Abstract
Background
Epilepsy is a network disease and EEG could be used to evaluate dynamic inter-regional connectivity. The aim of the current study is to explore disruption of resting state EEG functional connectivity in focal epilepsy using coherence and phase lag degree. This cross-sectional study included 30 patients with focal epilepsy and 30 matched healthy controls. One to two minutes of EEG segmented into 2-s epochs during awake eye-closed state were analyzed using fast Fourier transform to yield four frequency bands: delta, theta, alpha and beta. Coherence and phase lag degree were computed between each pair of 19 EEG electrodes and were assessed at the intra-hemispheric (frontal–parietal and frontal–temporal) and inter-hemispheric (frontal, temporal and parietal) levels. The frequency of interictal epileptiform discharges (IEDs) was calculated from a 60-min EEG recording session.
Results
Compared to healthy controls, patients had lower theta coherence at left frontal–parietal (P = 0.017), lower delta coherence at inter-frontal (P = 0.045), higher theta phase lag at right frontal–parietal (P = 0.01) and lower delta phase lag at inter-temporal (P = 0.046) levels. Patients with left-sided epilepsy had lower theta coherence at left frontal–parietal (P = 0.026), higher theta phase lag at right frontal–parietal (P < 0.001), higher delta phase lag at right frontal–temporal (P = 0.036) and higher theta phase lag at inter-parietal (P = 0.028) levels. The frequency of IEDs correlated with phase lag of delta (P = 0.036, r = 0.406) and theta (P = 0.005, r = 0.513).
Conclusions
Patients with focal epilepsy had significant interictal functional connectivity disruption detected by coherence and phase lag degree of delta and theta waves and correlated with frequency of IEDs.
Similar content being viewed by others
Background
The human brain is the most complex biological system known, and it was shown that it operates as a system of coupled oscillatory units and multistate dynamic network system. Epilepsy is one of the most complex pathological manifestations of this system [1].
Epilepsy affects more than 50 million people with about one-third of the patients having intractable seizures despite medical management [2]. Epilepsy is now established as a network disease with hyperexcitable neuronal networks [3]. For advancing epilepsy management, it is necessary to understand the pathophysiological basis of epilepsy generation and spread [4, 5].
The gold standard for assessing brain electrical activity is the electroencephalogram (EEG), which measures the brain electrical fluctuations of wide range frequencies with very high temporal resolution. These brain oscillations appear to be coupled both in time and space. The EEG could be recorded during resting wakefulness to measure spontaneous brain fluctuations or with different types of stimulation to provoke any task-related changes in the brain waves [1].
EEG could be used to measure functional connectivity which refers to the statistical interdependence or synchronization between time series of different brain regions. It represents the temporal correlation between spatially remote neurophysiological signals [5]. Among the largely used functional connectivity measures are coherence and phase lag. Coherence assesses linear relation between the amplitude of two signals in the frequency domain, while phase lag measures averaged instantaneous phase differences between two time series [6].
The study of brain connectivity and network characteristics in epileptic patients has many clinical implications. First, it will help to objectively explore pathophysiological mechanisms involved in seizure initiation and propagation which may help in introducing novel therapeutic interventions (pharmacological and non-pharmacological) [5, 7]. Second, theta band functional connectivity was demonstrated as a useful diagnostic tool to predict seizure recurrence in those patients with first unprovoked seizure and normal conventional EEG [8].
Regarding epilepsy management, neurophysiological-derived functional brain connectivity was successfully used to predict patient responsiveness to certain AEDs [9, 10], epilepsy surgery planning [11, 12] and non-invasive localization of epileptogenic zone [13], in addition to its prognostic value to predict seizure and neurocognitive outcome following epilepsy surgery [14, 15]. Disrupted brain networks and functional connectivity in epileptic patients may play a role in the devastating cognitive and neuropsychological affection in those patients [16, 17]. Lastly, connectivity analysis was used in preictal prediction of epileptic seizures using partial directed coherence [18] and automatic seizure detection using effective brain connectivity metrics [19].
