Abstract
Background
Mild encephalopathy wıth reversible splenial lesions (MERS) are a clinical–radiological diagnosis that can be diagnosed with radiological imaging and can be accompanied by impaired consciousness, aphasia, headache, and paralysis. MERS can be divided into two different types based on radiological findings; Involvement of the splenium is seen in type 1, and involvement of the splenium and deep white matter is seen in type 2. MERS Type 2 is very rare in adults. Here, we describe a patient diagnosed with MERS Type 2 and our therapeutic intervention.
Case presentation
A 22-year-old woman presented with slurred speech, weakness in the extremities and headache that started 14 h ago. The patient had sore throat and fever of 37.6 °C for 2 days, and medical history or family history were unremarkable. Neurological examination revealed that she was conscious, cooperative, with no signs of meningeal irritation. Speech comprehension, naming, and repetition were preserved, motor examination revealed 5/5 left upper extremity strength, 4/5 right upper extremity strength, and 2/5 bilateral lower extremity strength. Diffusion-weighted magnetic resonance imaging (MRI-DWI) revealed bilateral deep white matter and splenium symmetrical diffusion restriction. Blood tests showed high C-reactive protein (CRP) and no leukocytosis. No cells were detected in the cerebrospinal fluid (CSF), protein was 151 mg/dl, glucose was within normal limits. The patient, who developed quadriparesis during follow-up, was started on pulse dose steroids. Neurological examination improved to patient’s baseline at the 12th hour of treatment. In the 72nd hour control MRI-DWI, it was seen that the lesions had regressed. Culture/Polymerase chain reaction (PCR) for bacterial/viral infection agents came back negative. After steroids were given for 5 days, patient was discharged at her baseline.
Conclusions
MERS is a rare diagnosis in adults and can be radiologically confused with acute toxic leukoencephalopathy. It can be distinguished clinically by the absence of prior infection, fever, and toxic agent exposure. Although there is no consensus in the literature regarding the treatment, the clinical picture improved rapidly after steroid in our case. Despite being rare, it should be considered in the differential diagnosis of patients with deep white matter lesions in adults.
Similar content being viewed by others
Background
Acute encephalopathies refer to the sudden onset of impaired consciousness, seizures, and other neurological symptoms and indicate acute brain damage [1]. Causes of acute encephalopathy include febrile encephalopathies (bacterial and viral meningoencephalitis and acute disseminated encephalomyelitis (ADEM)), systemic diseases (hepatic and renal failure, sepsis), hypoxic–ischemic encephalopathies, traumatic brain injuries, toxins, acute toxic leukoencephalopathy (ATL), autoimmune encephalitis and mild encephalopathy with reversible splenial lesions (MERS) [1, 2]. MERS is a newly identified clinical–radiological syndrome is believed to contribute to the pathogenesis of infectious events [3]. MERS is predominantly observed in the pediatric age group, and although rare, cases have been reported in the adult age group [3, 4]. MERS accounts for ~ 16% of all cases of encephalitis in children in Japan [4]. Although there is no clear information on the incidence of MERS in the adult age group in the literature review, it is thought that infectious pathologies frequently contribute to the incidence of MERS [3]. We aimed to present and discuss a patient diagnosed with MERS in adulthood, along with a brief review of the literature.
