Abstract
Background
There is a debate over the origin of bleeding in case of spontaneous spinal epidural hematoma (SSEH). The most widely accepted theory is of venous origin. Since the epidural veins are valveless, there will be increased venous pressure transmitted from intrathoracic and intraabdominal compartments on straining, causing rupture. Another view is that only arterial bleeding can cause rapid compression of spinal cord, since the venous pressure is less than intrathecal pressure. There is a lack of consensus on treatment also. Most of the authors recommend urgent decompressive laminectomy. There is a recent trend towards less invasive options such as partial laminectomy and hemilaminectomy and conservative treatment.
Aim, materials, and methods
Aim of this study is to review the theories about the origin of bleeding in spontaneous spinal epidural hematoma and the methods of treatment. Literature search was done in PubMed for theories of the origin of spontaneous spinal epidural hematoma and the treatment methods. Descriptive analysis was done.
Case presentation
A 49-year-old male stoneworker presented with thoracic back pain of acute onset while doing work, followed by weakness of forearm and legs. He had paraplegia with grade 1 power of lower limbs. MRI showed posterior epidural hematoma from C3 to T4. Midline partial laminectomy was done from C5 to T2. Hematoma was evacuated. His power improved over 1 week. Later CT (computed tomography) angiography showed no vascular malformation.
Conclusion
Cervical location and rapid development of weakness point towards arterial origin of spontaneous spinal epidural hematoma. Thoracic location and presence of peroperative venous ooze suggest venous origin. Partial or hemilaminectomy is recommended to reduce postoperative instability. Conservative treatment is preferred in case of coagulopathy.
Similar content being viewed by others
Background
Spinal epidural hematoma occurring in the absence of any trauma or iatrogenic procedure is described as spontaneous spinal epidural hematoma (SSEH) [1]. Coagulopathy, vascular malformation, cavernous angioma, or tumor may cause it. When no cause can be identified, it can be termed idiopathic [1]. There is a debate over the origin of bleeding. Literature describes both venous and arterial origins, although the most widely accepted theory is of the venous origin [1, 2]. There is a lack of consensus on treatment also. Although early surgery is recommended, there are reports of successful conservative treatment [1]. There is a trend towards hemilaminectomy and partial laminectomy also [3, 4].
Aim, materials, and methods
The aim of this study is to review the theories about the origin of bleeding in spontaneous spinal epidural hematoma and the methods of treatment. Search was done in PubMed for the etiology of SSEH, for the treatment methods, and for the anatomy of spine vasculature. Descriptive study is done on these points.
Review of literature
Bruyn and Bosma support the venous theory of origin. Activities such as straining, bending, coitus, coughing, and sneezing (Valsalva maneuvers) cause increased intrathoracic and intraabdominal pressure. It leads to increase in intravenous pressure since the epidural veins are valveless. The veins are thin walled also. These factors lead to their rupture [1, 3,4,5,6].
Relevant anatomy: Gilbert Breschet described the vertebral venous plexus initially [7]. Later, Oscar Batson emphasized its functional importance. It is longitudinal, large capacitance, and valveless plexiform network of veins. The flow is bidirectional. Blood can flow superiorly or inferiorly depending on pressure gradient [8]. Studies in dogs have shown pressure transmission through the vertebral veins [9]. Although the anterior part of internal vertebral plexus is constant, its posterior part has segmental and individual variability [10]. Radicular veins drain from vertebral veins into segmental and intervertebral veins [11]. Then, the drainage is into large vessels. Superior vena cava receives blood from the cervical area, the azygos and hemiazygos veins from the thoracic region, and the inferior vena cava from the lower.
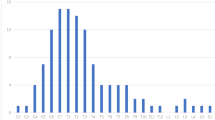
In the case series by Liao et al., 54% of patients reported a straining-associated event during the initial attack, supporting the venous theory [1]. This is especially true in the older patients [2]. They have slow progression of neurological deficits. In patients with liver cirrhosis, the epidural veins would be swollen and thin walled [3]. They can rupture easily producing neurologic deficits. The cumulative effect of gravity causes greater dilatation of the vessels in middle age and thus can predispose to SSEH [5].
