Abstract
Background
Anti-N-methyl d-aspartate (NMDA) receptor encephalitis is an autoimmune encephalitis characterized by neuronal surface antibodies targeting NMDA receptor in the spinal fluid and serum. After acute disseminated encephalomyelitis, anti-NMDA receptor encephalitis is the most frequent cause of autoimmune encephalitis. Despite its clinical significance, the exact prevalence and optimal treatment strategies for this condition remain poorly understood. This comprehensive review aims to evaluate the therapeutic potential of bortezomib as a novel therapy for anti-NMDA receptor encephalitis in hopes of mitigating symptoms and improving outcomes for anti-NMDA receptor encephalitis patients.
Results
The disease is primarily triggered by immunoreactivity against the NMDA receptor 1 (NR1). Recurrence rates are of significant concern in the treatment of anti-NMDA receptor encephalitis, given that a substantial portion of patients are unresponsive to immunosuppressive and immunomodulatory therapies. Thus, the exploration of alternative therapies is necessary. In recent years, bortezomib, a proteasome inhibitor, has emerged as a potential therapeutic candidate by inhibiting autoantibody production against NMDA receptor. Bortezomib exerts immunosuppressive and immunomodulatory effects by inhibiting the production of autoantibodies against NMDA receptor. Studies suggest that bortezomib, by inhibiting proteasome activity and altering antigen presentation, can suppress autoantibody production and immune cell activation, contributing to clinical improvement. However, literature reviews on the utilization of bortezomib in the context of anti-NMDA receptor encephalitis are still highly limited.
Conclusions
Bortezomib presents a promising avenue for intervention. While initial studies suggest its potential to modify the immune response and alleviate symptoms, further comprehensive investigations are imperative to establish optimal dosing, usage guidelines, and long-term safety profiles.
Similar content being viewed by others
Introduction
Anti-N-methyl d-aspartate (NMDA) receptor encephalitis is one of the most common autoimmune encephalitis, prompted by immunoreactivity against the NMDA receptor 1 (NR1) subunit of the NMDA receptor. It is defined by the presence of neuronal surface antibodies designed to attack the NMDA receptor in the spinal fluid and serum, as well as sudden onset of disease with multilevel advancement in neuro-psychiatric problems [1, 2]. It was first described in 2007 by Dalmau and colleagues, who discovered psychiatric and neurologic symptoms in women with ovarian teratomas [3]. According to epidemiological research, anti-NMDA receptor encephalitis is the second most prevalent cause of autoimmune encephalitis following acute disseminated encephalomyelitis [4]. There are still no estimates of prevalence rates at this time, but more than 500 cases have been documented [5]. Although existing statistics indicate that the condition is more common in adult women and the non-Caucasian demographic, the disorder has been recorded in both sexes, numerous races, and across the lifetime [6,7,8]. In one study of 100 people with a median age of 23 years, the projected fatality for anti-NMDA receptor encephalitis was 4% [9]. In a recent study conducted by Zhong and colleagues, it was found that the mortality rates for anti-NMDA receptor encephalitis stood at 10%, with older age at onset being a significant risk factor [10]. A study in China quantified the economic burden of autoimmune encephalitis, revealing a mean cost per patient of $14,219, highlighting the substantial impact on healthcare resources and the economy [11]. Moreover, recurrence is a major concern in the course of the illness. Relapses have been documented in 9–23% of patients according to primary literature cohorts after an initial episode of anti-NMDA receptor encephalitis [12]. Patients with NMDA receptor antibody encephalitis have a reduced tolerance for neuroleptic malignant syndrome, and some psychotropic medicines might exacerbate symptoms [13].
Anti-NMDA receptor encephalitis is a complex disorder involving a multiaxial diagnosis. The condition is often asymptomatic and its initial symptoms are not specific. The presence of a tumor or viral infection is the primary cause of anti-NMDA receptor encephalitis. However, patients usually exhibit behavioral and psychiatric symptoms first before other symptoms. Thus, a multidisciplinary approach is necessary to accurately diagnose patients with anti-NMDA receptor encephalitis [14]. Different from other psychiatric disorders, the onset of its psychiatric symptoms is abrupt and there are both negative and positive symptoms, which are more prominent in adults. In children, the disorder most frequently is characterized by the presence of seizures or other movement disorders [15]. It is defined by the presence of neuronal surface antibodies designed to attack the NMDA receptor in the spinal fluid and serum, as well as sudden onset of disease with multilevel advancement in psychiatric or behavioral shifts, dystonia, epilepsy, verbal disorder, awareness and surveillance interruptions and sleep–wake cycle disturbance [1, 2].
As one of several ligand-gated non-selective ionotropic glutamate receptors (iGluRs), NMDA receptors are essential for the fast control of synaptic plasticity involving long-term potentiation and depressive moods which are significant physiological indicators for learning and memory function [16]. Overactive NMDA receptors have been related to neurodegenerative diseases such as Alzheimer’s, while underactive NMDA receptors may play a role in the development of schizophrenia. The receptors have also been linked to a variety of disorders, including depression and epilepsy [17, 18]. Approximately 20–40% of individuals with anti-NMDA receptor encephalitis may have accompanying malignancies, most often teratomas [19, 20]. As a result, not only has immunotherapy been utilized to treat anti-NMDA receptor encephalitis, but also tumor identification and excision [21]. High-dose corticosteroids, intravenous gamma globulin (IVIg), and serum exchange are among the first-line immunotherapies. Second-line immunotherapies such as rituximab and cyclophosphamide have been frequently utilized [19]. Since individuals without tumors are more likely to relapse, it is advised to maintain immunosuppression until at least a year with medications, such as mycophenolate mofetil or azathioprine [22, 23]. Delays in differentiating this condition from a main mental syndrome may have catastrophic repercussions with patients receiving restricted or delayed immunotherapy having a death rate of up to 25% [24]. Inadequate anti-NMDA receptor antibody titer reduction has been linked to therapy resistance. Typically, long-lived plasma cells are resistant to rituximab and other immunosuppressive and B-cell-depleting treatments [25, 26]. Individuals with an aggressive form of the illness may not react to first-line immunotherapy and thus may need other forms of treatment to complement the therapy [27]. However, there are no specific therapy recommendations for patients for whom first- and second-line therapies are unsuccessful [28]. Furthermore, individuals with NMDA receptor antibody encephalitis could be especially susceptible to the extrapyramidal adverse effects of antipsychotic drugs, which might lead to a progression of catatonia or potentially the emergence of neuroleptic malignant syndrome [29]. Prolonged use of corticosteroids can result in a number of undesirable side effects, including osteoporosis, infections, and developmental deficits [30].
