Abstract
Background
The thalamus is crucial in the development of idiopathic generalized epilepsy (IGE), which could lead to cognitive dysfunctions, according to data from neuropsychology and advanced neuroimaging investigations. This research aimed to measure the metabolic changes in the thalamus and to assess if could be contributed to cognitive impairment in IGE patients. Thirty IGE patients and thirty healthy volunteers with matched ages, genders, and educational levels participated in this cross-sectional case–control research. The IGE patients and controls were evaluated neuropsychologically using Intelligence Quotient (IQ) to assess general cognitive ability, Digit span for attention, Wechsler memory scale (WMS) for verbal memory, cube drawing test for visuospatial memory, Trail making test for executive functions, and Controlled Oral Word Association test (COWAT) for verbal fluency and quantitative multi-voxel MR spectroscopy (MRS) measurements of N-acetyl aspartate (NAA), choline (Cho), creatine (Cr), NAA/Cr, NAA/Cho and Cho/Cr ratios at 1.5 T scanner. The voxels were located over the right and left thalamus.
Results
The IGE patients showed worse cognitive performance in IQ, attention, executive function, and verbal and visuospatial memory domains compared to the controls. The IGE patients exhibited a significantly decrease NAA in the right thalamus (p = 0.004) and a lower NAA/Cr ratio in the left thalamus (p = 0.01). the mean thalamus NAA level exhibited a positive correlation with CDT (r = 0.45, p = P = 0.01), and WMS-R (r = 0.39, p = 0.03) and a negative correlation with trail-making A test (r = 0.42, P = 0.01).
Conclusions
it was concluded that IGE patients exhibited poor cognition which could be attributed to thalamic neurometabolic changes due to impaired thalamic cortical circuits.
Similar content being viewed by others
Introduction
Idiopathic generalized epilepsy (IGE) is a frequent and complicated disorder with a genetic background and varying phenotypes [1]. The International League Against Epilepsy (ILAE) Classification of Epilepsies defined idiopathic generalized epilepsies (IGEs) to be applied for the heterogeneous class of epilepsies with generalized seizure forms and generalized spike-wave in 2017 [2]. This categorization was based on evidence from twin and family research studies that suggested a possible genetic cause. IGE affects 15–20% of people with epilepsy and is divided into 4 syndromes: childhood absence epilepsy (CAE), juvenile myoclonic epilepsy (JME), juvenile absence epilepsy (JAE), and epilepsy with generalized tonic–clonic seizures alone (GTCA) [3].
Previous human imaging studies had revealed strong evidence of structural malformations and thalamic dysfunction in IGE. The hydrogen proton magnetic resonance spectroscopy (1H-MRS), was employed to identify subtle alterations in neuronal density in patients with macroscopically normal brains [4], had documented metabolic alterations mainly found in the thalamic and prefrontal N-acetyl aspartate (NAA) levels in patients with IGE [5]. These neurochemical changes are thought to be a reflection of thalamocortical impairment. which could be related to neuropsychological impairment in IGE patients [6]
Although IGE has traditionally been thought of as a benign condition, studies have frequently postulated that executive functioning in IGE may be compromised. Patients with IGE frequently experienced memory deficits such as difficulty recalling commonplace items such as phone numbers, household duties, messages to pass on, and even difficulty recognizing familiar people [7]. The goal of this research was to explore the pattern of cognitive impairment in patients with IGE and determine whether these impairments might be related to the neurochemical alterations in the thalamus by using MR spectroscopy.
Methods
This is a cross-sectional case–control study that was done on 30 Egyptian patients with an IGE diagnosis according to the clinical guidlines based on the International League Against Epilepsy, 2017 [2] with ages ranging from 18 to 39 years. For a comparison of psychometric and neuroradiological data, thirty healthy volunteers who were age, sex, and educationally matched were chosen as the control group. Eligible patients were enrolled in the period from June 2020 to October 2021. Both the patient and control groups gave their written approval to take part in the research.
