optic chiasm compression further add to the complexity of the surgical decision-making process [3].
The primary goal of surgery is the total removal of the tumor, with improvement or at least preservation of the preoperative visual status [3].
In this setting, complete non-traumatic decompression of the optic pathway is crucial, with particular attention paid to the full preservation of the attendant delicate blood supply of the optic nerve and chiasm [3].
The optic pathway has a delicate blood supply. The intradural portion of the optic nerve and the optic chiasm receive their blood supply from perforating vessels coursing from the internal carotid artery (ICA) directly or from the superior hypophyseal artery (SHA). These perforating vessels arising directly from the ICA represent the sole blood supply to the inferior decussating fibers of the chiasm [4].
This delicate blood supply is vulnerable to either direct surgical trauma or delayed vasospasm from manipulation [3].
Several reports have evaluated the criteria for visual recovery in patients with these tumors, with series documenting a 25 to 80% chance of visual improvement; this discrepancy is depending on tumor size, location, extension, preoperative visual status, duration of symptoms, and the surgical technique [3].
The main factor influencing visual outcomes was the preoperative visual status; this is mostly related to the duration of symptoms and greater pressure on the optic system which will result in worse visual outcome. Duration of symptoms prior to treatment is thought to be an important factor in the visual outcome of patients [2].
The choice of the approach for removing such lesions depends on many factors, including the origin of the meningioma; size of the tumor; relationship to important structures, including the optic pathway, ICA, and its branches; extension into the cavernous sinus; and extent of bone involvement [5].
Immediate postoperative deterioration and progressive decrease of vision reflect the high possibility of direct vascular insult to the optic apparatus during surgery rather than simply transient neural edema [2].
Methodology
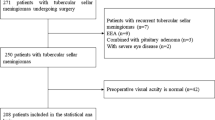
This is an observational study; between July 2015 and August 2019, 30 patients (24 women and 6 men) with meningiomas related to anterior optic pathway underwent surgery performed by senior professors. Patients’ age ranged from 24 to 72 years (mean 49.4 years). Patients were followed up for a period of 1 year with periodic evaluation of visual function.
Patients’ data, age, sex, and vision deterioration are recorded preoperatively.
Pathological feature of the tumor concerning the site of origin, size, period of symptoms before surgery degree of resection, and postoperative histopathological analysis, in addition to presentation and postoperative complications, are also recorded (Table 1).
Preoperative imaging (MR and CT studies of the brain) were evaluated to define tumor site, size, origin, and extension of the tumor including compression and encasement of surrounding structures (Table 2).
Full ophthalmological assessment was done preoperatively, in the early postoperative evaluation, and through the follow-up examinations. It included visual acuity, visual field, fundus examination, color vision, and ocular motility.
Visual parameters of the patients at follow-up visits at 3, 6, and 12 months were recorded and statistically analyzed.
Patients were operated by different approaches according to the pathology size, site, and adherence to adjacent neurovascular structure.
In this series, certain inclusion and exclusion criteria were applied:
-
1.
Inclusion criteria
-
(a)
Patients with MRI findings suggestive of meningiomas compressing the optochiasmic complex
-
(b)
Patients with compressive optic neuropathy
-
(a)
-
2.
Exclusion criteria
-
(a)
Compressive optic neuropathy which is caused by reasons other than meningiomas compressing the optochiasmic complex
-
(b)
Meningiomas in optochiasmic region not causing compressive optic neuropathy
-
(c)
Patients who received radiotherapy to the tumor site
-
(a)
Results
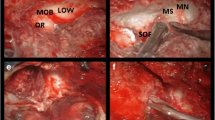
Visual function improvement was observed in most of the patients (Figs. 1, 2, 3 and 4).
Patients with younger age (mean age 46.8) at the time of presentation had a chance for improvement of vision better than those patients in the older age group (mean age 65.6).
Improvement was noted in all visual parameters (acuity, field, and fundus condition).
The improvement in visual acuity was more prominent in patients with better preoperative visual status (Fig. 5).
Visual field also showed improvement over time with nearly proportionally matching results to the improvement in visual acuity in the same patients (Fig. 6).