The current standard of care for anti-NMDA receptor encephalitis involves immunosuppressive and immunomodulatory therapies, but some patients do not respond to these treatments [31]. It has been observed that a considerable proportion of patients do not exhibit any improvement after receiving the primary mode of treatment [24]. This emphasizes the necessity for therapies that are tailored to different stages of the disease, as well as for new controlled and randomized clinical trials. Bortezomib, a proteasome inhibitor, has emerged as a potential therapy for anti-NMDA receptor encephalitis, targeting plasma cells that produce antibodies against NMDA receptors [32,33,34]. It works by inhibiting the proteasomal degradation of proteins, leading to the accumulation of abnormal proteins and ultimately, apoptosis of targeted cells [35]. In the context of anti-NMDA receptor encephalitis, bortezomib targets plasma cells that produce autoantibodies against NMDA receptors. By inhibiting the production of these autoantibodies, bortezomib may prevent or mitigate the symptoms of anti-NMDA receptor encephalitis [36].
Bortezomib has not been extensively studied in the context of anti-NMDA receptor encephalitis, and the current evidence is limited to case reports and small case series. Therefore, this study represents an important step toward establishing the efficacy and safety of bortezomib in this context. This study offers a promising alternative therapeutic option for these patients, highlighting the importance of personalized medicine in the management of anti-NMDA receptor encephalitis. This study thus sheds light on the pathogenesis of the disease and offers potential therapeutic targets for future research. In light of the recent breakthroughs, the authors are inclined to conduct further investigations into this modality with the objective of improving the prospects of managing anti-NMDA receptor encephalitis more efficaciously.
Methods
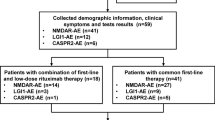
The methodology employed in this review was a systematic literature review. The sources for this review were obtained through extensive searches of PubMed and ScienceDirect databases, utilizing relevant keywords, such as “bortezomib”, “Anti-NMDA Receptor Encephalitis”, and “Neurological Management”. The inclusion criteria for this review were studies that were related to the use of bortezomib in the management of anti-NMDA receptor encephalitis and were published at least 10 years prior without language constraints to the completion of this review. In total, 438 articles were initially identified through the database searches and after rigorous screening and evaluation for credibility and reliability, 96 articles were deemed appropriate for inclusion in this literature review (Fig. 1). The data collected from these articles was analyzed and synthesized to present a comprehensive overview of the current state of knowledge regarding the use of bortezomib in the management of anti-NMDA receptor encephalitis.
Pathophysiology of anti-NMDA receptor encephalitis
Two of the most common triggers of anti-NMDA receptor encephalitis are tumor and post-viral infection [21]. Tumor tissues are arbitrarily arranged to recapitulate or resemble numerous somatic derivations, since they were generated from human embryonic stem cells [37]. Therefore, it was thought that tumor components may include neuroglial cells and neuro-elements, such as NMDA receptors [38]. The NMDA receptor antigen, that is expressed on malignancies or that is released by virally induced neuronal disruption, is either directly transferred in dissolved form to the nearby lymph nodes or is ingested by antigen-presenting cells (APCs), which leads to the production of memory B cells. Naive B cells subjected to NMDA receptor is stimulated and may pass across the blood–brain barrier through the choroid plexus with the assistance of CD4+ T cells [39]. Therefore, the anti-tumor reaction linked to autoimmune encephalitis may be triggered or sustained by neuroglial tissues [40]. Furthermore, it was discovered that tumors associated with anti-NMDA receptor encephalitis had an increased number of dysmorphic nerve cells with irregular cell morphology and large nuclei compared to those without encephalitis, raising the possibility that these dysplastic nerve cells might serve as a source of autoantigens that would lead to anti-NMDA receptor encephalitis [41]. Following their entry into the central nervous system, these activated B cells proceed through additional activation, antigen-driven development, and clonal proliferation before transforming into plasma cells that produce anti-NMDA receptor antibodies [39, 42]. Anti-NMDA receptor antibodies attach to both synaptic and extrasynaptic NMDA receptors. Due to the disruption of the NMDA receptor and ephrin type B2 (EphB2) receptor connection, this causes reduced NMDA receptor and hypoactivity in neurons. However, antibodies may promote synaptic channel permeability prior to internalization, which may account for the seizures [43, 44].
The tumors and viral pathogens express NMDA receptors on their surface (Fig. 2) [45, 46]. NMDA receptors antigens are taken up by APCs after apoptosis. Stimulation, maturation, and multiplication of T cells are induced by the mature dendritic cells’ capture of neural antigens of NMDA receptors and presentation of antigenic components to CD4+ T cells through the major histocompatibility complex (MHC) class II complex [47, 48]. The subsequent differentiation of B cells into plasma cells by activated CD4+ T cells led to the production of immunoglobulin G (IgG) autoantibodies [49]. Autoantibodies subsequently flow in the circulation and pass across the blood–brain barrier into the cerebrospinal fluid. The autoantibodies predominantly damage neurons in the brain's prefrontal cortex and hippocampus through antibody-mediated damage [50]. These autoantibodies attach to the NMDA receptors and cause cross-linking, which changes the surface dynamics of the receptors and impairs their ability to communicate with synaptic proteins [51]. The NR1 subunits of synaptic and extrasynaptic NMDA receptors are bound by anti-NMDA receptor antibodies. NMDA receptor and neuronal excitability are reduced as a result of the disruption of the connection between the NMDA receptor and the EphB2 receptor [52]. NMDA receptor density in synapses decreased as a result of internalization and destruction of NMDA receptors brought on by these antibody-mediated processes [53].
Speculative etiology of anti-NMDA receptor encephalitis associated with tumors or viral infections. Tumors and viruses express NMDA receptors, leading to antigen uptake by antigen-presenting cells after cell death. Mature dendritic cells activate T cells, which induce B-cell differentiation into plasma cells, producing IgG autoantibodies. These autoantibodies damage neurons, mainly in the prefrontal cortex and hippocampus, affecting NMDA receptors. Autoantibodies alter receptor dynamics, impairing synaptic communication. This leads to reduced NMDA receptor density in synapses and decreased neuronal excitability
Current treatments in anti-NMDA receptor encephalitis in humans
A vast number of observational studies and case series reports, including multi-center research, were analyzed to review the treatments of anti-NMDA receptor encephalitis [21]. Several immunotherapies used in anti-NMDA receptor encephalitis are shown in Table 1. Currently, experts recommend phased immunotherapeutic treatments for anti-NMDA receptor encephalitis, with first-line immunotherapy followed by second-line immunotherapy if the first therapy’s response is inadequate [54]. Nevertheless first-line and second-line treatments are still ineffective for 19–33% of autoimmune encephalitis patients, and they continue to experience neurological and psychiatric issues [24, 33]. Hence, for patients with refractory autoimmune encephalitis, novel immunotherapy medicines, also referred to as “third-line therapy,” are progressively being developed [33].
