Abstract
Background
Restless leg syndrome (RLS) is a common neurological morbidity. It is, however, a frequently underdiagnosed medical condition. This study was hence done to assess the occurrence and severity of RLS among participants and to study its determinants and its association with quality of sleep. This was a cross-sectional study conducted among the general population of Mangalore in July 2021. Data were collected using a Google Form. The International Restless Legs Syndrome Study Group Rating Scale was used to diagnose RLS and its severity. The Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality.
Results
The prevalence of RLS among the 202 participants was 24(11.9%). Among them, 5 were already diagnosed with RLS. Their mean age at onset was 40.4 ± 25.3 years. Among the rest 197 participants, 19(9.6%) were newly diagnosed with RLS. The severity of RLS was mild, moderate and severe among 7(36.8%), 9(47.4%) and 3(15.8%) participants, respectively. Five (26.3%) of the 19 newly diagnosed participants were identified as RLS sufferers. In multivariable analysis, the presence of diabetes mellitus and family history of RLS were associated with the presence of RLS among the participants. The mean Global PSQI value was 5.0 ± 3.1. Sleep latency was prolonged (p = 0.001), and sleep disturbances (p = 0.01) were higher among participants newly diagnosed with RLS (n = 19) compared to those without RLS (n = 178). Subjective sleep quality was poor (p = 0.038), and sleep disturbances (p = 0.016) were more among participants with severe degree RLS.
Conclusions
The prevalence of RLS in the present study was higher than that reported in previous Indian studies. Unpleasant sensations in RLS affected sleep initiation and maintenance among the affected. A multi-disciplinary approach is required to control its determinants and address other sleep-related problems among the RLS affected population.
Similar content being viewed by others
Background
Restless leg syndrome (RLS) is a common neurological morbidity. It affects as many as 4–29% of the general population in developed countries [1]. It is characterized by unpleasant sensations in the limbs relieved by movement. It is associated with sleep disturbances, anxiety, depression and deterioration in quality of life [2]. It thus has a significant social burden.
Despite these related problems, it is still a frequently underdiagnosed medical condition in India [3, 4]. Delay in diagnosis occurs probably due to minimal sensitization of this disease among medical practitioners. This may be why it is often wrongly diagnosed as an anxiety disorder or as a manifestation due to underlying exertion or fatigue [5]. There have also been reports of non-seeking of medical help by the patients due to ignorance of RLS [5]. Hence, there is a need to increase awareness about RLS among medical professionals and the general population, so that people suffering from it can be diagnosed early and managed. The understanding of its determinants is also very minimal, and therefore, a better understanding of its determinants will help to frame suitable preventive measures.
Prior studies on RLS were not comprehensively conducted. Some studied the occurrence of RLS only among people aged 40 years and above, while others studied its occurrence in patients with only specific diseases, such as diabetes mellitus and depression [6,7,8].
Hence, it was necessary to conduct this study to address these limitations. It would also help to improve the understanding of people toward RLS, its determinants, and its adverse health consequences. With this background, the present study was conducted to assess the occurrence and severity of RLS among participants and to study its determinants and its association with quality of sleep.
Methods
This cross-sectional study was done in July 2021. The institutional ethics committee gave the approval to conduct this study. The approval number was IEC KMC MLR 05-2020/200(C).
The formula Zα2PQ/d2 was used to calculate the sample size. In a study done in Pakistan [5], 23.6% of participants had RLS using the International Restless Legs Syndrome Study Group Rating Scale (IRLSSG) screening tool. The minimal sample size at 95% confidence intervals and 6% absolute precision was calculated as 193.
The questionnaire used for data collection was designed as a Google Form. It was content validated and pilot tested before its use in the present study. Considering the threat due to the ongoing COVID-19 pandemic, data were collected by sharing the questionnaire link using WhatsApp and email among the general population of Mangalore. The participants were hence recruited in this study using non-random sampling method. The first page of the questionnaire contained the study information sheet and the consent form.
Participants aged 18 years and above were included in this study. Those who did not give consent for participation, and those aged below 18 years of age were excluded from this study.