A few previous studies have analyzed the resting state EEG functional connectivity of patients with focal epilepsy and the results were somewhat inconsistent regarding specific characterization of the disrupted networks in such patients [10, 20].
In our previous study, we concluded that patients with focal epilepsy had transient dynamic changes in EEG functional connectivity related to the interictal epileptiform discharges (IEDs) [21], however it is unclear if this disruption is persistent in resting brain states regardless of the occurrence of IEDs.
The aim of this study is to explore any significant disruption of resting state EEG functional connectivity in focal epilepsy using coherence and phase lag degree.
Methods
This cross-sectional case control study was performed on 60 individuals (patients and controls of equal number). The study protocol was approved from the local ethical committee of faculty of Medicine, Beni-Suef University and an informed consent was obtained for experimentation with human subjects.
Thirty patients were retrospectively selected from the patient archives fulfilling the following inclusion criteria: a. age older than 16 years, b. patients complaining of focal epilepsy with EEG evidence of focal interictal epileptiform discharges (focal spikes or sharp waves followed by focal slow waves), c. EEG is technically optimum and suitable for selection of sufficient amount of epochs showing awake recordings. Another 30 EEG records were selected from age- and sex-matched healthy controls.
Nineteen gold disc electrodes were placed on the subject’s scalp using electrode paste; according to the international 10/20 system of electrode placement at electrode locations FP1, FP2, F7, F3, FZ, F4, F8, T3, C3, CZ, C4, T4, T5, P3, PZ, P4, T6, O1 and O2, in addition to reference and ground electrodes placed at the forehead and bilateral aural reference electrodes. The impedances of the electrodes were always below 5 kohms.
Raw EEG signals were recorded using Natus, Neurowork EEG system (Nicolet EEG V32 amplifier) with a frequency band of 1–70 Hz. The data were recorded using a sampling rate of 512 Hz.
During the 60-min session of EEG recording, the subject was lying supine during a state of relaxed wakefulness in a silent environment. An EEG technician was following the recording to monitor the signal quality, minimize any eye and muscle artifacts.
EEGs were reviewed visually to extract high-quality recorded segments during awake eye-closed state without any visually screened eye or muscle artifacts and without any visible epileptiform discharges. The total duration of these segments ranged between 4 and 8 min.
The frequency of interictal epileptiform discharges (IEDs) was calculated by counting the number of IEDs divided by the minutes of EEG recording. IEDs were defined according to the operational definition proposed by international federation of clinical neurophysiology (IFCN) which included six criteria: bi- or tri- phasic spikes or sharp waves, asymmetrical, different from background, slow after-wave, disrupted surrounding background activity and corresponding dipole on voltage maps [22].
All participants in the two study groups had their extracted EEG segments imported into the NeuroGuide software (NeuroGuide, Deluxe 3.2.1, 2021, Applied NeuroScience, St. Petersburg, Florida, USA) in department of Clinical Neurophysiology (Neuro-Diagnostic and Research Center), faculty of Medicine, Beni-Suef University. The data were digitally re-sampled at a sampling rate of 256 Hz, filtered at a 1–30 Hz interval, and re-referenced to connected ear reference. Another manual selection procedure was conducted to obtain 2-s epochs with a total duration of 1–2 min of EEG without any visible artifacts. To ensure high-quality selection, split-half reliability and test–retest reliability tests were performed, and only total records with values > 90 and 95%, respectively, were selected for further spectrum analysis [23].
The entire number of selected EEG segments underwent power spectrum analysis utilizing the fast Fourier transform (FFT) with a 25% sliding window approach of Kaiser and Sterman [24]. As a result, each of the 19 recording locations’ average power spectral values for the various frequency bands are produced. Delta (1–< 4 Hz), theta (4–< 8 Hz), alpha (8–12 Hz), and beta (13–25 Hz) were the frequency ranges that were utilized.