The first-line immunotherapy for anti-NMDA receptor encephalitis includes high-dose corticosteroids, IVIg, or plasma exchange (PLEX), either separately or in combination [55, 56]. Corticosteroids are a type of drug with anti-inflammatory properties that act on intracellular glucocorticoid receptors, obstructing the transcription of numerous pro-inflammatory genes that are activated in chronic inflammatory disorders and also that encode cytokines, adhesion molecules, chemokines, inflammatory enzymes, proteins, and receptors [57]. High doses of corticosteroids can stimulate the production of anti-inflammatory proteins and cause post-transcriptional or postgenomic effects [57, 58]. High-dose corticosteroid treatment is classified as 1000 mg/day of methylprednisolone via intravenous injection for 3–5 days [59]. Large-scale trials confirmed the efficacy of high-dose corticosteroids; nevertheless, the increased rate of secondary infection problems after high-dose corticosteroids were usually overlooked [60]. A recent study has associated the use of high-dose corticosteroids with pneumonia, which results in a longer length of hospital stay (LOS), lower functional outcomes, higher healthcare expenses, and even mortality [59]. Corticosteroids also may potentially cause or worsen psychiatric symptoms of anti-NMDA receptor encephalitis, such as insomnia, depression, agitation, and psychosis, also can be quite challenging to administered in patients with uncontrolled hypertension or diabetes [34].
IVIg is a blood product derived from a pool of plasma collected from over a thousand donors. IVIg produces antibodies against a wide variety of pathogens and is used to give passive protection in patients with immunodeficiency [61]. IVIg is frequently the first line of treatment for patients with medical conditions that exclude the use of corticosteroids, such as uncontrolled hypertension or diabetes, also when there is a worry for active infection [34]. It has anti-inflammatory and immunomodulatory effects by multidirectional pathways, including autoantibody neutralization, blockage of activating Fc-gamma receptors (FcγRs) and induction of inhibitory Fc-gamma receptor IIB (FcγRIIB), suppression of cytokines, complements, and leukocyte migration [62, 63]. IVIg also has fewer side effects than corticosteroids, and is frequently more accessible than PLEX, but in patients with specific immunoglobulin A (IgA) deficiency is associated with the risk of experiencing anaphylaxis, but it is quite rare [34]. Finally, PLEX is a non-selective extracorporeal blood purification process that involves the removal of patient plasma followed by replacement with another solution [34]. PLEX is frequently used in conjunction with or after steroids, rather than as first-line therapy [64]. PLEX can eliminate autoantibodies and other pathogenic chemicals from plasma and also affect the immune system by modifying lymphocyte numbers and distribution, T-helper cell phenotypes, and T-suppressor cell function [65]. The most common complications from PLEX includes pruritus, urticaria, hypertension, and hypotension. However, there are some serious complications that can occur, such as toxic epidermal necrolysis and infection outbreaks, so the use of PLEX should be considered [66].
The second-line immunotherapy for anti-NMDA receptor encephalitis include rituximab and cyclophosphamide if the first-line immunotherapy’s response is inadequate [54]. Rituximab is a partially humanized monoclonal antibody that targets CD20-positive activated and memory B cells, thus inhibiting the germinal centre reaction in anti-NMDA receptor encephalitis [34, 63, 67]. Nevertheless, rituximab is unable to target CD20-negative activated plasma cells, which may prolong the disease course even when first-line and second-line immunotherapies are used [63, 68]. Patients receiving rituximab are more likely to develop infusion reactions and increase risk of infections, such as upper respiratory tract infections and urinary tract infections, especially those with low IgG levels. In addition, it is critical to screen for chronic/latent infections, including hepatitis B and tuberculosis prior to starting rituximab, to avoid disease reactivation. Cyclophosphamide is an alkylating substance that inhibits T- and B-cell growth directly [69]. Unlike rituximab, which cannot penetrate the blood–brain barrier, cyclophosphamide has high bioavailability in the central nervous system and may cause local immunomodulation and immunosuppression. However, because of the possibility for major adverse effects, such as myelosuppression, hemorrhagic cystitis, infertility, and an increased risk of malignancy, it is usually less favored as second-line immunotherapy in anti-NMDA receptor encephalitis than rituximab [34].
The third-line immunotherapy for patients with refractory anti-NMDA receptor encephalitis includes tocilizumab [33]. Tocilizumab is a humanized anti-interleukin-6 (IL-6) receptor antibody created by grafting the complementarily determining sections of a mouse antihuman IL-6 receptor antibody into a human IgG1k to form a human antibody with a human IL-6 receptor binding site, as a result, numerous IL-6-mediated biological functions are inhibited [33]. Tocilizumab also may give additional benefit by targeting antibodies produced by long-lived plasma cells that are not immediately affected by rituximab or cyclophosphamide. However, tocilizumab can elevate the risk of infection and make it more difficult to detect an infection by lowering fever levels and C-reactive protein levels. Therefore, clinicians must be wary of systemic infection in treated patients, particularly those receiving numerous immunomodulatory drugs [34].
Pharmacokinetics and pharmacodynamics of bortezomib
Pharmacokinetics
Bortezomib is a proteasome inhibitor with a high degree of selectivity which is derived from dipeptide boronic acid. Originally, bortezomib was developed for inflammation and cachexia (wasting syndrome) until May 2003 when it became the first anti-cancer proteasome inhibitor that was approved by the Food and Drug Administration (FDA) under the trade name Velcade [70]. The chemical name of bortezomib is [(1R)-3-methyl-1-[[(2S)-1-oxo-3-phenyl-2-[(pyrazinylcarbonyl)amino]propyl]amino]butyl] boronic acid and is available for subcutaneous and injection usage.
In general, administration dose of bortezomib through IV or subcutaneous injection is twice weekly for 2 weeks about 1.0–1.3 mg/m2 with mean maximum concentration (Cmax) ranging from 57 ng/mL up to 112 ng/mL. As a potential second-line therapy, early administration of bortezomib may result in a better outcome as it allows bortezomib to target the plasma cell before crossing the blood–brain barrier as bortezomib capability to penetrate into the central nervous system is poor [32]. In case of anti-NMDA receptor encephalitis, where the patient’s body no longer expresses the cell surface CD20 antigen, the patient's body can absorb bortezomib better by targeting the long-lived plasma cell which mediates the antibody response itself [32]. Bortezomib distributes into nearly all tissues, except for the adipose and brain tissue. Metabolized by hepatic cytochrome P450 (CYP) enzymes, bortezomib’s main metabolic pathway is through the hepatic oxidative boronation which involves the removal of boronic acid from the main compound [71]. Systemic exposure to bortezomib increased by approximately 60% in patients with moderate or severe liver impairment, but not increased in normal and mild symptoms. Thus, it is recommended to reduce the starting dose of bortezomib for patients with moderate or severe liver impairment about 0.7 mg/m2 during the first cycle with escalation dose up to 1.0 mg/m2 and dose reduction to 0.5 mg/m2 adjusting to patient’s drug tolerance [72].