Patients who received tricyclic antidepressants and/or typical antipsychotic medications that interfered with the psychometric evaluation or had a concurrent neurological or psychiatric illness were excluded from the study. In order to avoid post-ictal confusion, which would impair cognitive function, patients who had generalized seizures in the previous week or myoclonic, absence seizures on the previous day, were also not included in this study [6]. Since they were regarded as absolute contraindications for MRI exposure, individuals with devices or metal foreign bodies including pacemakers, defibrillators, cochlear, and dental magnetic implants were also left out of the study.
The IGE patients who participated in this research had full neurological examination and history taking from their families including factors such as the age at which seizures first began, the duration of the condition, the frequency of fits (the number of fits per month), the semiology of seizures, presence of status epilepticus, and the history of antiepileptic medications received.
All the patients and the control groups underwent the following battery of psychometric evaluations including Intelligence Quotient (IQ) to assess general cognitive ability by using Stanford-Binet Intelligence Scales (SB5)—[8]. Digit Span test(DST) was used to evaluate selective attention [9], and the Cube drawing test (CDT) to assess Visuospatial functions. The task consisted of copying a three-dimensional printed cube of size 2.5 cm3 and the scoring system was proposed by [10]. The Weschler memory scale-Revised (WMS-R) was used to evaluate verbal memory, which is defined as the ability to learn and remember information presented verbally. The verbal memory test is a combination of the Logical Memory 1 test and the Verbal Paired Associates I of the WMS-R [11].
The Trail Making Test (TMT) [12] with an Arabic form [13] was used to measure executive functioning. Furthermore, the Arabic form of the Controlled Oral Word Association Test (COWAT) [14] was utilized to assess verbal fluency; the language part of the executive function.
All patients included in this study had an electroencephalogram (EEG) performed at Fayoum University Hospital's neurology department. EEG electrodes were set according to 10–20 system recordings with 32-channel Nihon Kohden equipment from Japan. EEG was recorded under conventional settings with hyperventilation and photic stimulation as stimuli. The EEG data were analyzed for background activity and the presence of epileptogenic activity.
All epileptic patients underwent magnetic resonance imaging (MRI) with epilepsy protocol, which included imaging the entire brain from the nasion to the inion to rule out subtle and mild structural abnormalities. The results of 1.5 Tesla magnetic resonance brain scans performed using a Toshiba Scanner Activion, Japan, were examined by the radiology department. The following pulse sequences were obtained using the epilepsy protocol according to the International League Against Epilepsy (ILAE) recommendations for neuroimaging in patients with epilepsy (2019) [15]. Axial T1 weighted images of 1.5 mm slice thickness were acquired in the coronal oblique plane without any gaps in between. Coronal and axial FLAIR sequences with slice thicknesses ranging from 2 to 3 mm and an interslice gap of 0–1 mm.
Both the patients and control groups underwent multivoxel MR spectroscopy (MRS) of the bilateral thalamus. The multivoxel approach allows for the placement of several voxels in the brain, allowing the synchronized study of metabolic changes in a broad range of microscopic volume units inside the structure and illustrating the magnitude of these metabolic alterations [16].
The outputs of the computer software processing of the gathered spectral data were evaluated using the area under the curve of metabolite peaks. The metabolite concentrations for N-acetyl aspartate (NAA), choline (Cho), and creatine (Cr) were estimated in absolute units of mmol/L using the MRS spectrum analysis (mM). The data for metabolite concentrations were examined using the free nuclear magnetic resonance-spectra calculation [17].
It is considered that N-acetyl aspartate (NAA) is a measure of neuronal/axonal density and vitality. NAA is recognized as an objective indicator of neuronal dysfunction or loss. In MRS, creatine (Cr) serves as an internal reference. Since Cr is thought to be a rather stable substance, concentrations of other brain metabolites are linked to it. The Cr peak serves as a biomarker for the density of glial and neuronal cells in the brain. Cell membranes and myelin are the two main components of choline (Cho). Cho is a sign of damaged membranes. Increased Cho might be a sign of gliosis or myelin damage. Different spectroscopic measures, including NAA, Choline, and Creatine levels, as well as spectroscopic ratios for the thalamus, including NAA/Cr, NAA/Cho, and Cho/Cr ratios, were measured and computed [18].