Case presentation
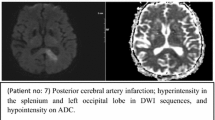
A 22-year-old female patient presented to the Emergency Department with complaints of speech disturbance and weakness in the arms and legs that had started 14 h ago. She reported that her speech improved over a few hours but weakness persisted. The patient had a high fever and sore throat 2 days prior; she was prescribed amoxicillin + clavulanic acid but had not taken it. Vital signs were within normal limits except for a mild fever, 37.6 °C. Neurological examination revealed an alert, oriented and cooperative patient without signs of meningeal irritation. Her speech slightly motor aphasia. During the motor examination, the left upper extremity strength was 5/5, the right upper extremity strength was 4/5, and the bilateral lower extremity muscle strength was 2/5 using the Medical Research Council (MRC) grading system. Diffusion-weighted Magnetic resonance imaging (MRI-DWI) (MAGNETOM Skyra 3 T, Siemens Healthcare, Erlangen, Germany) showed hyperintensity in the deep white matter of bilateral cerebral hemispheres and the splenium of the corpus callosum (Fig. 1A). Apparent diffusion coefficient (ADC) sequences demonstrated symmetric lesions with hypointensity (Fig. 1B) and fluid attenuated inversion recovery (FLAIR) sequences showed hyperintensity (Fig. 1C), with no contrast enhancement observed via contrast imaging. Blood test results revealed a white blood cell count of 8.85 (normal range: 4–10) 10^3/mm3 and a CRP level of 5.84 mg/dl (normal range: 0–0.5 mg/dl). CSF analysis revealed no cells, protein level of 151 mg/dl (normal range: 15–45), an albumin level of 749 mg (normal range: 150–350), and glucose level of 58.40 mg/dl (normal range: 40–70). CSF culture and viral and bacterial meningitis panel results were negative. 1000 mg intravenous pulse steroid (PS) treatment was initiated rapidly after worsening upper extremity muscle strength during the workup. Neurological examination 12 h after steroid treatment showed resolution of tetraparesis and full muscle strength in all extremities. The patient’s headache symptoms completely resolved by the fifth day of admission. Follow-up imaging (HITACHI Echelon 1,5 T, Tokyo, Japan) on the third day showed regression of the lesions (Fig. 2A). Bacterial and viral infection culture and PCR results came back negative. The patient was started on oral methylprednisolone after 5 days of pulse therapy, after which the treatment was gradually tapered and eventually discontinued. The patient was followed up at the first and second month after discharge. At the first and second month follow-up, the patient's neurological examination was found to be normal. In the MRI DWI + FLAIR sequences (MAGNETOM Skyra 3 T, Siemens Healthcare, Erlangen, Germany) taken at the second month (Fig. 3A, ), it was observed that the hyperintensities in the deep white matter and splenium part of the corpus callosum seen at the beginning completely disappeared.
Discussion
MERS, first described by Tada and colleagues in 2004, is a rare clinical–radiological syndrome in which magnetic resonance imaging plays a key role [5]. On characteristic MRI lesions are symmetrically observed as hyperintense on T2-weighted imaging, FLAIR sequences, and diffusion-weighted imaging but hypointense on ADC imaging without showing contrast enhancement [6]. Hyperintensity on diffusion-weighted imaging and hypointensity on ADC imaging indicate cytotoxic edema. It is suggested that the molecular mechanisms responsible for reversible MRI findings observed in MERS cases include intramyelinic edema caused by cytokine storm, which improves with steroid treatment [7, 8]. While MERS predominant presents as a clinical condition affecting the splenium of the corpus callosum, it can rarely present with involvement of the deep white matter [4]. The form in which only the splenium is involved is referred to as Type 1, while the form that also includes the involvement of the deep white matter is called Type 2.
While the majority of MERS cases are observed in the pediatric age group, rare cases have been reported in the adult population [6, 8]. The majority of patients in the pediatric age group have been reported from Japan and East Asia [4]. In the literature, the etiology of MERS is still unclear. The potential causes include viral or bacterial infection, epilepsy, hypoglycemia, antiepileptic drug withdrawal, metabolic disturbance [3, 9]. Among the viral and bacterial triggering factors are influenza virus, rotavirus, mumps virus, adenovirus, Salmonella enteritidis, Escherichia coli O157, Mycoplasma pneumoniae or Legionella pneumophila, and EBV [4, 8, 9]. Regarding the pathogenesis of MERS, there are various hypotheses, including intramyelinic edema, axonal damage, hyponatremia, and oxidative stress. However, there is no clear consensus on the etiology and pathogenesis of MERS [8].
Considering our case from both clinical and radiological perspectives, ADEM and acute toxic leukoencephalopathy (ATL) could be considered in the differential diagnosis. ADEM lesions typically appear asymmetric in the corpus callosum with contrast enhancement, whereas the lesions in our patients were symmetric and lacked contrast enhancement. ATL can be caused by chemotherapeutic agents, immunosuppressive drugs, carbon monoxide, methanol, heroin, cocaine, a history of radiotherapy for head and neck tumors, toluene, antiepileptic drugs (vigabatrin), metronidazole, ethylene glycol, or exposure to heavy metals (lead, cadmium, arsenic) [2, 8, 10]. However, in the case series of ATL evaluated by Özütemiz and colleagues involving 101 patients, the etiology could not be determined in 7 patients [11]. It has been reported that radiologically similar cases to ATL may represent a subtype of ATL, possibly classified as a variant of the condition [12]. The absence of exposure to a potential toxin causing toxic leukoencephalopathy and the presence of prodromal symptoms (fever, headache, sore throat) within the 48 h preceding the onset of symptoms in our patient suggested MERS. As in the case series of 3 cases conducted by Guo and colleagues and other case examples, it was observed that the CSF protein level was high in our case [4, 8].