Elimination of bortezomib is mainly done by hepatic route but can also be done by renal route with a mean elimination half-life range from 40 to 193 h following a multiple dosing regimen at a 1.0 mg/m2. While the half-life for multiple dosing of 1.3 mg/m2 bortezomib ranged from 76 to 108 h. Mean total body clearance of the first dose of 1.0 mg/m2 and 1.3 mg/m2 bortezomib were 102 L/h and 112 L/h. While clearances for the next dose are 15 L/h and 32 L/h [71].
Pharmacodynamics
The pharmacodynamics of bortezomib is shown in Fig. 3. Bortezomib primarily inhibits the ubiquitin–proteasome system and nuclear factor-kappa B pathway (NF-kB), leading to plasma cell and activated T-cell apoptosis and the depletion of plasma blast precursors in the bone marrow (30%) [73, 74]. Plasma cell-mediated and antibody-mediated mechanisms are considered to be the cause of anti-NMDA receptor encephalitis in which NMDA receptor antibodies cause disease by internalizing NMDA receptor into neurons [42, 75]. However, postmortem studies revealed that NMDA receptor antibodies are not only produced in the periphery, but resident plasma cells in the perivascular, interstitial, and Virchow–Robin zones in the brain also produce NMDA receptor antibodies [75, 76].
Pharmacodynamics of bortezomib in anti-NMDA receptor encephalitis. Bortezomib primarily inhibits the ubiquitin–proteasome system and the NF-kB pathway, promoting apoptosis in plasma cells and activated T cells. By blocking the 26S proteasome activity, it prevents protein degradation, leading to apoptosis and affecting NF-kB. This influences the immune response by reducing autoreactive B cells and suppressing T-cell activation and proliferation, decreasing pro-inflammatory cytokines such as IL-6 and TNF-α while increasing anti-inflammatory cytokines such as IL-10. In addition, Bortezomib enhances regulatory T-cell activity, preserving immunological tolerance and suppressing autoimmune responses
Based on the pharmacodynamics, bortezomib works by blocking the activity of the 26S proteasome in the ubiquitin–proteasome system, which is responsible for the degradation of proteins within cells [73, 77, 78]. Inhibition of the proteasome leads to an accumulation of misfolded or damaged proteins within the cells, which can cause apoptosis in cells and affecting the NF-kB, a transcription factor that regulates the expression of genes related to immune function and inflammation. It influence immunological response by encouraging the apoptosis of autoreactive B cells and decreasing the activation and proliferation of T cells. Hence, reducing the release of pro-inflammatory cytokines results in anti-inflammatory effects [73, 79]. Recent studies have suggested that bortezomib may alter the immune response by decreasing the production of pro-inflammatory cytokines, such as IL-6 and tumor necrosis factor-alpha (TNF-α), as well as boosting the production of anti-inflammatory cytokines, such as interleukin-10 (IL-10), as a result of the suppression of the NF-kB pathway [80, 81]. Bortezomib also increases regulatory T-cell activity, which is essential for preserving immunological tolerance and preventing autoimmune disorders. As a result, it will lead to the suppression of the autoimmune response [81].
Efficacy of bortezomib in anti-NMDA receptor encephalitis
Several in vivo studies of bortezomib in anti-NMDA receptor encephalitis are shown in Table 2. As anti-NMDA receptor encephalitis is mediated by humoral immunity, treatment targeting B cells and plasma cells are the best option treatment. Usage of rituximab as second-line therapy is suggested before administering bortezomib to counter the CD20 surface antigen which is expressed on B cells. Protracted clinical course of anti-NMDA receptor encephalitis is due to antibody production by long-lived plasma cells. Bortezomib acts as a blocker in the activation of anti-apoptotic NF-kB and activates the terminal unfolded protein response leading to apoptosis which is associated with significant depletion of long-lived plasma cells in peripheral blood and bone marrow [82]. A combination of rituximab and bortezomib shows good results in reducing the production of pathogenic antibodies by reducing the proliferation and differentiation of B cells and plasma cells [82, 83].
For refractory cases of anti-NMDA receptor encephalitis, bortezomib is suggested as it has the ability to target the long-lived plasma cells which cannot be targeted by rituximab and is resistant to antiproliferative agents, such as cyclophosphamide. According to research, a review of bortezomib’s efficacy in anti-NMDA receptor encephalitis patients shows 16 patients (55.2%) of 29 patients had good outcomes. Several side effects were reported in 37.9% of the patients, including hematological problems, infectious, gastrointestinal, neuropathy, and elevated liver enzymes [84]. Bortezomib has been proven to reduce serum anti-NMDA receptor antibodies titer by about 85.7% which shows that bortezomib has a role in reducing the production of peripheral antibodies [84]. Another study also shows bortezomib treatment on anti-NMDA receptor encephalitis patients shows clinical improvement accompanied by reduction of anti-NMDA receptor antibodies titer in 4 of 5 patients [75].
In a case report of a patient with anti-NMDA receptor encephalitis, despite receiving PLEX, rituximab, cyclophosphamide, and high-dose corticosteroids, no clinical improvement was observed. However, the administration of bortezomib was well-tolerated and led to a marked remission in the patient’s condition [85]. In Waldenström’s Macroglobulinemia patients, the addition of bortezomib to the standard optimal treatment resulted in an increase in progression-free survival to 80.6% and an elevated response rate [86]. Furthermore, in a study involving multiple myeloma patients that compared carfilzomib and bortezomib, the bortezomib group exhibited lower mortality rates related to adverse events, anemia, and hypertension [87]. The intervention involving Bortezomib led to improved progression-free survival and event-free survival, with a trend toward improved overall survival compared to interventions that did not include bortezomib. These associations were primarily driven by improved outcomes for high-risk patients [88].
Conclusions
This comprehensive review underscores bortezomib’s therapeutic potential for anti-NMDA receptor encephalitis, showing notable benefits, such as reduced antibody titers, improved neurology, and enhanced autonomic function. Early administration is vital due to its blood–brain barrier limitations. However, limited long-term studies warrant further diverse research for a deeper understanding and validation of bortezomib's role in managing this condition.
Availability of data and materials
Not applicable.
Abbreviations
- IgG:
-
Immunoglobulin G
- IL:
-
Interleukin
- IVIg:
-
Intravenous immunoglobulin
- NF-kB:
-
Nuclear factor-kappa B
- NMDA:
-
N-Methyl d-aspartate
- NR1:
-
N-Methyl d-aspartate receptor 1
- PLEX:
-
Plasma exchange
References
Nosadini M, Granata T, Matricardi S, Freri E, Ragona F, Papetti L, et al. Relapse risk factors in anti-N-methyl-d-aspartate receptor encephalitis. Dev Med Child Neurol. 2019;61:1101–7. https://doi.org/10.1111/dmcn.14267.