The first part of the questionnaire enquired sociodemographic details, total monthly family income, number of family members, known status of RLS, history of other comorbidities, history of using substances of abuse, self-reported height and weight and recent blood investigation reports of fasting blood sugar (FBS), glycosylated haemoglobin, serum creatinine, and blood urea nitrogen values among the participants. The second part constituted the IRLSSG screening tool. Initial four questions of this tool were meant to diagnose RLS based on the symptoms experienced in the preceding 1 week. The subsequent 10 questions were designed in a five-point Likert scale with scores ranging from 0 to 4. These were meant to assess the severity among those newly diagnosed with RLS over the preceding week. The severity was considered “none, mild, moderate, severe and very severe” if the cumulative score was 0, 1–10, 11–20, 21–30 and 31–40, respectively. The third part of the questionnaire constituted the Pittsburgh Sleep Quality Index (PSQI). This assessed the quality of sleep over the past 1 month. It had 10 questions designed in a four-point Likert scale scored from 0 to 3. These questions assessed seven components under sleep quality. The total of the seven component scores gave the Global PSQI score, which ranged from 0 to 21 (no difficulty to severe difficulty in sleeping).
The internal consistency Cronbach’s alpha of the IRLSSG screening tool used in this study was found to be 0.95, and of the PSQI was found to be 0.7.
The early onset RLS was defined as patients diagnosed with RLS before 45 years [9].
RLS sufferers were those participants who reported both frequencies of symptoms at least twice a week and experienced distress due to symptoms of RLS of the moderate or severe degree over the past 1 week [10].
In this study, current users of substances of abuse were defined as those who used tobacco (either in smoked or smokeless form) or alcohol within the recent 1 month [11].
Body mass index (BMI) was categorized based on the Asia–Pacific classification. Socioeconomic status (SES) was classified based on the Modified BG Prasad classification of 2021.
Data were analyzed using SPSS Statistics for Windows, Version 25.0; IBM Corp, Armonk, NY, USA. Statistical tests such as the Independent samples t test, Chi-Square test, Fisher’s exact test, and binary logistic regression analysis were applied. p ≤ 0.05 was set as cut off to state statistical significant association.
Results
The mean age of the participants was 29 ± 13 years. It ranged from 18 to 84 years (Table 1).
Among the participants, 2(1%) had a parental history of consanguineous marriage. Thirty-seven (18.3%) had one or other comorbidities. This comprised of type II diabetes mellitus among 17(8.4%), hypertension among 15(7.4%), asthma among 7(3.5%), anaemia among 6(3%), snoring, dyslipidaemia and hypothyroidism among 4(2%) participants each, diabetic foot among 3(1.5%), rheumatoid arthritis and hyperthyroidism among 2(1%) participants each and type I diabetes mellitus, polycystic ovarian disease, osteoarthritis, and obsessive–compulsive disorders among 1 participant each out of the 202 participants. Of the total participants, 21(10.4%) were current smokers, 15(7.4%) were ex-smokers, 5(2.5%) each were current tobacco chewers and ex-tobacco chewers, 58(28.7%) were current alcohol users, and 26(12.9%) were ex-alcohol users.
Among the 18 patients with either Type I or II diabetes mellitus, recent FBS values were on the higher side among 8, recent HbA1c values were on the higher side among 5, blood urea nitrogen values were on the higher side among 2, and serum creatinine values were on the higher side in 1 patient. The median duration of diabetes mellitus was 8.5 years (IQR 2.5, 19.75 years).
Out of the 18 diabetic patients, 11(61.1%) felt that their blood sugars were well in control, 5(27.7%) felt that it was somewhat in control, 1(5.6%) felt that it was in little control, and 1(5.6%) felt that it was not at all in control.
The prevalence of RLS out of the total 202 participants was 24(11.9%). Among them, 5 were known patients with RLS. Their mean age at onset was 40.4 ± 25.3 years. Four of them had early age at the onset of RLS.
Among the known patients with RLS, both the patients with a family history of RLS had early age at the onset of RLS. In comparison, out of 3 patients without a family history of RLS among the known patients with RLS, 2(66.7%) had early age at the onset of RLS (p = 1).
Out of 13(6.4%) participants with a family history of RLS out of the total participants, 3 reported it to be present in their father, 6 in their mother, 1 in both father and brother, 1 in grandfather, 1 in sister, and 1 in uncle (Table 2).
Out of the 24 participants, both previously diagnosed and newly diagnosed with RLS, 7(29.2%) had a family history of RLS.
Out of the 197 participants who were not diagnosed with RLS before, 19(9.6%) were found positive for RLS using the screening tool (Table 2).
The severity of RLS among the 19 participants newly diagnosed with RLS was of mild, moderate, and severe degree among 7(36.8%), 9(47.4%), and 3(15.8%), respectively, based on the ten parameters indicating the severity of RLS listed in Table 2.
Of the newly diagnosed participants, 6(31.6%) reported moderate degree of symptoms, and 7(36.8%) reported frequency of symptoms at least twice a week (Table 2).