In the literature, it is seen that Takanashi and colleagues have a series of 54 MERS cases in the pediatric age group, with prodromal symptoms appearing 1–3 days before neurological symptoms in 71% of these cases. Fever was observed in 94% of the cases, and aside from fever, symptoms included cough (12%), diarrhea (15%), and vomiting (25%) [13]. In the adult age group, a literature review by Yuan and colleagues found that 29 patients were diagnosed with adult-onset MERS between 2004 and 2016. Three of these cases were reported from Turkey, and all three were MERS Type 1 cases [8]. No other adult-onset MERS Type 2 cases from Turkey have been reported in the literature.
According to the case series by Takanashi and colleagues, the most common neurological symptom is delusional behavior, observed in 54% of cases, followed by impaired consciousness in 35% and seizures in 33% [13]. In our case, delirium, seizures, or impaired consciousness were not observed, but progressive tetraplegia was noted. At the onset of clinical symptoms, speech impairment was present but resolved, leading us not to consider a pathology related to the cervical cord in our patient. The literature reveals only one case with progressive tetraplegia, and we could not identify another case similar to ours. A case reported from Japan described a 35-year-old male patient who developed progressive tetraplegia and motor aphasia following an Influenza A infection, and similar to our case, pulse steroid therapy was initiated. 12 h after the initiation of pulse steroid therapy, the patient's neurological symptoms had mostly improved [14].
Two cases of familial MERS were reported by Imamura and colleagues, suggesting that genetic factors may play a role in the pathogenesis [15]. There is no consensus on the treatment protocol for MERS. Based on previous studies, PS, antiepileptic, antiviral and IVIG treatments are also used in the treatment [8, 13]. Although the efficacy of methylprednisolone pulse therapy and IVIG on MERS is not definitive, they are recommended for patients with infectious encephalopathy regardless of the pathogen or clinical–radiological syndromes [8]. Although cases of spontaneously resolving MERS have been reported, it has been noted that there is a greater likelihood of neurological sequelae in patients with type 2 involvement [3]. After all there is no complete consensus on the pathophysiology and treatment of MERS, it is very difficult to establish evidence-based treatment in this rare syndrome. In our patient, the fact that there was an increase in protein without cells in CSF examination suggested that there was an inflammatory process in the CNS and therefore, we started PS treatment, which has been previously reported to be given to MERS patients in the literature, and the dramatic improvement in our patient after treatment suggests that PS is effective.
Conclusion
MERS is a syndrome that is rare and should be considered in adults it can cause sequelae and may benefit from PS treatment. The diagnosis should be made based on both radiological and clinical findings, even though the etiology is not fully understood.
Availability of data and materials
We declare that all of the imaging used in this paper are original and belong to Duzce University.
Authors declare possibility to provide data if require.
Abbreviations
- MERS:
-
Mild encephalopathy wıth reversible splenial lesions
- MRI-DWI:
-
Diffusion-weighted magnetic resonance imaging
- ADEM:
-
Acute disseminated encephalomyelitis
- CRP:
-
C-reactive protein
- ATL:
-
Acute toxic leukoencephalopathy
- MRC:
-
Medical Research Council
- ADC:
-
Apparent diffusion coefficient
- FLAIR:
-
Fluid attenuated inversion recovery
- PS:
-
Pulse steroid
- CSF:
-
Cerebrospinal fluid
- PCR:
-
Polymerase chain reaction
References
Kamate M. Acute leukoencephalopathy with restricted diffusion. Indian J Crit Care Med Peer-Rev Off Publ Indian Soc Crit Care Med. 2018;22(7):519–23. https://doi.org/10.4103/ijccm.IJCCM_139_18.
de Rimkus C. Toxic Leukoencephalopathies, including drug, medication, environmental, and radiation-induced encephalopathic syndromes. Semin Ultrasound CT MRI. 2014;35(2):97–117. https://doi.org/10.1053/j.sult.2013.09.005.