Analysis of functional brain connectivity included EEG coherence and phase lag degree. Coherence, which is equal to a squared correlation coefficient, is a measurement of the consistency of phase differences over time. It depends on how many degrees of freedom were utilized to calculate how consistent the phase differences were. It ranges from 1 (constant phase differences in successive epochs) to 0 (random phase differences) [25]
Phase lag is an analytical measure that can be computed for every instant of time between two channels [26]. Absolute phase lag has a (±) sign to denote the direction of the relationship (lead/lag) between the two channels and has a range of 0–180°. But according to other studies, “a simple coherence and phase analysis cannot separate magnitude and direction in the absence of Directed Transfer Functions (DTF) using Multivariate Auto-Regression” [27]. Because of this, the magnitude of the inter-relation was represented by the absolute value of the phase difference rather than its (±) sign.
Using the paired cross-spectrum method to compare each individual EEG channel to each of the remaining 18 channels, EEG coherence and phase lag degree were calculated, producing pairs of inter-electrode values of connectivity measures in the four specified frequency bands.
EEG coherence and phase lag were measured at the intra and inter-hemispheric levels as follows: a. intra-hemispheric (fronto-parietal, F3–P3 and F4–P4 and fronto-temporal, F3–T3 and F4–T4); b. inter-hemispheric (frontal, F3–F4, parietal, P3–P4, and temporal, T3–T4).
G*Power 3.1.9.2 (2014) was used to compute the sample size (t-test) with an 80% study power [28]. The statistical package for social science (SPSS) Version 25.0 was used to analyze the data (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). In order to compare quantitative data, independent t tests or Mann–Whitney U tests were used, as appropriate. Quantitative variables were represented as mean, standard deviation, and 95% confidence interval, or as median and inter-quartile range (IQR), as appropriate.
Chi-square tests were used to compare qualitative variables that were reported as numbers and percentages. Pearson correlation was used to correlate two continuous variables, otherwise Spearman correlation was used. In every test, a P-value less than 0.05 was regarded as significant.
Results
The patient group included 30 patients with focal epilepsy (15 males, their mean age was 28.6 ± 9.6 years). The control group included 30 participants and their ages and sexes were matched to those of the patients (P = 0.94 and 0.796, respectively). Tables 1 and 2 show other clinical and EEG features of the individuals.
The epileptic patients had statistically significant lower coherence of theta frequency at the left frontal–parietal level (P value 0.017) and delta frequency at the inter-hemispheric fontal level (P value 0.045) (Figs. 1 and 2).
The epileptic patients had statistically significant higher phase lag degree of theta frequency at the right frontal–parietal level (P value 0.01) and lower phase lag delta frequency at the inter-hemispheric temporal level (P value 0.046) (Figs. 3 and 4).
The effect of epileptic discharges side on functional connectivity measures was explored by comparing the epileptic patients with left-sided epileptiform discharges with matched controls. The patients had statistically significant lower coherence of theta frequency at the left frontal–parietal level (P value 0.026). (Additional file 1: Figure S1).
Epileptic patients with left-sided epileptiform discharges had statistically significant higher phase lag degree of theta frequency at the right frontal–parietal level (P value < 0.001), delta frequency at right frontal–temporal level (P value 0.036) and theta frequency at the inter-hemispheric parietal level (P value 0.028) (Additional file 1: Figures S2-S4).
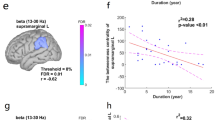
The frequency of epileptic discharges showed significant correlation with phase lag degree of delta (P = 0.036, r = 0.406) and theta (P = 0.005, r = 0.513) frequency over the right hemisphere.
The EEG peak frequency showed significant correlation with alpha coherence at the inter-hemispheric temporal level (P = 0.000, r = − 0.448), alpha phase lag over the left frontal–temporal level (P = 0.038, r = − 0.275) and theta phase lag over the right frontal–temporal level (P = 0.005, r = − 0.388).