Visual field improvement also was noticed to be better in those patients with preoperative favorable visual field (Fig. 6).
Color vision was affected in 10 patients of the 30 patients preoperatively and improved in 2 cases at follow-up and was not statistically of significance and dealt with as qualitative variant in the follow-up.
It was observed that tumors in the close vicinity to the anterior optic pathway like clinoidal and tubercullum sellae meningiomas has a smaller size at presentation and also has a shorter period of complaint before diagnosis.
Tumors with more distant site, larger size at presentation, and later diagnosis were observed in olfactory grove and sphenoid wing meningiomas.
Tumors were operated through the unilateral sub-frontal approach in 12 (40%) patients and through the classical pterional approach in 9 (30%) patients, frontolateral approach in 8 cases (26.7%), and only one case through frontotempro-orbitozygomatic representing 3.3%.
Discussion
This is a series of 30 patients diagnosed to have meningioma which is compressing the anterior visual pathway and causing visual deterioration, they have completed the follow-up period for 1 year; females represented 80% of patients included in this research.
Improvement in visual function was noticed in 73.3% of patients after surgical resection, and stationary course was recorded in 20% and deterioration of vision in 6.7% of patients which has a slight discrepancy from what Yasargil [6] and Ohata et al. [7] concluded, respectively, that improvement of vision was noted in 50% and 66%, while in 17% and 28% it remained unchanged and deterioration was noted in 10% and 25%.
The duration of symptoms before recognition of presence of tumors and starting preparation for surgery ranged between 2 and 24 months, which was shorter in tumors originating from locations immediately close to the optic canal and chiasm like diaphragma sellae, clinoidal, and tuberculum sellae meningiomas and longer duration in tumors originating from more distant areas like olfactory groove, planum sphenoidale, and sphenoid wing meningiomas, the duration of symptoms had no significant implication on the recovery of vision of our patients which is not matching the results of Schick and Hassler [5] who concluded in their study on surgical management of tuberculum sellae meningiomas that longer duration of preoperative symptoms correlated with worse recovery; also, Zevgaridis et al. [8] concluded “visual prognosis was favorably affected in patients duration of symptoms of less than seven months”. It may be the scope of study made the discrepancy between the Schick and Zevgaridis studies and this study as they focused only on the tuberculum sellae and anterior clinoid meningiomas which are of the nearest origin and rapidly eruptive tumors for vision deterioration according to our analysis.
In this study the tumor size and the site of origin had statistically non-significant impact on the postoperative results which are not matching the results of Schick and Hassler [5] which concluded that tumor size and location had effect on outcome.
In this study, from the analysis of patients’ age at the time of presentation, we noticed that patients at a lower age group are more favorably recovered concerning visual function (mean age 46.8 years) more than patients in higher age (56.6 years) group which matches the series by Zevgaridis et al. [8] “visual prognosis was favorably affected by age under 54 years,” and, according to Zevgaridis’ hypothesis, ischemia is the cause of primary visual loss rather than simply optic nerve compression, so younger patients are able to compensate for microvascular deprivation more effectively than older ones.
In this study, there is a substantial improvement in visual acuity in most of patients postoperatively especially in the groups with near-normal and moderate-low vision preoperatively; this improvement was most significant in the early postoperative period to 3 months follow-up visit; this improvement continued in further follow-up in less significant rate with also more prominent improvement in the better function group, the severe and profound low vision groups, and blindness group, as those with no perception of light NPL had non-significant improvement in the bad group with no improvement in the very bad group; these findings matches the results from Grkovic and Davidovic [9].
The statistical analysis of data in this study revealed important correlation between preoperative visual acuity status and vision improvement.
There is significant improvement in visual field over the time; the improvement was most significant in the first 6 months after surgery with slower and less significant improvement in the remaining time of the study.
In the follow-up evaluation of the visual field of the patient, there was a modest more affection in the visual field more than that in acuity in same patients, which may be due to unawareness of patients of field cuts as their central vision is not affected.
There is a significant improvement in visual field over time especially in the patients with better visual field evaluation preoperatively than those with worse values of visual field assessment preoperatively; also, improvement was more evident in the early postoperative period with more gradual improvement in following visits.