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15:391–404. https://doi.org/10.1016/S1474-4422(15)00401-9.
Dalmau J, Tüzün E, Wu H, Masjuan J, Rossi JE, Voloschin A, et al. Paraneoplastic anti-N-methyl-d-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61:25–36. https://doi.org/10.1002/ana.21050.
Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010;10:835–44. https://doi.org/10.1016/S1473-3099(10)70222-X.
Maneta E, Garcia G. Psychiatric manifestations of anti-NMDA receptor encephalitis: neurobiological underpinnings and differential diagnostic implications. Psychosomatics. 2014;55:37–44. https://doi.org/10.1016/j.psym.2013.06.002.
Pollak TA, McCormack R, Peakman M, Nicholson TR, David AS. Prevalence of anti-N-methyl-d-aspartate (NMDA) receptor [corrected] antibodies in patients with schizophrenia and related psychoses: a systematic review and meta-analysis. Psychol Med. 2014;44:2475–87. https://doi.org/10.1017/S003329171300295X.
Kayser MS, Dalmau J. Anti-NMDA receptor encephalitis, autoimmunity, and psychosis. Schizophr Res. 2016;176:36–40. https://doi.org/10.1016/j.schres.2014.10.007.
Tsutsui K, Kanbayashi T, Tanaka K, Boku S, Ito W, Tokunaga J, et al. Anti-NMDA-receptor antibody detected in encephalitis, schizophrenia, and narcolepsy with psychotic features. BMC Psychiatry. 2012;12:37. https://doi.org/10.1186/1471-244X-12-37.
Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008;7:1091–8. https://doi.org/10.1016/S1474-4422(08)70224-2.
Zhong R, Chen Q, Zhang X, Zhang H, Lin W. Risk factors for mortality in anti-NMDAR, anti-LGI1, and anti-GABABR encephalitis. Front Immunol. 2022;13: 845365. https://doi.org/10.3389/fimmu.2022.845365.
Li A, Gong X, Guo K, Lin J, Zhou D, Hong Z. Direct economic burden of patients with autoimmune encephalitis in western China. Neurol Neuroimmunol Neuroinflammation. 2020. https://doi.org/10.1212/NXI.0000000000000891.
Nosadini M, Mohammad SS, Ramanathan S, Brilot F, Dale RC. Immune therapy in autoimmune encephalitis: a systematic review. Expert Rev Neurother. 2015;15:1391–419. https://doi.org/10.1586/14737175.2015.1115720.
Lejuste F, Thomas L, Picard G, Desestret V, Ducray F, Rogemond V, et al. Neuroleptic intolerance in patients with anti-NMDAR encephalitis. Neurol Neuroimmunol Neuroinflammation. 2016;3: e280. https://doi.org/10.1212/NXI.0000000000000280.
Forrester A, Latorre S, O’Dea PK, Robinson C, Goldwaser EL, Trenton A, et al. Anti-NMDAR encephalitis: a multidisciplinary approach to identification of the disorder and management of psychiatric symptoms. Psychosomatics. 2020;61:456–66. https://doi.org/10.1016/j.psym.2020.04.017.
Samanta D, Lui F. Anti-NMDA receptor encephalitis. Treasure Island: StatPearls; 2023.
Kumar A. NMDA receptor function during senescence: implication on cognitive performance. Front Neurosci. 2015. https://doi.org/10.3389/fnins.2015.00473.
Adell A. Brain NMDA receptors in schizophrenia and depression. Biomolecules. 2020;10:947. https://doi.org/10.3390/biom10060947.
Lakhan SE, Caro M, Hadzimichalis N. NMDA receptor activity in neuropsychiatric disorders. Front Psychiatry. 2013;4:52. https://doi.org/10.3389/fpsyt.2013.00052.
Huang X, Fan C, Wu J, Ye J, Zhan S, Song H, et al. Clinical analysis on anti-N-methyl-d-aspartate receptor encephalitis cases: Chinese experience. Int J Clin Exp Med. 2015;8:18927–35.
Wang W, Li J-M, Hu F-Y, Wang R, Hong Z, He L, et al. Anti-NMDA receptor encephalitis: clinical characteristics, predictors of outcome and the knowledge gap in southwest China. Eur J Neurol. 2016;23:621–9. https://doi.org/10.1111/ene.12911.
Huang Q, Xie Y, Hu Z, Tang X. Anti-N-methyl-d-aspartate receptor encephalitis: a review of pathogenic mechanisms, treatment, prognosis. Brain Res. 2020;1727: 146549. https://doi.org/10.1016/j.brainres.2019.146549.
Mann A, Machado NM, Liu N, Mazin A-H, Silver K, Afzal KI. A multidisciplinary approach to the treatment of anti-NMDA-receptor antibody encephalitis: a case and review of the literature. J Neuropsychiatry Clin Neurosci. 2012;24:247–54. https://doi.org/10.1176/appi.neuropsych.11070151.
Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011;10:63–74. https://doi.org/10.1016/S1474-4422(10)70253-2.
Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013;12:157–65. https://doi.org/10.1016/S1474-4422(12)70310-1.
Winter O, Dame C, Jundt F, Hiepe F. Pathogenic long-lived plasma cells and their survival niches in autoimmunity, malignancy, and allergy. J Immunol. 2012;189:5105–11. https://doi.org/10.4049/jimmunol.1202317.
Gresa-Arribas N, Titulaer MJ, Torrents A, Aguilar E, McCracken L, Leypoldt F, et al. Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis: a retrospective study. Lancet Neurol. 2014;13:167–77. https://doi.org/10.1016/S1474-4422(13)70282-5.
Gomes Ferreira M, Lapresa Alcalde V, García Sánchez MH, Hernández Hernández L, Doyague Sánchez MJ. Successful treatment of anti-NMDA receptor encephalitis with early teratoma removal and plasmapheresis: a case report. Medicine (Baltimore). 2018;97: e11325.
Titulaer MJ, Kayser MS, Dalmau J. Prevalence and treatment of anti-NMDA receptor encephalitis—Authors’ reply. Lancet Neurol. 2013;12:425–6. https://doi.org/10.1016/S1474-4422(13)70072-3.
Mohammad SS, Jones H, Hong M, Nosadini M, Sharpe C, Pillai SC, et al. Symptomatic treatment of children with anti-NMDAR encephalitis. Dev Med Child Neurol. 2016;58:376–84. https://doi.org/10.1111/dmcn.12882.
Guang S, Ma J, Ren X, Zhou S, Yang J, Zhang J, et al. Immunotherapies for anti-N-M-methyl-d-aspartate receptor encephalitis: multicenter retrospective pediatric cohort study in China. Front Pediatr. 2021;9: 691599. https://doi.org/10.3389/fped.2021.691599.