Statistical analysis
Version 22 of the Statistical Package for Social Science (SPSS) (SPSS Inc., Chicago, IL, USA) software was used for data assessment. Simple descriptive analysis in the form of qualitative data numbers and percentages, as well as arithmetic means and standard deviations. The Independent samples t-test was used to compare two separate groups for quantitative parametric data, while the One-way ANOVA test was applied to compare more than two independent groups. The Kruskal–Wallis test was applied to quantitative nonparametric data, the Mann–Whitney test was utilized to compare two independent groups. A Chi-square test was used to compare more than two qualitative groups. A Pearson correlation test was used to examine the relationship between variables. The P-value < 0.05 was supposed statistically significant.
Based on prior research [19], the sample size was determined using open Epi, with the following presumption. 90% power, 95% confidence interval, and at least 20 people per group.
Results
The clinical and demographic features of the patients and control were shown in Table 1. The distribution of different IGE syndromes among the cases was illustrated in Fig. 1 and all the epileptic (100%) patients showed interictal epileptiform activity in the form of generalized spikes and slow complexes lasting 2–5 HZ/s in the EEG study.
The epileptic patients performed worse than the control group in general cognitive abilities, attention, executive functions, verbal memory, and visuospatial functions assessed by IQ, DST, trail-making B, WMS-R, and CDT tests respectively with (p = 0.003, 0.001, 0.003, 0.02, < 0.001, and 0.02, respectively) as shown in Table 2.
Concerning the MR spectroscopy results, it was found that epileptic patients showed a significantly lower NAA level in the right thalamus (13.3 ± 3.5) than the control group(15.6 ± 2.2) (p = 0.004)as shown in Fig. 2. Additionally, the NAA/Creatine ratio was significantly lower in the left thalamus (1.8 ± 0.71) of the epileptic patients than in the control group (2.4 ± 1.3) (p = 0.01). Otherwise, there was no significant difference in the other parameters as shown in Table 2.
Multivoxel spectroscopy of the thalamus of 18 years old male patient with childhood absence epilepsy, T2 weighted image in the axial plane. Placement of the volume of interest over the right and left thalami. It was shown a reduced N-acetyl aspartate and N-acetyl aspartate/creatine ratio in the right thalamus
As regard the effect of antiseizure medications (ASM) on the cognitive performance of epileptic patients, it was shown that the patients receiving polytherapy (117.6 ± 14.5) had worse performance in executive function than those receiving monotherapy(Na valproate) (104.8 ± 11.8) (p = 0.01). Otherwise, no significant difference in the other cognitive domains between the two groups. Moreover, no significant difference was found in MRS results between the two groups as shown in Table 3.
By comparing the different IGE syndromes in psychometric tests, it was shown that the CAE syndrome had the worst performance in attention (6 ± 0.82) assessed by DST versus JAE (6.8 ± 0.46), JME (7.3 ± 0.89) and GTCA (7.5 ± 1.2) (p = 0.04). Otherwise, no significant difference was found in the other cognitive domains. Moreover, there was no significant difference was found in MRS parameters between the different syndromes.
The age of the epileptic patients had a significant negative correlation with choline of the mean thalamus (r = − 0.47, p = 0.009) and a substantial positive correlation with NAA/Choline ratio (r = 0.42, p = 0.01). Otherwise, there was no significant correlation between the patients' ages, frequency of seizures, and duration of illness with the other biochemical alterations in the thalamus or the psychometric assessments.