Groen and Ponssen had suggested that bleeding arises from the posterior epidural venous plexus, which lies between the dura and ligamentum flavum [12, 13]. The anterior venous plexus is covered by the posterior longitudinal ligament which gives support [5, 12]. The resistance is minimal at the cervicothoracic and thoracolumbar junctions [12]. There, the epidural venous plexus is vulnerable to sudden changes in pressure. In most of the published cases, only venous oozing was seen peroperatively [14]. Bansal et al. reported the occurrence of non-traumatic spinal epidural hematoma in a pregnant woman with HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome [15]. Since pregnancy is a hypercoagulable state, the etiology is not sure. Pregnancy can induce changes in hemodynamics, increasing epidural venous pressure and causing rupture. Okazaki et al. reported a case of chronic SSEH [16]. The hematoma was dark brown and jelly-like. The membrane was adherent to the epidural fat. The venous bleeding from epidural fat was probably the source of bleeding.
The venous theory will not be applicable in the cervical region [1, 2]. The venous pressure is lower than the intrathecal pressure [1, 2]. Secondly, the cervical epidural hematoma usually produces rapid deterioration. Beatty and Winston proposed arterial bleeding as the source in cervical epidural hematomas [1, 3, 4, 17].
Anatomical features: The spinal canal is supplied by the spinal arteries from vertebro-subclavian arteries to thoraco-abdominal aorta [18]. The ventral and dorsal branches of spinal artery supply the bone and dura mater. The radiculomedullary artery supplies the spinal cord. Cadaveric studies have demonstrated cervical radicular arteries from the vertebral, ascending cervical, and deep cervical arteries [19]. The C6 radicular artery was larger. The descending aorta gives off 8 to 10 segmental arteries [20]. The radiculomedullary arteries arise from their posterior branches. The largest anterior radiculomedullary artery is the artery of Adamkiewics. It enters the canal through the intervertebral foramen, passes ventrally, and joins the anterior spinal artery.
The free anastomotic arteries in the epidural space connect with radicular arteries. Rupture of the radicular arteries that run along the nerve roots in the epidural space can cause hematoma [14]. It may be a consequence of trauma or abrupt movements. The rapid development of spinal cord compression is better explained by arterial bleeding [2, 3]. The high mobility of the C6–C7 cervical spine also is a factor [3, 5]. Beatty’s argument was that venous bleeding would not create enough pressure to compress the spinal cord [12]. The intrathecal pressure is higher than the venous pressure [6, 21]. Miyagi et al. favor the arterial source because of this reason [6]. The posterior venous plexus theory could not explain anterior hematomas [12].
Figueroa and DeVine have postulated that SSEH can develop from either rupture of epidural vein, epidural artery, or vascular malformation [5]. They emphasize on the speed of progression of symptoms and the anatomical location. Presence of significant progressive neurological decline suggests arterial source.
Paraskevopoulos et al. reported SSEH from C6/C7 to T2, secondary to extradural arteriovenous malformation in a child [22]. CT and MR angiography are noninvasive and are recently more used in the diagnoses of spinal vascular malformations [23]. Si-Jia et al. reported good spatial and temporal resolution of CT spinal angiography using 64-detector row spiral CT [24].
Emergency decompressive laminectomy is recommended in most of the papers [5, 21, 25,26,27]. Patients with neurologic deficit need urgent surgery. Early surgery leads to greater neurologic recovery [27]. Groen and Ponssen reported better outcomes for patients who underwent decompression within 36 h [13]. Shin et al. opined that early decompression within 12 h restricts the secondary ischemic change, leading to good recovery [28]. Less invasive options such as hemilaminectomy and partial laminectomy are described to evacuate hematoma [3,4,5, 16, 21]. Irrigation can help in hematoma evacuation. Fu et al. reported minimally invasive method using tubular retractors for hematoma extending from T12 to L5 [29]. Iida et al. opined in a series study of postoperative functional radiographic analysis that occurrence of spinal instability was more in cases of wide laminectomy than in cases of partial laminectomy [30].