Mao X. Adult severe encephalitis/encephalopathy with a reversible splenial lesion of the corpus callosum: a case report. Medicine. 2018;97(26):e11324. https://doi.org/10.1097/MD.0000000000011324.
Guo Y, Wang S, Jiang B, et al. Encephalitis with reversible splenial and deep cerebral white matter lesions associated with Epstein-Barr virus infection in adults. Neuropsychiatr Dis Treat. 2017;13:2085–92. https://doi.org/10.2147/NDT.S135510.
Tada H, Takanashi J, Barkovich AJ, et al. Clinically mild encephalitis/encephalopathy with a reversible splenial lesion. Neurology. 1854;63:10.
Grosset L, Hosseini H, Bapst B, et al. Mild encephalopathy with reversible splenial lesion: description of nine cases and review of the literature. Seizure. 2021;88:83–6. https://doi.org/10.1016/j.seizure.2021.03.032.
Tetsuka S, Ogawa T. Clinically mild Encephalitis/encephalopathy with a reversible Splenial lesion without central nervous system disturbances: a case report. J Gen Fam Med. 2016;17(4):319–22. https://doi.org/10.14442/jgfm.17.4_319.
Yuan J, Yang S, Wang S, Qin W, Yang L, Hu W. Mild encephalitis/encephalopathy with reversible splenial lesion (MERS) in adults-a case report and literature review. BMC Neurol. 2017;17:103. https://doi.org/10.1186/s12883-017-0875-5.
Hibino M, Horiuchi S, Okubo Y, Kakutani T, Ohe M, Kondo T. Transient hemiparesis and hemianesthesia in an atypical case of adult-onset clinically mild encephalitis/encephalopathy with a reversible Splenial Lesion associated with adenovirus infection. Intern Med. 2014;53(11):1183–5. https://doi.org/10.2169/internalmedicine.53.1966.
Makawita C, Ravindra S, Rajapakshe I, Senanayake B. Acute leukoencephalopathy in an adult. Pract Neurol. 2020;20(5):429–32. https://doi.org/10.1136/practneurol-2020-002584.
Özütemiz C, Roshan SK, Kroll NJ, et al. Acute toxic leukoencephalopathy: etiologies, imaging findings, and outcomes in 101 patients. AJNR Am J Neuroradiol. 2019;40(2):267. https://doi.org/10.3174/ajnr.A5947.
Koksel Y, Ozutemiz C, Rykken J, et al. “CHOICES”: an acronym to aid in delineating potential causes of non-metabolic, non-infectious acute toxic leukoencephalopathy. Eur J Radiol Open. 2019;6:243–57. https://doi.org/10.1016/j.ejro.2019.06.005.
Takanashi J. Two newly proposed infectious encephalitis/encephalopathy syndromes. Brain Dev. 2009;31(7):521–8. https://doi.org/10.1016/j.braindev.2009.02.012.
Kimura E, Okamoto S, Uchida Y, et al. A reversible lesion of the corpus callosum splenium with adult influenza-associated encephalitis/encephalopathy: a case report. J Med Case Rep. 2008;2:220. https://doi.org/10.1186/1752-1947-2-220.
Imamura T, Takanashi J. Sisters with clinically mild encephalopathy with a reversible splenial lesion (MERS)-like features Familial MERS? J Neurol Sci. 2010;290(1–2):153–6. https://doi.org/10.1016/j.jns.2009.12.004.
Acknowledgements
Not applicable.
Funding
No funding received.
Author information
Authors and Affiliations
Contributions
All authors participated in the design of the manuscript, collection and review of clinical data, and drafting and writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We confirm that ethical clearance was not required for publication of this case report.
Consent for publication
Written informed consent to publish this information was obtained from patient.
Competing interests
The authors disclose no competing interest in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Şahan, H., Yabalak, A. A case of MERS presenting with acute motor aphasia and tetraparesis and literature review. Egypt J Neurol Psychiatry Neurosurg 60, 97 (2024). https://doi.org/10.1186/s41983-024-00872-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-024-00872-2