No significant correlation was found between age, disease duration and both connectivity measures.
Discussion
This cross-sectional observational study was designed to determine any differences in resting state EEG functional connectivity between patients with focal epilepsy and matched healthy controls, using coherence and phase lag degree measures.
The current study showed significant alterations of functional connectivity in the form of reduced coherence in the patient group at both intra-hemispheric (left frontal–parietal) and inter-hemispheric (frontal) levels. Moreover, the epileptic patients showed higher phase lag degree at both intra-hemispheric (right frontal–parietal) and inter-hemispheric (temporal) levels. Also, the patients with left-sided focal epilepsy showed significantly lower coherence at the intra-hemispheric level (left frontal–parietal) and higher phase lag degree at both intra-hemispheric (right frontal–parietal and frontal–temporal) and inter-hemispheric (parietal) levels. These connectivity alterations were restricted to the delta and theta frequency bands.
Earlier studies have investigated different aspects of disrupted networks and connectivity in patients with focal and generalized epilepsy. Margherita and colleagues found increased global efficiency (measured by partial directed coherence) in patients with focal epilepsy and demonstrated alterations of functional connectivity in whole brain and in specific resting state networks [29].
Furthermore, in their systematic review and meta-analysis, Eric van Diessen and his colleagues concluded the presence of less optimal interictal network organization in patients with focal epilepsy in the form of increased average path length (marker of reduced network integration) and increased average clustering coefficient (more segregated interictal networks). These alterations were more evident in the theta frequency band [30].
At the same time, even in benign focal epilepsy such as Rolandic epilepsy, Hyun-soo choi and his colleagues demonstrated lower weighted phase lag index and longer characteristic path length in lower alpha and beta bands. They concluded decreased connectivity, integration, and efficiency of resting state functional connectivity in these epileptic children [31].
Moreover, Azeez and colleagues reported functional disruption in children with rolandic epilepsy in the form of increased theta, alpha and reduced beta lagged phase synchronization. They proved reduced functional segregation and integration together with loss of local and long-distance functional connections [32].
Unfortunately, the comparison among different connectivity and network studies is not applicable due to wide variation in choice of connectivity measures, network structure and metrics, modality (EEG, MEG, fMRI,…), recording electrodes, and selection of different patient populations [7, 29].
Although there is no clear explanation for the altered connectivity and network disruption in epileptic brains, there are, however, potential pathophysiological mechanisms that could explain such disruption. These include axonal swelling, demyelination, Wallerian degeneration, cortical hypometabolism and cortical neuronal cell death [30, 33].
Whether the seizures cause abnormal connectivity or seizures occur as an epiphenomenon due to altered networks is unclear, however there is emerging evidence that the frequent seizure recurrence leads to detrimental effects on both brain structural and functional integration and may cause disruption of long range subcortical–cortical connectivity [14, 30].
Considering our conclusion ‘in a previous study’ of disruption in EEG functional connectivity in close temporal relation to the occurrence of IEDs [21] and the finding of a connectivity disruption in resting EEG (not including IEDs) in the current study, it seems that these IED-related transient changes accumulate along the disease course into a more persistent connectivity disruption that could be explained by plasticity-related reorganization of epileptic brain networks [33].
The altered connectivity in this study was restricted to the delta and theta frequency bands. This is consistent with the concept of frequency specific epileptic network disruption in previous studies [7, 30, 32]. Theta and delta activity are rhythms that are not present normally in adults during wakefulness, and their presence either visually or even by quantitative spectral and connectivity analysis denotes diffuse grey matter dysfunction in cortical and subcortical areas as well as partial deafferentation of cerebral cortex [34]. These abnormal rhythms were reported to occur in various neuropsychiatric diseases including epilepsy [35].