In patients with coagulopathy, conservative treatment with replacements of clotting factors is preferred [21, 26]. Since in these patients, there is impaired clotting of blood, hematoma will remain in liquid state [28]. Borkar et al. and Sheikh and Abildgaard reported cases of children with hemophilia B who responded to conservative management with factor IX replacement [31, 32]. Kiehna et al. opined in a review that aggressive correction of coagulopathy is a reasonable treatment for hemophilic patients presenting with SSEH, provided neurological condition is stable [33]. Surgery can be avoided if there is no cord compression [21].
Case presentation
Clinical features
A 49-year-old male had a severe thoracic backache of sudden onset. He was a stoneworker. Pain occurred while working on rock. Pain was followed by the weakness of forearm and legs. There were no comorbidities. On examination, he had pain on moving the neck. Forearm and hand muscles were weak and had grade 3 power. He had paraplegia with grade 1 power of lower limbs. He had numbness. All sensations were decreased below nipple. American Spinal Injury Association (ASIA) Impairment Scale was B (incomplete).
Imaging
MRI (magnetic resonance imaging) scan of the cervicothoracic spine was done. It showed posterior convex lesion compressing spinal cord from C3 level to T4 (Fig. 1a, b). It was isointense on T1-weighted and hyperintense on T2-weighted sequence with heterogeneity inside. Fat suppression image was done. MRI was suggestive of epidural hematoma.
Treatment
Methylprednisolone was started. Emergency surgery was done. Long segment midline partial laminectomy and removal of hematoma were done. Laminectomy was done from C5 to T2. Since laminectomy had to be done at many levels, partial laminectomy was done to avoid instability (Fig. 2). Hematoma was removed with suction and irrigation (Fig. 3). No active oozing was noted peroperatively. He slowly improved over 1 week to grade 4+ power. He was discharged on the tenth day in a stage of walking without support. Postoperative MRI showed total evacuation and no instability (Fig. 4).
Follow-up
He was referred for angiography. One hundred twenty-eight-slice CT angiography was done and did not reveal any vascular malformations. He was advised to avoid strenuous works.
Discussion
From the review of literature, we can see that both theories are equally supported. The factors in favor of venous origin are occurrence after strenuous Valsalva maneuvers, thoracic location of hematoma, engorgement of veins in diseases such as cirrhosis, and peroperative demonstration of venous ooze in many cases. The factors in favor of arterial origin are rapid development of spinal cord compression, high mobility of cervical spine, and higher pressure inside theca than veins. In our case, the cervical location and rapid development of weakness point towards arterial origin. Prior stonework could contribute either as strain or by mobility of neck. But the possibility of a burnt-out dural arteriovenous malformation is also there.
Since hematoma can be evacuated through partial or hemilaminectomy, these are the preferred options. These can minimize the chance of instability, as multiple levels have to be opened.
Conclusion
This is a case report of idiopathic spontaneous spinal epidural hematoma. Both views of the source of bleeding, viz. that from epidural veins and that from anastomotic arteries, are supported by authors. Cervical location and rapid development of weakness point towards arterial origin. Thoracic location and presence of peroperative venous ooze suggest venous origin. Early surgical decompression is needed for neurologic recovery. Partial or hemilaminectomy is recommended to reduce postoperative instability. Conservative treatment is preferred in case of coagulopathy.
Availability of data and materials
Data sharing is not applicable.
Abbreviations
- CTA:
-
Computed tomography angiogram
- HELLP syndrome:
-
Hemolysis, elevated liver enzymes, and low platelet count syndrome
- MRI:
-
Magnetic Resonance Imaging
- SSEH:
-
Spontaneous spinal epidural hematoma
References
Gopalkrishnan CV, Dhakoji A, Nair S. Spontaneous cervical epidural hematoma of idiopathic etiology: case report and review of literature. J Spinal Cord Medicine. 2012;35(2):113–7. https://doi.org/10.1179/2045772312Y.0000000001.
Li C, He R, Li X, Zhong Y, Ling L, Li F. Spontaneous spinal epidural hematoma mimicking transient ischemic attack: a case report. Medicine (Baltimore). 2017;96(49):e9007. https://doi.org/10.1097/MD.0000000000009007.
Kim JK, Kim TH, Park SK, Hwang YS, Shin HS, Shin JJ. Acute spontaneous cervical epidural hematoma mimicking cerebral stroke: a case report and literature review. Korean J Spine. 2013;10(3):170–3. https://doi.org/10.14245/kjs.2013.10.3.170.