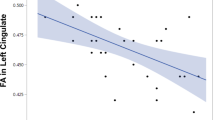
Furthermore, the mean thalamus NAA level exhibited a positive correlation with CDT (r = 0.45, p = P = 0.01), and WMS-R (r = 0.39, p = 0.03) and a substantial negative correlation with trail-making A test (r = 0.42, P = 0.01). Furthermore, there was a significant positive correlation between the NAA/choline ratio of the mean thalamus and CDT (r = 0.39, p = P = 0.03) as shown in Fig. 3.
Discussion
In the past ten years, there has been a rise in the amount of research on the cognitive features of IGE patients, with JME being the primary focus of most investigations. The goal of the present study is a thorough evaluation of cognitive performance in IGE patients with a group of mixed syndromes.
Children with epilepsy who have cognitive impairment are at higher risk of having less academic success. In addition, adult individuals who suffered from childhood epilepsy with cognitive issues had a greater risk of unemployment than those with childhood epilepsy without cognitive issues [20]. It was observed in the current study that IGE patients had lesser IQ scores than the control group despite they being of the normal average range, in concordance with these results [21, 22] reported decreased general intelligence in IGE in comparison to controls, with the reported IQ tests for IGE patients clustered around typical population values, between 90 and 110. Therefore, it is yet unknown if general intellectual capacities in IGE may be below normative levels or whether discrepancies between patient and control samples may result, for example, from the enrollment of high-performing, nonrepresentative control groups in several research studies [23].
It was shown in this study that the patients with IGE had a significantly poor performance of attention, executive function, verbal memory, and visuospatial memory than the control group, as regards verbal fluency, the IGE patients had worse performance than the control, but it did not reach to a significant level. These findings were consistent with earlier studies on this subject as Chowdhury et al. [24]. as well as Loughman et al. [25] found that IGE patients particularly those with childhood absence epilepsy performed noticeably worse than controls in working memory, attention, and nonverbal reasoning.
It was hypothesized that the IGE patients had worse scores in cognitive processing speed, attention, and working memory than the healthy control group, as well as to a lesser extent in short-term memory and long-term memory retrieval. Working memory deficits are less well tolerated than impairments in other cognitive domains, which may explain why self-reported memory symptoms are frequently reported in response to a decline in working memory [26]. Cognitive dysfunction in IGE is most probably attributed to neurodevelopmental delays which were emphasized by some research that had shed light on outlining first-order relatives along with index patients to describe the cognitive phenotypes of IGE subgroups and discover family features with putative genetic origins. Active epilepsy causes abnormal neurodevelopmental changes in the structure and interconnection of the brain, resulting in structural abnormalities mostly in subcortical areas, including thalamocortical networks [27].
Magnetic resonance spectroscopy (MRS) is a noninvasive method for identifying brain metabolites. Multivoxel MRS allows for simultaneous analysis of a broad range of microscopic volume units, as well as demonstrating the extent of metabolic abnormalities within the structure. Magnetic resonance spectroscopy (MRS) investigations have supported thalamic participation in IGE since neurochemical abnormalities are thought to represent thalamocortical dysfunction, which is thought to be a pathophysiologic basis for IGE [17].
N-acetyl aspartate (NAA) is an indicator of axonal or neuronal density, and viability, any decline in NAA or its ratio to Cr and Cho is supposed to be a sign of neuronal death or damage [17]. In the current study, it was found that IGE patients had significantly lower NAA values in the right thalamus as well as a lower NAA/Creatine ratio in the left thalamus compared to the control group. These findings were somewhat consistent with [17, 28, 29], who reported considerably reduced NAA and NAA/cr ratio in both thalami. The contradictory MRS results in the literature regarding the laterality of thalamic impairment, which affects either the right or left thalamus in IGE patients, could be attributed to the fact that MRS parameters were impacted by numerous factors such as changes in data gathering, post-processing techniques such as single voxel or multivoxel spectroscopy or employing a high resolution 3 T MRI, the age and duration of epilepsy of the patients who participated in these studies.