It was found a significant correlation between fundus examination status and postoperative recovery as those patients with just optic nerve head edema or no significant change in fundus on preoperative evaluation had the most significant and important improvement compared to groups with optic cupping or atrophy.
Conclusion
In this study, most of the patients improved in all scales of preoperative visual statuses, more significant in the better preoperative vision group, preoperative age of patient, and preoperative visual acuity; field status and fundus examination condition showed up as significant parameters concerning search for characteristics which are indicative for vision recovery prognosis. No parameter is a standalone predictor concerning specificity for vision recovery prognosis but sensitive predictor to predict chances of vision recovery after non-complicated blood vessels preserving microsurgery for excision of meningiomas compressing the optochiasmic complex.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the attached file (Results).
Abbreviations
- ICA:
-
Internal carotid artery
- SHA:
-
Superior hypophyseal artery
- MR:
-
Magnetic resonance
- CT:
-
Computed tomography
- FOTZ:
-
Frontoorbito-tembrozygomatic
- NPL:
-
No perception of light
References
Jacob M, Wydh E, Vighetto A, Sindou M. Visual outcome after surgery for cavernous sinus meningioma. Acta Neurochir. 2008;150(5):421–9 discussion 429.
Mehrazin M, Mirfalah R. Early post operative visual outcome in microsurgically treated suprasellar meningiomas predict long-term visual outcome. Turkish Neurosurg. 2008;18(4):380–6.
Taha ANM, Erkmen K, Dunn IF, Pravdenkova S, Al-Mefty O. Meningiomas involving the optic canal: pattern of involvement and implications for surgical technique. Neurosurg Focus. 2011;30(5):E12.
Bergland R. The arterial supply of the human optic chiasm. J Neurosurg. 1969;31:327–34.
Schick U, Hassler W. Surgical management of tuberculum sellae meningiomas: involvement of the optic canal and visual outcome. J Neurol Neurosurg Psychiatry. 2005;76:977–83.
Yasargil MG. Microneurosurgery: Principles, Applications, and Training. Anterior cranial fossa meningiomas. In: Yasargil MG, 1991.
Ohta K, Yasuo K, Morikawa M, Nagashima T, Tamaki N. Treatment of tuberculum sellae meningiomas:a long-term follow-up study. J Clin Neurosci. 2001 May;8 Suppl 1:26–31.
Zevgaridis D, Medele RJ, Muller A, et al. Meningiomas of the sellar region presenting with visual impairment: impact of various prognostic factors on surgical outcome in 62 patients. Acta Neurochir. 2001;143:471–6.
Grkovic D, Davidovic S. Prognostic factors for postoperative visual outcome in surgically treated suprasellar meningiomas. Med Pregl. 2016;69(5–6):146–52.
Acknowledgements
Prof. Dr. Hamdy Ibrahim had provided support with the data of some of his patients.
Funding
There was no funding or any financial support for the current study.
Author information
Authors and Affiliations
Contributions
The first author (Ali Kotb Ali) had a substantial role in study design, manuscript editing, and operating most of the patients. In addition, the co-authors (Ahmad Elsayed Desouky, Tarek Hamdy, Mohammed Abdulrahamn, and Mahmoud Galaleldeen) actively participated in data acquisition and interpretation and manuscript revision. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
An approval from the research ethics committee of the Faculty of Medicine, Ain Shams University, with reference number 000017585 was obtained before the start of the study.
Consent for publication
Consent for surgery and participation in the study of the patients were obtained before surgery. Consent for publication was not required from 29 patients as details, images and videos of each individual participant were not used in manuscript; only one participant was consented for publication as his data and images were included.
Competing interests
All co-authors have seen and agreed with the contents of the manuscript and there is neither a financial nor a non-financial competing interest to report.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Results.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ali, A.K., Elayoty, A.E.D., Elserry, T.H. et al. Visual outcome predictors after surgical excision of meningiomas compressing the optochiasmatic complex. Egypt J Neurosurg 35, 17 (2020). https://doi.org/10.1186/s41984-020-00088-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-020-00088-5