Aycan A, Ozdemir S, Arslan H, Gonullu E, Bozkına C. Idiopathic thoracic spontaneous spinal epidural hematoma. Case Rep Surg. 2016;2016:5430708. https://doi.org/10.1155/2016/5430708.
Figueroa J, DeVine JG. Spontaneous spinal epidural hematoma: literature review. J Spine Sur. 2017;3(1):58–63. https://doi.org/10.21037/jss.2017.02.04.
Motamedi M, Baratloo A, Majidi A, Rahmati F, Shahrami A. Spontaneous spinal epidural hematoma; a case report. Emergency. 2014;2(4):183–5.
Nathoo N, Caris EC, Wiener JA, Mendel E. History of the vertebral venous plexus and the significant contributions of Breschet and Batson. Neurosurgery. 2011;69(5):1007–14; discussion 1014. https://doi.org/10.1227/NEU.0b013e3182274865.
Waxenbaum JA, Futterman B. Anatomy, back, lumbar vertebrae. In: StatPearls. Treasure Island: StatPearls Publishing; 2018. [Updated 2018 Dec 13].
Guerci AD, Shi AY, Levin H, Tsitlik J, Weisfeldt ML, Chandra N. Transmission of intrathoracic pressure to the intracranial space during cardiopulmonary resuscitation in dogs. Circ Res. 1985;56(1):20–30.
Groen RJ, Groenewegen HJ, van Alphen HA, Hoogland PV. Morphology of the human internal vertebral venous plexus: a cadaver study after intravenous Araldite CY 221 injection. Anat Rec. 1997;249(2):285–94.
DeSai C, Agarwal A. Anatomy, back, vertebral column. In: StatPearls. Treasure Island: StatPearls Publishing; 2018. [Updated 2018 Dec 13].
Fedor M, Kim ES, Ding K, Muizelaar JP, Kim KD. Spontaneous spinal epidural hematoma: a retrospective study on prognostic factors and review of the literature. Korean J Spine. 2011;8(4):272–82. https://doi.org/10.14245/kjs.2011.8.4.272.
Groen RJ, Ponssen H. The spontaneous spinal epidural hematoma. A study of the etiology. J Neurol Sci. 1990;98:121–38.
Muñoz González A, Cuello JP, Rodríguez Cruz PM, Iglesias Mohedano AM, Domínguez Rubio R, Romero Delgado F, García Pastor A, Guzmán de Villoria Lebiedziejswki J, Fernández García P, Romero Martínez J, Ezpeleta Echevarri D, Díaz Otero F, Vázquez Alen P, Villanueva Osorio JA, Gil Núñez A. Spontaneous spinal epidural haematoma: a retrospective study of a series of 13 cases. Neurologia. 2015;30:393–400. https://doi.org/10.1016/j.nrleng.2014.03.005.
Bansal J, Maheshwarappa RP, Gupta A, Goyal A. Non traumatic spinal epidural haematoma in a woman with HELLP syndrome: a case report. J Clin Diagn Res. 2014;8(12):RD06–7. https://doi.org/10.7860/JCDR/2014/10415.5307.
OKAZAKI T, NAKAGAWA H, HAYASE H, et al. Idiopathic and chronic epidural hematoma in the lumbar spine: a case report and review of literatures. Neurol Med Chir. 2018;58(3):138–44. https://doi.org/10.2176/nmc.cr.2017-0052.
Beatty RM, Winston KR. Spontaneous cervical epidural hematoma. A consideration of etiology. J Neurosurg. 1984;61:143–8.
Miyasaka K, Asano T, Ushikoshi S, Hida K, Koyanagi I. Vascular anatomy of the spinal cord and classification of spinal arteriovenous malformations. Interv Neuroradiol. 2001;6(Suppl 1):195–8.
Arslan M, Acar HI, Comert A, Tubbs RS. The cervical arteries: an anatomical study with application to avoid the nerve root and spinal cord blood supply. Turk Neurosurg. 2018;28(2):234–40. https://doi.org/10.5137/1019-5149.JTN.19469-16.1.