Some evidence had emphasized that the neural activity of the thalamus in IGE patients was implicated in the generation of seizures in this form of epilepsy. The electrophysiological experiments had postulated centrencephalic and corticoreticular theories had been involved in the pathophysiology of IGE, whereas the pathological changes were primarily present in the thalamic nuclei, or that thalamic ascending impulses impact a diffusely hyperexcitable cortex [30]. MRS studies had shown that the thalamic NAA reduction could be a result of cell damage, excitotoxicity, or both. Another hypothesis is that the IGE patients’ dystopic thalamus neurons were more vulnerable to seizures, leading to a significant decline in neuronal density [31]. It was considered that the thalamus metabolites (NAA, Cr, NAA/Cr values) are the most applicable diagnostic indicators for distinguishing IGE patients from healthy persons despite no structural impairment present in the conventional MRI images [17].
The recent structural and functional neuroimaging modalities had demonstrated widespread changes in cortical and subcortical organization, functioning, and interconnectivity. which could be associated with cognitive dysfunction. In this study, it was shown that the level of NAA of the thalamus was correlated to verbal, and visuospatial memory as well as executive function. In concordance with Savic et al. [32] reported poor executive function performance of JME patients who had decreased NAA levels as well as Simani et al. [28] found that NAA levels and NAA/Cr ratio in bilateral thalamic and prefrontal regions were lower than the controls which were positively correlated to neuropsychological performance and were not linked with the disease duration.
Concerning the effect of antiseizure medications, this study found that IGE patients receiving poly antiepileptic therapy (valproate, levetiracetam, or lamotrigine combinations) had a worse impact on executive functions than IGE patients receiving valproate monotherapy, with no significant difference in other cognitive domains. According to Witt et al. [33], several ASMs, including levetiracetam, topiramate, zonisamide, and valproate, seem to impair all cognitive functions, particularly attention, executive function, and memory function. Any combination of these ASMs also tends to increase cognitive dysfunctions. Increased GABAergic activity in the prefrontal cortex, which may result in mental slowness and executive dysfunction, is the mechanism through which polytherapy antiepileptic medications may induce cognitive impairment. and switching to monotherapy or fewer ASMs typically results in cognitive improvement [34]. The conflict of seizure control versus side-effect management is a common challenge to clinicians seeking to address the adverse effects of ASM and optimize patient welfare.
Veenendaal et al. [35] reported that ASMs exert their anticonvulsant properties by affecting the excitatory and inhibitory neurotransmitter systems (GABA and glutamate concentrations), primarily with a minor effect on concentrations of other metabolites as (NAA, Cre), and that supported our results that there was no significant difference between the patients who had been treated with either monotherapy or polytherapy ASM in this study. Moreover, Ramirez-García et al. [36] found no change in NAA and creatine concentrations in patients taking valproate compared with patients taking other ASMs.
It was postulated that the duration of epilepsy is very variable as it is dependent on the age of the patient as well as the age of the onset of the disease, it was discovered that increasing the age of the patient or increasing the age of the onset is associated with decreased thalamic NAA/Creat or NAA/Choline ratio which indicated an advanced thalamic neuronal loss in patients with IGE [28]. This notion supported our results as it was found negative correlations between the age of patients and choline level, and positive correlations with NAA/choline ratio, with no significant correlations, were found between the other clinical data and MRS parameters. the lack of correlations between the duration of epilepsy and MRS parameters is explained that the onset of epilepsy in our study started later in childhood and early adolescent period with a relatively shorter duration of epilepsy.
Some studies in JME sought to link up the potential substrates of epileptogenesis, which are most probably characterized by fronto-thalamo-cortical circuitry with certain cognitive functions. O'Muircheartaigh [37] showed abnormal fronto-cortico-thalamic function and connection in JME during an fMRI task demonstrating verbal memory defect. Corresponding evidence was offered by a structural imaging evaluation in IGE patients, which demonstrated a relationship between executive function performance and both frontal and thalamic volumes [38], this research hypothesized that the same circuit responsible for seizure generation in IGE may similarly mediate executive function impairment.