Five (26.3%) of the 19 newly diagnosed participants fulfilled both these criteria and were identified as RLS sufferers. The prevalence of RLS sufferers was 5(2.5%) out of the 197 participants.
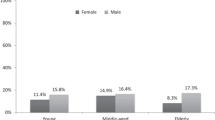
The presence of RLS (both newly/previously diagnosed) was seen significantly more among participants aged > 30 years, those married, those with comorbidities, such as diabetes mellitus and hypertension, and those with a family history of RLS in the univariate analysis (Table 3).
There was no association of RLS status with gender (p = 0.647), occupation (p = 0.987), educational status (p = 0.226), number of family members (p = 0.592), BMI (p = 0.424), SES (p = 1), residential status (p = 0.07), presence of comorbidities (p = 0.409), chewing tobacco status (p = 0.3377), smoking cigarettes status (p = 1), drinking alcohol status (p = 0.228) among the participants and the self-perceived control status of blood sugar among the diabetic patients (p = 0.1534).
In multivariable analysis, the presence of diabetes mellitus (p < 0.001) and family history of RLS (p < 0.001) were associated with the presence of RLS among the participants (Table 3).
Out of 12 female patients newly diagnosed with RLS, 3(25%) had severe degree RLS. Out of 7 male patients newly diagnosed with RLS, none had severe degree RLS (p = 0.263).
There was no association of sociodemographic variables, history of usage of substances of abuse, presence of comorbidities, duration of diabetes mellitus, and abnormalities in the recent blood investigation report with the severity of RLS among the participants.
Among the five newly diagnosed RLS participants with a family history of RLS, 2(40%) were RLS sufferers. Out of the rest 14 newly diagnosed RLS participants without a family history of RLS, 3(21.4%) were RLS sufferers (p = 0.57).
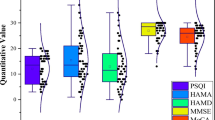
The Global PSQI score ranged from 0 to 17. Its mean value was 5.0 ± 3.1.
Sleep latency was prolonged (p = 0.001) and sleep disturbances (p = 0.01) were higher among participants newly diagnosed with RLS (n = 19) compared to those without RLS (n = 178) (Table 4).
The Global PSQI among the participants with mild degree RLS (n = 7) was 5.4 ± 2.3 and among those with moderate or severe degree RLS (n = 12) was 6.3 ± 3.2 (t = 0.653, p = 0.523).
Subjective sleep quality was poor (p = 0.038), and sleep disturbances (p = 0.016) were more among participants with severe degree RLS (Table 5).
The mean subjective sleep quality scores among RLS sufferers (n = 5) was 1.4 ± 0.55 in comparison with 0.745 ± 0.643 among non-sufferers (n = 14) [95% CI − 0.0162 to 1.53, p = 0.054].
Discussion
The prevalence of RLS in the present study was found to be 11.9% compared to 5.5% [12], 8.4% [13], 13.7% [6] and 23.6% [5] reported in studies done in other parts of the world. However, in other Indian studies, its prevalence was 2.1% [3] and 2.9% [4]. Therefore, its prevalence was much higher in the present study compared to previous studies done in India. This could be because of varying age distribution, family history of RLS and morbidity pattern among the participants of previous Indian studies compared to participants in this study. In the study done by Panda and colleagues, the age distribution of participants ranged from 16 to 55 years compared to 18 to 84 years in the present study [4]. In the other study done by Rangarajan and colleagues, the proportion of patients with diabetes mellitus and hypertension was 4.9% and 4.7%, respectively, in comparison with 8.9% and 7.4% observed in the present study [3]. In addition, family history of RLS was reported by 0% [4] and 18.5% [3] participants in these studies compared to 29.2% reported by participants in the present study.
Determinants independently associated with RLS status among the participants in the present study were family history of RLS and the presence of diabetes mellitus. This highlights the role of genetic factors and lifestyle diseases in the occurrence of RLS. Analytical studies in genetics have identified 20 single nucleotide polymorphisms in 19 loci on the chromosomes related to RLS [14].
However, there was no association between family history of RLS and early age at the onset of RLS among the previously diagnosed RLS patients in this study.
In previous studies, young age [6], increasing age [5, 12, 15, 16], male gender [13, 16], female gender [5, 15], low educational status [3, 5, 15], poor SES [3], history of consanguinity [13], history of smoking [5, 13], history of alcohol usage [3], higher BMI [15], presence of depression [6, 12], anxiety [6], stress [5, 6], gastritis [15], anaemia [15], hypertension [15], diabetes mellitus [13], bronchial asthma [13] and habitual snoring practice [13] were associated with the presence of RLS among the participants.