In the current study, isolated comparison of the left-sided epileptic patients showed similar connectivity alterations to those detected in comparison of the whole patients’ group. Moreover, the coherence and phase lag changes in epileptic patients were bilateral, multifocal and occurred at both intra- and inter-hemispheric levels. This may support the idea of widespread nature of connectivity disruption in epileptic networks which is not restricted to the epileptic focus location [4, 5, 14].
Other studies showed differential impact of the epileptic focus lateralization with greater burden of connectivity changes in left lateralized epilepsies [36]. Moreover, some studies demonstrated that patients with mesial temporal lobe epilepsy had increased connectivity in temporal region and decreased connectivity in frontal and parietal regions outside the zone of epileptogenic focus [37, 38].
In the current study the connectivity measures showed no significant correlation with age and disease duration, however phase lag degree had significant correlation with the frequency of interictal epileptiform discharges pointing to their detrimental effect on the brain networks. Similarly, Eric van Diessen and his colleagues found in their review no significant association between patients age, disease duration and network organization [30]. The rate of interictal epileptiform discharges was found to increase connectivity strength in infantile spasm patients [39].
There are some limitations that should be highlighted. First, the patient population was heterogenous regarding etiology, semiology, disease duration, location of the epileptogenic focus, intake of anti-epileptic drugs (AED) and prognosis. Second, there was no analysis of the possible effects of AEDs on the connectivity measures. Lastly, this study did not include correlation of connectivity measures with neuropsychological and cognitive abilities which are frequently affected in epileptic patients.
Conclusions
Patients with focal epilepsy had significant disruption of EEG resting state functional connectivity detected by coherence and phase lag degree. Such disruption was specific in delta and theta frequency bands and correlated with the frequency of interictal epileptiform discharges.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AED:
-
Anti-epileptic drugs
- DTF:
-
Directed transfer functions
- EEG:
-
Electroencephalography
- FFT:
-
Fast Fourier transform
- fMRI:
-
Functional magnetic resonance imaging
- IEDs:
-
Inter-ictal epileptiform discharges
- IFCN:
-
International Federation of Clinical Neurophysiology
- IQR:
-
Interquartile range
- MEG:
-
Magnetoencephalography
References
Kalitzin S, Petkov G, Suffczynski P, Grigorovsky V, Bardakjian BL, da Silva FL, et al. Epilepsy as a manifestation of a multistate network of oscillatory systems. Neurobiol Dis. 2019;130: 104488.
Duncan JS, Sander JW, Sisodiya SM, Walker MC. Adult epilepsy. Lancet. 2006;367(9516):1087–100.
San-Juan D, Rodríguez-Méndez DA. Epilepsy as a disease affecting neural networks: a neurophysiological perspective. Neurologia (Engl Ed). 2020. https://doi.org/10.1016/j.nrl.2020.06.010.
Bernhardt BC, Bonilha L, Gross DW. Network analysis for a network disorder: the emerging role of graph theory in the study of epilepsy. Epilepsy Behav. 2015;50:162–70.
Stacey W, Kramer M, Gunnarsdottir K, Gonzalez-Martinez J, Zaghloul K, Inati S, et al. Emerging roles of network analysis for epilepsy. Epilepsy Res. 2020;159: 106255.
Van Diessen E, Numan T, Van Dellen E, Van Der Kooi AW, Boersma M, Hofman D, et al. Opportunities and methodological challenges in EEG and MEG resting state functional brain network research. Clin Neurophysiol. 2015;126(8):1468–81.
Kramer MA, Cash SS. Epilepsy as a disorder of cortical network organization. Neuroscientist. 2012;18(4):360–72.
Douw L, De Groot M, Van Dellen E, Heimans JJ, Ronner HE, Stam CJ, et al. ‘Functional connectivity’ is a sensitive predictor of epilepsy diagnosis after the first seizure. PLoS ONE. 2010;5(5): e10839.