Conclusion and recommendation
Finally, it was concluded that IGE patients exhibited poor cognitive performance in certain cognitive domains such as general cognitive abilities, attention, verbal memory, visuospatial function, and executive functions compared to controls which could be attributed to thalamic neurometabolic changes due to impaired thalamic cortical circuits.
Limitation
One of the study's weaknesses was the relatively small number of IGE patients with different syndromes, which made it challenging to characterize the selective cognitive pattern in each syndrome relative to the control group and analyze the effects of seizure control on the thalamic biochemical alterations. Moreover, one of the main drawbacks of this research is the fact that cortical biochemical alterations or cortical atrophy, which may have an impact on patients with IGE's cognitive performance, were not examined.
Availability of data and materials
The dataset cannot be publicly available due to institutional rules. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. The figures used in this manuscript are original.
Abbreviations
- ASM:
-
Anti-seizure medication
- 1H-MRS:
-
Hydrogen proton magnetic resonance spectroscopy
- CAE:
-
Childhood absence epilepsy
- CDT:
-
Cube drawing test
- Cho:
-
Choline
- COWAT:
-
Controlled oral word association test
- Cr:
-
Creatine
- DST:
-
Digit span test
- EEG:
-
Electroencephalogram
- GGE:
-
Genetic generalized epilepsies
- GTCA:
-
Generalized tonic–clonic seizures alone
- IGE:
-
Idiopathic generalized epilepsy
- ILAE:
-
International League Against Epilepsy
- IQ:
-
Intelligence quotient
- JAE:
-
Juvenile absence epilepsy
- JME:
-
Juvenile myoclonic epilepsy
- NAA:
-
N-Acetyl aspartate
- TMT:
-
Trail making test
- WMS:
-
Wechsler memory scale
References
Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1989;30(4):389–399.
Fisher RS, Cross JH, French JA, Higurashi N, Hirsch E, Jansen FE, et al. Operational classification of seizure types by the international league against epilepsy: position paper of the ILAE commission for classification and terminology. Epilepsia. 2017;58(4):522–30.
Hirsch E, French J, Scheffer IE, Bogacz A, Alsaadi T, Sperling MR, et al. ILAE definition of the idiopathic generalized epilepsy syndromes: position statement by the ILAE task force on nosology and definitions. Epilepsia. 2022;63(6):1475–99.
Hammen T, Stefan H, Eberhardt KE, W-Huk BH, Tomandl BF. Clinical applications of 1H-MR spectroscopy in the evaluation of epilepsies—what do pathological spectra stand for with regard to current results and what answers do they give to common clinical questions concerning the treatment of epilepsies? Acta Neurol Scand. 2003;108(4):223–38.
Bernasconi A, Bernasconi N, Natsume J, Antel SB, Andermann F, Arnold DL. Magnetic resonance spectroscopy and imaging of the thalamus in idiopathic generalized epilepsy. Brain. 2003;126(Pt 11):2447–54.
Cevik N, Koksal A, Dogan VB, Dirican AC, Bayramoglu S, Ozturk M, et al. Evaluation of cognitive functions of juvenile myoclonic epileptic patients by magnetic resonance spectroscopy and neuropsychiatric cognitive tests concurrently. Neurol Sci. 2016;37(4):623–7.
Dickson JM, Wilkinson ID, Howell SJL, Griffiths PD, Grünewald RA. Idiopathic generalised epilepsy: a pilot study of memory and neuronal dysfunction in the temporal lobes, assessed by magnetic resonance spectroscopy. J Neurol Neurosurg Psychiatry. 2006;77(7):834–40.
Roid GH, Barram RA. Essentials of Stanford-Binet Intelligence Scales (SB5) assessment. USA: Wiley; 2004.
Digit Span Test. Encyclopedia Clin Neuropsychol. 2011;849–849. https://doi.org/10.1007/978-0-387-79948-3_4407.
Schweiger A, Elkana O, Keren O. Quantitative scoring of the cube drawing test: an empirical approach. G Acta Neuropsychol. 2005;3(4):343–54.