The proportion of RLS sufferers among the newly diagnosed RLS patients in this study was 26.3% which was more than 8.3% reported in the Korean study [12]. The proportion of RLS sufferers among the total participants in a study done in Denmark was reported to be 5.2% which was more than 2.5% as observed in the present study [17]. The RLS sufferers constitute a medically significant group who most likely require medical treatment [18].
The present study observed that as many as 26.3% participants had the frequency of symptoms 4 or more times per week which was lesser than that reported among 50.1% patients in a study done in Pakistan [5].
The proportion of newly diagnosed RLS participants with moderate to severe degree RLS in the present study was 63.2% in comparison with 25% [12], 67.4% [5], 68.3% [15] reported in studies done at Korea, Pakistan and China, respectively.
No sociodemographic variables were associated with the severity of RLS in the present study. On the contrary, the study done in Bangalore, India, reported that RLS severity was significantly higher among males [3].
The present study observed that prolonged sleep latency and sleep disturbances were more among participants newly diagnosed with RLS. This was supported by the observation of Rangarajan and colleagues, where sleep latency was prolonged among participants with RLS [3]. RLS is, therefore, related to difficulty in initiating and maintaining sleep and disrupting sleep. In addition, a study done in Saudi Arabia reported the presence of RLS to be associated with daytime sleepiness and habitual snoring [13]. On the contrary, a Korean study reported no association between the presence of RLS and sleep profiles among the participants [12].
In the present study, subjective sleep quality was affected and sleep disturbances were more among newly diagnosed participants with severe degree RLS. In the study done in Bangalore, India severity of RLS was found to positively and significantly correlate with delay in sleep onset [3].
RLS is a major determinant of insomnia among the affected population, which drives them to seek medical care [1]. Sleep disturbances are a known determinant of stroke and other cardiovascular disorders [19]. These observations infer that improper sleep habits among the RLS patients could also affect their health and well-being, work productivity, and social activities.
The majority of previously diagnosed patients in the present study were on Ayurvedic treatment for RLS. Medications are commonly advised among primary RLS patients when symptoms are of moderate or severe degree [18].
Conclusions
The prevalence of RLS in the present study was higher than that reported in previous Indian studies. Determinants such as family history of RLS and the presence of diabetes mellitus were independently associated with its presence, indicating the role of genetic factors and lifestyle diseases in its occurrence. Unpleasant sensations in RLS significantly affected sleep initiation and maintenance among the affected. A multi-disciplinary approach is required to control its determinants and address other sleep-related problems among the RLS affected population at this setting.
Limitations
The cross‑sectional design might be a deterrent to establishing a causal relationship. There is also a possibility of non-reporting of symptoms by the participants. There were few participants with diabetes mellitus, hypothyroidism, and rheumatoid arthritis in study. There is a possibility that some of these patients might be also suffering from peripheral neuropathy, which is a major differential diagnosis of RLS. The non-random selection of 202 participants considering the prevailing COVID-19 conditions could also be another limitation of this study.
Availability of data and materials
The research data are deposited in the Figshare repository: ‘Study on restless leg syndrome and its relationship with quality of sleep among the general population of India’. https://doi.org/10.6084/m9.figshare.19550776
Abbreviations
- RLS:
-
Restless leg syndrome
- IRLSSG:
-
International Restless Legs Syndrome Study Group Rating Scale
- PSQI:
-
Pittsburgh Sleep Quality Index
- COVID-19:
-
Coronavirus disease 2019
- FBS:
-
Fasting blood sugar
- BMI:
-
Body mass index
- SES:
-
Socioeconomic status
- SPSS:
-
Statistical Package for Social Sciences
- UOR:
-
Unadjusted odds ratio
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence intervals
- SD:
-
Standard deviation
References
Innes KE, Selfe TK, Agarwal P. Prevalence of restless legs syndrome in North American and Western European populations: a systematic review. Sleep Med. 2011;12:623–34.
Mansur A, Castillo PR, Cabrero RF, Bokhari SRA. Restless legs syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK430878/. Updated 2022 Mar 11.
Rangarajan S, Rangarajan S, D’Souza GA. Restless legs syndrome in an Indian urban population. Sleep Med. 2007;9:88–93.
Panda S, Taly AB, Sinha S, Gururaj G, Girish N, Nagaraja D. Sleep-related disorders among a healthy population in South India. Neurol India. 2012;60:68–74.