Kolls BJ, O’Keefe YA, Sahgal AK. Autoimmune encephalitis: NMDA receptor encephalitis as an example of translational neuroscience. Neurotherapeutics. 2020;17:404–13. https://doi.org/10.1007/s13311-020-00861-2.
Turnbull MT, Siegel JL, Becker TL, Stephens AJ, Lopez-Chiriboga AS, Freeman WD. Early bortezomib therapy for refractory anti-NMDA receptor encephalitis. Front Neurol. 2020. https://doi.org/10.3389/fneur.2020.00188.
Yang J, Liu X. Immunotherapy for refractory autoimmune encephalitis. Front Immunol. 2021. https://doi.org/10.3389/fimmu.2021.790962.
Nguyen L, Wang C. Anti-NMDA receptor autoimmune encephalitis: diagnosis and management strategies. Int J Gen Med. 2023;16:7–21. https://doi.org/10.2147/IJGM.S397429.
Sharma A, Preuss CV. Bortezomib. StatPearls: Treasure Island; 2022.
Masaki RI. Mechanism of action of bortezomib in multiple myeloma therapy. Int J Myeloma. 2016;6:1–6.
Damjanov I, Andrews PW. Teratomas produced from human pluripotent stem cells xenografted into immunodeficient mice—a histopathology atlas. Int J Dev Biol. 2016;60:337–419. https://doi.org/10.1387/ijdb.160274id.
Wu C-Y, Wu J-D, Chen C-C. The association of ovarian teratoma and anti-N-methyl-d-aspartate receptor encephalitis: an updated integrative review. Int J Mol Sci. 2021;22:10911. https://doi.org/10.3390/ijms222010911.
Dalmau J. NMDA receptor encephalitis and other antibody-mediated disorders of the synapse: the 2016 cotzias lecture. Neurology. 2016;87:2471–82. https://doi.org/10.1212/WNL.0000000000003414.
Chefdeville A, Treilleux I, Mayeur M-E, Couillault C, Picard G, Bost C, et al. Immunopathological characterization of ovarian teratomas associated with anti-N-methyl-d-aspartate receptor encephalitis. Acta Neuropathol Commun. 2019;7:38. https://doi.org/10.1186/s40478-019-0693-7.
Jiang X-Y, Lei S, Zhang L, Liu X, Lin M-T, Blumcke I, et al. Co-expression of NMDA-receptor subunits NR1, NR2A, and NR2B in dysplastic neurons of teratomas in patients with paraneoplastic NMDA-receptor-encephalitis: a retrospective clinico-pathology study of 159 patients. Acta Neuropathol Commun. 2020;8:130. https://doi.org/10.1186/s40478-020-00999-2.
Martinez-Hernandez E, Horvath J, Shiloh-Malawsky Y, Sangha N, Martinez-Lage M, Dalmau J. Analysis of complement and plasma cells in the brain of patients with anti-NMDAR encephalitis. Neurology. 2011;77:589–93. https://doi.org/10.1212/WNL.0b013e318228c136.
Planagumà J, Haselmann H, Mannara F, Petit-Pedrol M, Grünewald B, Aguilar E, et al. Ephrin-B2 prevents N-methyl-d-aspartate receptor antibody effects on memory and neuroplasticity. Ann Neurol. 2016;80:388–400. https://doi.org/10.1002/ana.24721.
Mikasova L, De Rossi P, Bouchet D, Georges F, Rogemond V, Didelot A, et al. Disrupted surface cross-talk between NMDA and Ephrin-B2 receptors in anti-NMDA encephalitis. Brain. 2012;135:1606–21. https://doi.org/10.1093/brain/aws092.
Deutsch SI, Tang AH, Burket JA, Benson AD. NMDA receptors on the surface of cancer cells: target for chemotherapy? Biomed Pharmacother. 2014;68:493–6. https://doi.org/10.1016/j.biopha.2014.03.012.
Dale RC, Nosadini M. Infection-triggered autoimmunity: The case of herpes simplex virus type 1 and anti-NMDAR antibodies. Neurol Neuroimmunol Neuroinflammation. 2018;5: e471. https://doi.org/10.1212/NXI.0000000000000471.
Garbi N, Kreutzberg T. Dendritic cells enhance the antigen sensitivity of T cells. Front Immunol. 2012;3:389. https://doi.org/10.3389/fimmu.2012.00389.
Peron JP, Brandão WN, Rossato C, Camara NO. Glutamate ionotropic receptor (NMDAR) modulates T cell survival (IRM7P.712). J Immunol. 2015;194:61.13 LP-61.13.
Choi S-C, Morel L. B cell contribution of the CD4(+) T cell inflammatory phenotypes in systemic lupus erythematosus. Autoimmunity. 2017;50:37–41. https://doi.org/10.1080/08916934.2017.1280028.
Platt MP, Agalliu D, Cutforth T. Hello from the other side: how autoantibodies circumvent the blood-brain barrier in autoimmune encephalitis. Front Immunol. 2017;8:442. https://doi.org/10.3389/fimmu.2017.00442.
Jézéquel J, Johansson EM, Dupuis JP, Rogemond V, Gréa H, Kellermayer B, et al. Dynamic disorganization of synaptic NMDA receptors triggered by autoantibodies from psychotic patients. Nat Commun. 2017;8:1791. https://doi.org/10.1038/s41467-017-01700-3.
De Rossi P, Bouchet D, Georges F, Rogemond V, Didelot A, Meissirel C, et al. Disrupted surface cross-talk between NMDA and Ephrin-B2 receptors in anti-NMDA encephalitis. Brain. 2012;135:1606–21. https://doi.org/10.1093/brain/aws092.
Huang Y-Q, Xiong H. Anti-NMDA receptor encephalitis: a review of mechanistic studies. Int J Physiol Pathophysiol Pharmacol. 2021;13:1–11.
Halliday A, Duncan A, Cheung M, Boston RC, Apiwattanakul M, Camacho X, et al. Second-line immunotherapy and functional outcomes in autoimmune encephalitis: a systematic review and individual patient data meta-analysis. Epilepsia. 2022;63:2214–24. https://doi.org/10.1111/epi.17327.
Zhang X, Wang C, Zhu W, Wang B, Liang H, Guo S. Factors affecting the response to first-line treatments in patients with anti-N-methyl-d-aspartate receptor encephalitis. J Clin Neurol. 2019;15:369–75. https://doi.org/10.3988/jcn.2019.15.3.369.
Sakpichaisakul K, Patibat L, Wechapinan T, Sri-Udomkajrorn S, Apiwattanakul M, Suwannachote S. Heterogenous treatment for anti-NMDAR encephalitis in children leads to different outcomes 6–12 months after diagnosis. J Neuroimmunol. 2018;324:119–25. https://doi.org/10.1016/j.jneuroim.2018.09.007.