Elwood RW. The Wechsler memory scale-revised: psychometric characteristics and clinical application. Neuropsychol Rev. 1991;2(2):179–201.
Corrigan JD, Hinkeldey NS. Relationships between parts A and B of the Trail Making Test. J Clin Psychol. 1987;43(4):402–9.
Stanczak DE, Stanczak EM, Awadalla AW. Development and initial validation of an Arabic version of the expanded trail making test: implications for cross-cultural assessment. Arch Clin Neuropsychol. 2001;16(2):141–9.
Ruff RM, Light RH, Parker SB, Levin HS. Benton controlled oral word association test: reliability and updated norms. Arch Clin Neuropsychol. 1996;11(4):329–38.
Bernasconi A, Cendes F, Theodore WH, Gill RS, Koepp MJ, Hogan RE, et al. Recommendations for the use of structural magnetic resonance imaging in the care of patients with epilepsy: a consensus report from the International League Against Epilepsy Neuroimaging Task Force. Epilepsia. 2019;60:1054–68.
Abdel Aziz K, Khater MS, Emara T, Tawfik HM, Rasheedy D, Mohammedin AS, et al. Effects of age, education, and gender on verbal fluency in healthy adult Arabic-speakers in Egypt. Appl Neuropsychol Adult. 2017;24(4):331–41.
Abedi-Firouzjah R, Rostamzadeh A, Banaei A, Shafiee M, Moghaddam ZM, Vafapour H. Exploring changes in Thalamus metabolites as diagnostic biomarkers in idiopathic generalised epilepsy patients using magnetic resonance spectroscopy. Malays J Med Sci. 2020;27(1):78.
Dixon RM, Bradley KM, Budge MM, Styles P, Smith AD. Longitudinal quantitative proton magnetic resonance spectroscopy of the hippocampus in Alzheimer’s disease. Brain. 2002;125(Pt 10):2332–41.
Bernhardt BC, Rozen DA, Worsley KJ, Evans AC, Bernasconi N, Bernasconi A. Thalamo-cortical network pathology in idiopathic generalized epilepsy: insights from MRI-based morphometric correlation analysis. Neuroimage. 2009;46(2):373–81.
Berg AT, Baca CB, Rychlik K, Vickrey BG, Caplan R, Testa FM, et al. Determinants of social outcomes in adults with childhood-onset epilepsy. Pediatrics. 2016;137(4).
Abarrategui B, Parejo-Carbonell B, García García ME, Di Capua D, García-Morales I. The cognitive phenotype of idiopathic generalized epilepsy. Epilepsy Behav. 2018;1(89):99–104.
Jackson DC, Dabbs K, Walker NM, Jones JE, Hsu DA, Stafstrom CE, et al. The neuropsychological and academic substrate of new-onset epilepsies. J Pediatr. 2013;162(5):1047.
Ratcliffe C, Wandschneider B, Baxendale S, Thompson P, Koepp MJ, Caciagli L. Cognitive function in genetic generalized epilepsies: insights from neuropsychology and neuroimaging. Front Neurol. 2020;10(11):144.
Chowdhury FA, Elwes RDC, Koutroumanidis M, Morris RG, Nashef L, Richardson MP. Impaired cognitive function in idiopathic generalized epilepsy and unaffected family members: an epilepsy endophenotype. Epilepsia. 2014;55(6):835–40.
Loughman A, Bowden SC, D’Souza WJ. A comprehensive assessment of cognitive function in the common genetic generalized epilepsy syndromes. Eur J Neurol. 2017;24(3):453–60.
Loughman A, Bowden SC, D’Souza W. Cognitive functioning in idiopathic generalised epilepsies: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2014;43:20–34.
Johnson MR, Shorvon SD. Heredity in epilepsy: neurodevelopment, comorbidity, and the neurological trait. Epilepsy Behav. 2011;22(3):421–7.