Anderson DE, Madhavan D, Swaminathan A. Global brain network dynamics predict therapeutic responsiveness to cannabidiol treatment for refractory epilepsy. Brain Commun. 2020;2(2):fcaa140.
Slinger G, Otte WM, Braun KP, van Diessen E. An updated systematic review and meta-analysis of brain network organization in focal epilepsy: looking back and forth. Neurosci Biobehav Rev. 2022;132:211–23.
Barron DS, Fox PT, Pardoe H, Lancaster J, Price LR, Blackmon K, et al. Thalamic functional connectivity predicts seizure laterality in individual TLE patients: application of a biomarker development strategy. Neuroimage Clin. 2015;7:273–80.
Chiang S, Levin HS, Haneef Z. Computer-automated focus lateralization of temporal lobe epilepsy using fMRI. J Magn Reson Imaging. 2015;41(6):1689–94.
Staljanssens W, Strobbe G, Van Holen R, Keereman V, Gadeyne S, Carrette E, et al. EEG source connectivity to localize the seizure onset zone in patients with drug resistant epilepsy. Neuroimage Clin. 2017;16:689–98.
Englot DJ, Hinkley LB, Kort NS, Imber BS, Mizuiri D, Honma SM, et al. Global and regional functional connectivity maps of neural oscillations in focal epilepsy. Brain. 2015;138(8):2249–62.
Carboni M, Rubega M, Iannotti GR, De Stefano P, Toscano G, Tourbier S, et al. The network integration of epileptic activity in relation to surgical outcome. Clin Neurophysiol. 2019;130(12):2193–202.
Holmes M, Folley BS, Sonmezturk HH, Gore JC, Kang H, Abou-Khalil B, et al. Resting state functional connectivity of the hippocampus associated with neurocognitive function in left temporal lobe epilepsy. Hum Brain Mapp. 2014;35(3):735–44.
Kemmotsu N, Kucukboyaci NE, Cheng CE, Girard HM, Tecoma ES, Iragui VJ, et al. Alterations in functional connectivity between the hippocampus and prefrontal cortex as a correlate of depressive symptoms in temporal lobe epilepsy. Epilepsy Behav. 2013;29(3):552–9.
Zhang Q, Hu Y, Potter T, Li R, Quach M, Zhang Y. Establishing functional brain networks using a nonlinear partial directed coherence method to predict epileptic seizures. J Neurosci Methods. 2020;329: 108447.
Akbarian B, Erfanian A. A framework for seizure detection using effective connectivity, graph theory, and multi-level modular network. Biomed Signal Process Control. 2020;59: 101878.
Bernhardt B, Hong S-J, Bernasconi A, Bernasconi N. Imaging structural and functional brain networks in temporal lobe epilepsy. Front Hum Neurosci. 2013. https://doi.org/10.3389/fnhum.2013.00624.
Elkholy M. Effect of interictal epileptiform discharges on EEG coherence and phase lag in patients with focal epilepsy. Egypt J Med Res. 2023;4(2):7–18. https://doi.org/10.21608/ejmr.2023.198481.1361.
Kane N, Acharya J, Beniczky S, Caboclo L, Finnigan S, Kaplan PW, et al. A revised glossary of terms most commonly used by clinical electroencephalographers and updated proposal for the report format of the EEG findings. Clin Neurophysiol Pract. 2017;2:170.
Thatcher RW, North DM, Biver CJ. Development of cortical connections as measured by EEG coherence and phase delays. Hum Brain Mapp. 2008;29(12):1400–15.
Kaiser DA, Sterman MB. Automatic artifact detection, overlapping windows, and state transitions. J Neurother. 2001;4(3):85–92.
Otnes RK, Enochson L. Digital time series analysis. New York: John Wiley and Sons; 1972.
Oppenheim AV, Schafer RW. From frequency to quefrency: a history of the cepstrum. IEEE Signal Process Mag. 2004;21(5):95–106.