González Torre JA, Cruz-Gómez ÁJ, Belenguer A, Sanchis-Segura C, Ávila C, Forn C. Hippocampal dysfunction is associated with memory impairment in multiple sclerosis: A volumetric and functional connectivity study. Mult Scler. 2017;23:1854–63. https://doi.org/10.1177/1352458516688349.
Lozada-Martinez ID, Moscote-Salazar L, Quintana Pájaro L, Florez Perdomo WA, Picón Jaimes YA. The use of corticosteroids in autoimmune encephalitis. Basic and clinical considerations. Rom Neurosurg. 2021;35:192–8. https://doi.org/10.33962/roneuro-2021-030.
Wang J, Lin J, Wang M, Meng Z, Zhou D, Li J. High dose steroids as first-line treatment increased the risk of in-hospital infections in patients with anti-NMDAR encephalitis. Front Immunol. 2021;12: 774664. https://doi.org/10.3389/fimmu.2021.774664.
Chi X, Wang W, Huang C, Wu M, Zhang L, Li J, et al. Risk factors for mortality in patients with anti-NMDA receptor encephalitis. Acta Neurol Scand. 2017;136:298–304. https://doi.org/10.1111/ane.12723.
Shin Y-W, Lee S-T, Park K-I, Jung K-H, Jung K-Y, Lee SK, et al. Treatment strategies for autoimmune encephalitis. Ther Adv Neurol Disord. 2018;11:1756285617722347. https://doi.org/10.1177/1756285617722347.
Galeotti C, Kaveri SV, Bayry J. IVIG-mediated effector functions in autoimmune and inflammatory diseases. Int Immunol. 2017;29:491–8. https://doi.org/10.1093/intimm/dxx039.
Lee W-J, Lee S-T, Shin Y-W, Lee HS, Shin H-R, Kim D-Y, et al. Teratoma removal, steroid, IVIG, rituximab and tocilizumab (T-SIRT) in anti-NMDAR encephalitis. Neurother J Am Soc Exp Neurother. 2021;18:474–87. https://doi.org/10.1007/s13311-020-00921-7.
Nosadini M, Eyre M, Molteni E, Thomas T, Irani SR, Dalmau J, et al. Use and safety of immunotherapeutic management of N-methyl-d-aspartate receptor antibody encephalitis: a meta-analysis. JAMA Neurol. 2021;78:1333–44. https://doi.org/10.1001/jamaneurol.2021.3188.
Reeves HM, Winters JL. The mechanisms of action of plasma exchange. Br J Haematol. 2014;164:342–51. https://doi.org/10.1111/bjh.12629.
Lu J, Zhang L, Xia C, Tao Y. Complications of therapeutic plasma exchange: a retrospective study of 1201 procedures in 435 children. Medicine (Baltimore). 2019;98: e18308. https://doi.org/10.1097/MD.0000000000018308.
Makuch M, Wilson R, Al-Diwani A, Varley J, Kienzler A-K, Taylor J, et al. N-methyl-D-aspartate receptor antibody production from germinal center reactions: therapeutic implications. Ann Neurol. 2018;83:553–61. https://doi.org/10.1002/ana.25173.
Hachiya Y, Uruha A, Kasai-Yoshida E, Shimoda K, Satoh-Shirai I, Kumada S, et al. Rituximab ameliorates anti-N-methyl-d-aspartate receptor encephalitis by removal of short-lived plasmablasts. J Neuroimmunol. 2013;265:128–30. https://doi.org/10.1016/j.jneuroim.2013.09.017.
Kong S-S, Chen Y-J, Su I-C, Lin J-J, Chou I-J, Chou M-L, et al. Immunotherapy for anti-NMDA receptor encephalitis: experience from a single center in Taiwan. Pediatr Neonatol. 2019;60:417–22. https://doi.org/10.1016/j.pedneo.2018.10.006.
Tan CRC, Abdul-Majeed S, Cael B, Barta SK. Clinical pharmacokinetics and pharmacodynamics of bortezomib. Clin Pharmacokinet. 2019;58:157–68. https://doi.org/10.1007/s40262-018-0679-9.
Schwartz R, Davidson T. Pharmacology, pharmacokinetics, and practical applications of bortezomib. Oncology (Williston Park). 2004;18:14–21.
LoRusso PM, Venkatakrishnan K, Ramanathan RK, Sarantopoulos J, Mulkerin D, Shibata SI, et al. Pharmacokinetics and safety of bortezomib in patients with advanced malignancies and varying degrees of liver dysfunction: phase I NCI Organ Dysfunction Working Group Study NCI-6432. Clin Cancer Res an Off J Am Assoc Cancer Res. 2012;18:2954–63. https://doi.org/10.1158/1078-0432.CCR-11-2873.
Fierabracci A. Proteasome inhibitors: a new perspective for treating autoimmune diseases. Curr Drug Targets. 2012;13:1665–75. https://doi.org/10.2174/138945012803530053.
Lazzarin SM, Vabanesi M, Cecchetti G, Fazio R, Fanelli GF, Volonté MA, et al. Refractory anti-NMDAR encephalitis successfully treated with bortezomib and associated movements disorders controlled with tramadol: a case report with literature review. J Neurol. 2020;267:2462–8. https://doi.org/10.1007/s00415-020-09988-w.
Scheibe F, Prüss H, Mengel AM, Kohler S, Nümann A, Köhnlein M, et al. Bortezomib for treatment of therapy-refractory anti-NMDA receptor encephalitis. Neurology. 2017;88:366–70. https://doi.org/10.1212/WNL.0000000000003536.
Foran E, Kwon DY, Nofziger JH, Arnold ES, Hall MD, Fischbeck KH, et al. CNS uptake of bortezomib is enhanced by P-glycoprotein inhibition: implications for spinal muscular atrophy. Neurobiol Dis. 2016;88:118–24. https://doi.org/10.1016/j.nbd.2016.01.008.
Caldeira MV, Curcio M, Leal G, Salazar IL, Mele M, Santos ARA, et al. Excitotoxic stimulation downregulates the ubiquitin–proteasome system through activation of NMDA receptors in cultured hippocampal neurons. Biochim Biophys Acta Mol Basis Dis. 2013;1832:263–74. https://doi.org/10.1016/j.bbadis.2012.10.009.
Wang T, Wang B, Zeng Z, Li H, Zhang F, Ruan X, et al. Efficacy and safety of bortezomib in rituximab-resistant anti-N-methyl-d-aspartate receptor (anti-NMDAR) encephalitis as well as the clinical characteristics: an observational study. J Neuroimmunol. 2021;354: 577527. https://doi.org/10.1016/j.jneuroim.2021.577527.