Mahmood K, Farhan R, Surani A, Surani AA, Surani S. Restless legs syndrome among Pakistani population: a cross-sectional study. Int Sch Res Notices. 2015;2015: 762045.
Castillo PR, Mera RM, Fredrickson PA, Zambrano M, Del Brutto VJ, Del Brutto OH. Psychological distress in patients with restless legs syndrome (Willis-Ekbom disease): a population-based door-to-door survey in rural Ecuador. BMC Res Notes. 2014;7:911.
Afkhami-Ardekani A, Momayez-Sanat Z, Vahhabi Z, Vazirpanah T, Afkhami-Ardekani M. The relationship between frequency of restless leg syndrome and type 2 diabetes. Iran J Diabetes Obes. 2017;9:40–4.
Gupta R, Lahan V, Goel D. Prevalence of restless leg syndrome in subjects with depressive disorder. Indian J Psychiatry. 2013;55:70–3.
Guo S, Huang J, Jiang H, Han C, Li J, Xu X, et al. Restless legs syndrome: from pathophysiology to clinical diagnosis and management. Front Aging Neurosci. 2017;9:171.
Salas RE, Kwan AB. The real burden of restless legs syndrome: clinical and economic outcomes. Am J Manag Care. 2012;18:S207–12.
Chen J, Li S, Zheng K, Wang H, Xie Y, Xu P, et al. Impact of smoking status on stroke recurrence. J Am Heart Assoc. 2019;8:e011696.
Kim TJ, Yoon JE, Park JA, Lee SK, Chu MK, Yang KI, et al. Prevalence and characteristics of restless legs syndrome in Korean adults: a study in two independent samples of the general population. Neuroepidemiology. 2019;52:193–204.
Wali SO, Abaalkhail B. Prevalence of restless legs syndrome and associated risk factors among middle-aged Saudi population. Ann Thorac Med. 2015;10:193–8.
Schormair B, Zhao C, Bell S, Tilch E, Salminen AV, Putz B, et al. Identification of novel risk loci for restless legs syndrome in genome-wide association studies in individuals of European ancestry: a meta-analysis. Lancet Neurol. 2017;16:898–907.
Shi Y, Yu H, Ding D, Yu P, Wu D, Hong Z. Prevalence and risk factors of restless legs syndrome among Chinese adults in a rural community of Shanghai in China. PLoS ONE. 2015;10:e0121215.
Harisudan S, Soumya PC, Prasanna KB, Kumar SK. Restless leg syndrome in general population of an urban area in India. J Med Sci Clin Res. 2018;6:725–35.
Didriksen M, Hansen TF, Thorner LW, Burgdorf KS, Erikstrup C, Pedersen OB, et al. Restless legs syndrome is associated with increased risk of migraine. Cephalalgia Rep. 2018;1:1–7.
Winkelman JW, Armstrong MJ, Allen RP, Chaudhuri KR, Ondo W, Trenkwalder C, et al. Practice guideline summary: treatment of restless legs syndrome in adults: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology. 2016;87:2585–93.
Koo DL, Nam H, Thomas RJ, Yun CH. Sleep disturbances as a risk factor for stroke. J Stroke. 2018;20:12–32.
Acknowledgements
The authors of this study thank Dr. Arun Shirali, Associate Professor, Department of Internal Medicine, Kasturba Medical College, Mangalore, India for his help in content validation of the data collection tools. We also thank all the participants who enthusiastically took part in this study.
Funding
No source of funding was acquired for this research study.
Author information
Authors and Affiliations
Contributions
NJ: guarantor of this research work, concept, design, literature search, proforma preparation, data collection, data analysis, manuscript preparation, revising the work critically for important intellectual content. SS, SP and AB: Literature search, data collection, interpretation of data, revising the work critically for important intellectual content, manuscript editing. SMM, VG: data collection, interpretation of data, revising the work critically for important intellectual content, manuscript editing. The requirements for authorship as stated earlier in this document have been met, and each author believes that the manuscript represents honest work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
It was obtained from the institutional ethics committee with reference number IEC KMC MLR 05-2020/200(C) dated 27th May 2020 and was in accordance to the 1964 Helsinki declaration. Informed consent to participate was taken from the participants using a Google form.
Consent for publication
The participants were informed that the data generated as a part of this study would be used for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Joseph, N., Suresh, S., Prasad, S. et al. Study on restless leg syndrome and its relationship with quality of sleep among the general population of Mangalore, India. Egypt J Neurol Psychiatry Neurosurg 58, 109 (2022). https://doi.org/10.1186/s41983-022-00544-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-022-00544-z