Kaminski MJ, Blinowska KJ. A new method of the description of the information flow in the brain structures. Biol Cybern. 1991;65(3):203–10.
Faul F, Erdfelder E, Buchner A, Lang A. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60.
Carboni M, De Stefano P, Vorderwülbecke BJ, Tourbier S, Mullier E, Rubega M, et al. Abnormal directed connectivity of resting state networks in focal epilepsy. Neuroimage Clin. 2020;27: 102336.
van Diessen E, Zweiphenning WJEM, Jansen FE, Stam CJ, Braun KPJ, Otte WM. Brain network organization in focal epilepsy: a systematic review and meta-analysis. PLoS ONE. 2014;9(12): e114606.
Choi H-S, Chung YG, Choi SA, Ahn S, Kim H, Yoon S, et al. Electroencephalographic resting-state functional connectivity of benign epilepsy with centrotemporal spikes. J Clin Neurol. 2019;15(2):211.
Adebimpe A, Aarabi A, Bourel-Ponchel E, Mahmoudzadeh M, Wallois F. EEG resting state functional connectivity analysis in children with benign epilepsy with centrotemporal spikes. Front Neurosci. 2016;10:143.
Otte WM, van Eijsden P, Sander JW, Duncan JS, Dijkhuizen RM, Braun KPJ. A meta-analysis of white matter changes in temporal lobe epilepsy as studied with diffusion tensor imaging. Epilepsia. 2012;53(4):659–67.
Caviness JN, Hentz JG, Evidente VG, Driver-Dunckley E, Samanta J, Mahant P, et al. Both early and late cognitive dysfunction affects the electroencephalogram in Parkinson’s disease. Parkinsonism Relat Disord. 2007;13(6):348–54.
Steriade M, Gloor PL, Llinas RR, Da Silva FL, Mesulam MM. Basic mechanisms of cerebral rhythmic activities. Electroencephalogr Clin Neurophysiol. 1990;76(6):481–508.
Ridley BGY, Rousseau C, Wirsich J, Le Troter A, Soulier E, Confort-Gouny S, et al. Nodal approach reveals differential impact of lateralized focal epilepsies on hub reorganization. Neuroimage. 2015;118:39–48.
Zhang Z, Lu G, Zhong Y, Tan Q, Liao W, Chen Z, et al. Impaired perceptual networks in temporal lobe epilepsy revealed by resting fMRI. J Neurol. 2009;256(10):1705–13.
Liao W, Zhang Z, Pan Z, Mantini D, Ding J, Duan X, et al. Altered functional connectivity and small-world in mesial temporal lobe epilepsy. PLoS ONE. 2010;5(1): e8525.
Derek KH, Mower A, Shrey DW, Lopour BA. Effect of interictal epileptiform discharges on EEG-based functional connectivity networks. Clin Neurophysiol. 2020;131(5):1087–98. https://doi.org/10.1016/j.clinph.2020.02.014.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ME collected, revised and analyzed the clinical and EEG data. ME performed statistical analysis and prepared the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved from the local ethical committee of faculty of Medicine, Beni-Suef University (Approval number: FMBSUREC/02102022) and in accordance with the principles of Helsinki Declaration and an informed written consent was obtained from all participants before enrollment in the study.
Consent for publication
Not applicable.
Competing interests
The author declares that he has no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Left frontal–parietal coherence of the left-sided epileptic patients and controls. Figure S2. Right frontal–parietal phase lag degree of the left-sided epileptic patients and controls. Figure S3. Right frontal–temporal phase lag degree of the left-sided epileptic patients and controls. Figure S4. Interhemispheric parietal phase lag degree of the left-sided epileptic patients and controls.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elkholy, M.M. Disruption of EEG resting state functional connectivity in patients with focal epilepsy. Egypt J Neurol Psychiatry Neurosurg 59, 122 (2023). https://doi.org/10.1186/s41983-023-00727-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00727-2