Simani L, Raminfard S, Asadollahi M, Roozbeh M, Ryan F, Rostami M. Neurochemicals of limbic system and thalamofrontal cortical network: are they different between patients with idiopathic generalized epilepsy and psychogenic nonepileptic seizure? Epilepsy Behav. 2020;112: 107480.
Doelken MT, Mennecke A, Stadlbauer A, Kecskeméti L, Kasper BS, Struffert T, et al. Multi-voxel magnetic resonance spectroscopy at 3 T in patients with idiopathic generalised epilepsy. Seizure. 2010;19(8):485–92.
Gloor P, Metrakos J, Metrakos K, Andermann E, van Gelder N. Neurophysiological, genetic and biochemical nature of the epileptic diathesis. Electroencephalogr Clin Neurophysiol Suppl. 1982;(35).
Savic I, Österman Y, Helms G. MRS shows syndrome differentiated metabolite changes in human-generalized epilepsies. Neuroimage. 2004;21(1):163–72.
Savic I, Lekvall A, Greitz D, Helms G. MR spectroscopy shows reduced frontal lobe concentrations of N-acetyl aspartate in patients with juvenile myoclonic epilepsy. Epilepsia. 2000;41(3):290–6.
Witt JA, Elger CE, Helmstaedter C. Adverse cognitive effects of antiepileptic pharmacotherapy: each additional drug matters. Eur Neuropsychopharmaco. 2015;25(11):1954–9.
Packer RMA, McGreevy PD, Pergande A, Volk HA. Negative effects of epilepsy and antiepileptic drugs on the trainability of dogs with naturally occurring idiopathic epilepsy. Appl Anim Behav Sci. 2018;1(200):106–13.
van Veenendaal TM, Ijff DM, Aldenkamp AP, Hofman PAM, Vlooswijk MCG, Rouhl RPW, et al. Metabolic and functional MR biomarkers of antiepileptic drug effectiveness: a review. Neurosci Biobehav Rev. 2015;1(59):92–9.
Ramirez-García T, Serrano-Castro PJ, Alonso-Morillejo E, Perea-Justicia P, Iglesias-Espinosa M, Parrón-Carreño T. Cognitive profile of zonisamide and valproic acid in the treatment of idiopathic generalized epilepsy: a comparative observational study. Neurol Ther. 2016;5(1):59–68.
O’Muircheartaigh J, Vollmar C, Barker GJ, Kumari V, Symms MR, Thompson P, et al. Abnormal thalamocortical structural and functional connectivity in juvenile myoclonic epilepsy. Brain. 2012;135(Pt 12):3635–44.
Pulsipher DT, Seidenberg M, Guidotti L, Tuchscherer VN, Morton J, Sheth RD, et al. Thalamofrontal circuitry and executive dysfunction in recent onset juvenile myoclonic epilepsy. Epilepsia. 2009;50(5):1210.
Acknowledgements
The department of radiology should acknowledge as they save no time and effort to bring this study to reality.
Funding
No funding resources were declared for this research.
Author information
Authors and Affiliations
Contributions
LD: responsible for drafting the work, analyzing, and interpreting the data, writing the article, and communicating with the journal during the manuscript submission, peer review, and publication process. SS: responsible for analyzing, interpreting the data of the work, and approving the final reversion of the work. MA: responsible for analyzing the data of the work. AH: responsible for data collection, sharing in writing the article. MI: responsible for radiological analysis and interpretation of the collected data. ME: responsible for analyzing, and interpreting the data of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Faculty of Medicine, Fayoum University Ethical Committee had approved the study written informed consent was obtained from all the patients and control volunteers before study initiation. The research has been approved by the ethical committee, Faculty of Medicine, Fayoum University on June 11th, 2020 with code (D-223).
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of financial interest to declare concerning this study. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Daker, L.I., Sayed, S.S., Abdelghaffar, M. et al. Could thalamic biochemical changes correlate to cognitive impairment in idiopathic generalized epilepsy?. Egypt J Neurol Psychiatry Neurosurg 59, 35 (2023). https://doi.org/10.1186/s41983-023-00638-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00638-2