Alé A, Bruna J, Calls A, Karamita M, Haralambous S, Probert L, et al. Inhibition of the neuronal NFκB pathway attenuates bortezomib-induced neuropathy in a mouse model. Neurotoxicology. 2016;55:58–64. https://doi.org/10.1016/j.neuro.2016.05.004.
Verbrugge SE, Scheper RJ, Lems WF, de Gruijl TD, Jansen G. Proteasome inhibitors as experimental therapeutics of autoimmune diseases. Arthritis Res Ther. 2015;17:17. https://doi.org/10.1186/s13075-015-0529-1.
Shin Y-W, Lee S-T, Kim T-J, Jun J-S, Chu K. Bortezomib treatment for severe refractory anti-NMDA receptor encephalitis. Ann Clin Transl Neurol. 2018;5:598–605. https://doi.org/10.1002/acn3.557.
Kim LN, Edwards L, Goonetilleke N, Kane A, McDougall A, Calic Z. Bortezomib for the treatment of refractory anti-N-methyl-d-aspartate receptor encephalitis. Intern Med J. 2020;50:1591–2. https://doi.org/10.1111/imj.15118.
Sveinsson O, Granqvist M, Forslin Y, Blennow K, Zetterberg H, Piehl F. Successful combined targeting of B- and plasma cells in treatment refractory anti-NMDAR encephalitis. J Neuroimmunol. 2017;312:15–8. https://doi.org/10.1016/j.jneuroim.2017.08.011.
Dinoto A, Cheli M, Bratina A, Sartori A, Manganotti P. Bortezomib in anti-N-methyl-d-Aspartate-Receptor (NMDA-R) encephalitis: a systematic review. J Neuroimmunol. 2021;356: 577586. https://doi.org/10.1016/j.jneuroim.2021.577586.
Behrendt V, Krogias C, Reinacher-Schick A, Gold R, Kleiter I. Bortezomib treatment for patients with anti-N-methyl-d-aspartate receptor encephalitis. JAMA Neurol. 2016;73:1251–3. https://doi.org/10.1001/jamaneurol.2016.2588.
Buske C, Dimopoulos MA, Grunenberg A, Kastritis E, Tomowiak C, Mahé B, et al. Bortezomib-dexamethasone, rituximab, and cyclophosphamide as first-line treatment for Waldenström’s Macroglobulinemia: a prospectively randomized trial of the European consortium for Waldenström’s Macroglobulinemia. J Clin Oncol Off J Am Soc Clin Oncol. 2023;41:2607–16. https://doi.org/10.1200/JCO.22.01805.
Dimopoulos MA, Moreau P, Palumbo A, Joshua D, Pour L, Hájek R, et al. Carfilzomib and dexamethasone versus bortezomib and dexamethasone for patients with relapsed or refractory multiple myeloma (ENDEAVOR): a randomised, phase 3, open-label, multicentre study. Lancet Oncol. 2016;17:27–38. https://doi.org/10.1016/S1470-2045(15)00464-7.
Tan CR, Derkach A, Nemirovsky D, Ciardiello A, Diamond B, Hultcrantz M, et al. Bortezomib, lenalidomide and dexamethasone (VRd) vs carfilzomib, lenalidomide and dexamethasone (KRd) as induction therapy in newly diagnosed multiple myeloma. Blood Cancer J. 2023;13:112. https://doi.org/10.1038/s41408-023-00882-y.
Lee S-T, Lee HS, Lee W-J, Cha H-A, Kim SH, Shin S-Y, et al. The safety and efficacy of intravenous immunoglobulin in autoimmune encephalitis. Ann Clin Transl Neurol. 2022;9:610–21. https://doi.org/10.1002/acn3.51540.
Smets I, Titulaer MJ. Antibody therapies in autoimmune encephalitis. Neurotherapeutics. 2022;19:823–31. https://doi.org/10.1007/s13311-021-01178-4.
Schroeder C, Back C, Koc Ü, Strassburger-Krogias K, Reinacher-Schick A, Gold R, et al. Breakthrough treatment with bortezomib for a patient with anti-NMDAR encephalitis. Clin Neurol Neurosurg. 2018;172:24–6. https://doi.org/10.1016/j.clineuro.2018.06.005.
Cordani R, Micalizzi C, Giacomini T, Gastaldi M, Franciotta D, Fioredda F, et al. Bortezomib responsive refractory anti N methyl d aspartate receptor encephalitis. Pediatr Neurol. 2020;103:61–4. https://doi.org/10.1016/j.pediatrneurol.2019.09.004.
Zhang X-T, Wang C-J, Wang B-J, Guo S-G. The short-term efficacy of combined treatments targeting B cell and plasma cell in severe and refractory Anti-N-methyl-d-aspartate receptor encephalitis: two case reports. CNS Neurosci Ther. 2019;25:151–3. https://doi.org/10.1111/cns.13078.
Keddie S, Crisp SJ, Blackaby J, Cox A, Coles A, Hart M, et al. Plasma cell depletion with bortezomib in the treatment of refractory N-methyl-d-aspartate (NMDA) receptor antibody encephalitis. Rational developments in neuroimmunological treatment. Eur J Neurol. 2018;25:1384–8. https://doi.org/10.1111/ene.13759.
Lazzarin SM, Vabanesi M, Cecchetti G, Fazio R, Fanelli GF, Volonté MA, et al. Correction to: Refractory anti-NMDAR encephalitis successfully treated with bortezomib and associated movements disorders controlled with tramadol: a case report with literature review. J Neurol. 2021;268:741–2. https://doi.org/10.1007/s00415-020-10370-z.
Simmons ML, Perez KA. Bortezomib for treatment of anti-NMDA receptor encephalitis in a pediatric patient refractory to conventional therapy. Am J Heal Pharm AJHP Off J Am Soc Heal Pharm. 2021;78:395–400. https://doi.org/10.1093/ajhp/zxaa415.
Acknowledgements
We thank every party involved in the making of this manuscript. We would like to thank the Department of Neurology, Prof. I.G.N.G. Ngoerah General Hospital for their support. The final text has been read by all of the writers and have all given their consent publication.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
The initial concept for this literature review was hatched by BGL. The text was written by BGL, JCS, MPSE, and LMW with guidance from NMS. BGL, JCS, MPSE, LMW and NMS completed, copyedited and revised the manuscript. CPK and CTS were in charge of revising the manuscript. All authors assisted in reviewing, composing the manuscript, creating the figures and reviewing the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have given their consent for publication.
Competing interests
There is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Liyis, B.G., Sutedja, J.C., Evananda, M.P.S. et al. Bortezomib in the management of anti-NMDA receptor encephalitis. Egypt J Neurol Psychiatry Neurosurg 59, 169 (2023). https://doi.org/10.1186/s41983-023-00765-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00765-w