Lindeire S, Hauser JM. Anatomy, back, artery of Adamkiewicz. In: StatPearls. Treasure Island: StatPearls Publishing; 2018. [Updated 2018 Dec 6].
Baek BS, Hur JW, Kwon KY, Lee HK. Spontaneous spinal epidural hematoma. J Korean Neuro Soc. 2008;44(1):40–2. https://doi.org/10.3340/jkns.2008.44.1.40.
Paraskevopoulos D, Magras I, Polyzoidis K. Spontaneous spinal epidural hematoma secondary to extradural arteriovenous malformation in a child: a case-based update. Childs Nerv Syst. 2013;29(11):1985–91. https://doi.org/10.1007/s00381-013-2214-5. Epub 2013 Jun 29.
Eddleman CS, Jeong H, Cashen TA, et al. Advanced noninvasive imaging of spinal vascular malformations. Neurosurg Focus. 2009;26(1):E9.
Si-Jia G, Meng-Wei Z, Xi-Ping L, Yu-Shen Z, Jing-Hong L, Zhong-Hui W, et al. The clinical application studies of CT spinal angiography with 64-detector row spiral CT in diagnosing spinal vascular malformations. Eur J Radiol. 2009;71(1):22-8. https://doi.org/10.1016/j.ejrad.2008.04.005. Epub 2008 May 21.
Al-Mutair A, Bednar DA. Spinal epidural hematoma. J Am Acad Orthop Surg. 2010;18(8):494–502.
Duffill J, Sparrow OC, Millar J, et al. Can spontaneous spinal epidural haematoma be managed safely without operation? A report of four cases. J Neurol Neurosurg Psychiatry. 2000;69:816–9.
Lawton MT, Porter RW, Heiserman JE, Jacobowitz R, Sonntag VK, Dickman CA. Surgical management of spinal epidural hematoma: relationship between surgical timing and neurological outcome. J Neurosurg. 1995;83(1):1–7.
Shin JJ, Kuh SU, Cho YE. Surgical management of spontaneous spinal epidural hematoma. Eur Spine J. 2006;15(6):998–1004.
Fu CF, Zhuang YD, Chen CM, et al. Spontaneous spinal epidural hematoma management with minimally invasive surgery through tubular retractors: a case report and review of the literature. Medicine (Baltimore). 2016;95(26):e3906.
Iida Y, Kataoka O, Sho T, et al. Postoperative lumbar spinal instability occurring or progressing secondary to laminectomy. Spine. 1990;15:1186–9.
Borkar SA, Prasad GL, Satyarthee GD, Mahapatra AK. Spontaneous spinal extradural hematoma in a child with hemophilia B, surgery or medical management - a dilemma. J Pediatr Neurosci. 2011;6(2):131–3.
Sheikh AA, Abildgaard CF. Medical management of extensive spinal epidural hematoma in a child with factor IX deficiency. Pediatr Emerg Care. 1994;10:26–9.
Kiehna EN, Waldron PE, Jane JA. Conservative management of an acute spontaneous holocord epidural hemorrhage in a hemophiliac infant. J Neurosurg Pediatr. 2010;6:43–8.
Acknowledgements
I acknowledge the support of Dr. Suhas K.T., M.B.B.S, M.S., M.Ch., D.N.B., Consultant Neurosurgeon, Department of Neurosurgery, Koyili Hospital, Kannur, Kerala, India. PIN-670004. ktsdoc@gmail.com.
Funding
There is no external funding for this article.
Author information
Authors and Affiliations
Contributions
The author treated the patient, collected the data, and prepared the article. The author read and approved the final manuscript.
Author's information
Dr. Ajaya Kumar Ayyappan Unnithan, M.B.B.S., M.S., D.N.B., M.Ch., Consultant Neurosurgeon, Muthoot Hospital, Kozhencherry, Kerala, India.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The approval was gained for publication without revealing identifiable data.
Consent for publication
The patient has given the consent to publish the clinical data in anonymized form.
Competing interests
The author declares that he/she has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Unnithan, A.K.A. A brief review of literature of spontaneous spinal epidural hematoma in the context of an idiopathic spinal epidural hematoma. Egypt J Neurosurg 34, 21 (2019). https://doi.org/10.1186/s41984-019-0046-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-019-0046-7