Abstract
Background
Host inflammation has been studied in patients with ischemic stroke (IS) due to large vessel occlusions. Inflammatory markers were shown to correlate with large artery atherosclerosis and worse outcomes after ischemic stroke due to large vessel occlusions. However, the association between inflammation and cerebral small vessel disease (SVD) is controversial. Mostly studied are the white matter hyperintensities; however, results regarding association of white matter hyperintensities with inflammatory markers are conflicting. We aimed to investigate the association between cerebral microbleed (CMB) load, as an indicator of SVD, and inflammation indices in patients with IS.
Results
We identified 127 patients with IS admitted within 7 days of symptom onset. CMBs were detected in 37% (n: 47) of patients. Patient’s age and Fazekas score were independently associated with CMB load. Inflammatory biomarkers were not associated with the presence or quantitative burden of CMBs.
Conclusions
White matter damage and patient’s age predicted CMB presence and number, respectively, in IS patients. However, inflammatory markers failed to show any association with such SVD signs. Prospective studies with a higher number of stroke patients are needed in order to justify our findings.
Similar content being viewed by others
Introduction
Brain parenchymal changes on conventional magnetic resonance imaging (MRI), such as white matter hyperintensities (WMHs), recent small subcortical infarcts, lacunes, prominent perivascular spaces, cerebral microbleeds (CMBs) and atrophy, reveal cerebral small vessel disease (SVD) [1]. CMBs are small (< 10 mm) rounded areas of signal loss on paramagnetic-sensitive MR sequences, such as T2*-weighted gradient-recalled echo (GRE) or susceptibility-weighted imaging (SWI) sequences. These areas of signal void with associated blooming are most commonly located in the cortico-subcortical junction, and deep grey or white matter in the cerebral hemispheres, brainstem, and cerebellum [2].
The main histopathological changes underlying CMBs are hypertensive vasculopathy and cerebral amyloid angiopathy (CAA), which are the most prevalent forms of SVDs [3,4,5,6]. CAA is a cerebral SVD characterised by accumulation of amyloid-beta protein within the leptomeningeal and cortical blood vessels [1]. While hypertensive vasculopathy affects deep cerebral and infratentorial brain regions, CAA leads to strictly lobar CMBs. CMB burden is accepted as a sign of underlying SVD, and is associated with both haemorrhagic and ischemic stroke [7, 8]. The presence and burden of CMBs were found to be predictors of increased risk of haemorrhagic transformation and poor functional outcome in patients with ischemic stroke [9,10,11,12,13,14].
Inflammation was found to play a role in atherosclerosis. Higher levels of inflammatory markers were associated with poor outcomes in patients with stroke due to large vessel occlusions. Neutrophil–lymphocyte ratio (NLR), platelet–lymphocyte ratio (PLR), mean platelet volume (MPV), MPV–platelet ratio and C-reactive protein (CRP) can be easily obtained and have been extensively investigated as simple biomarkers of systemic inflammation [15,16,17,18,19,20]. The association between these markers and SVD is controversial. However, still there are studies supporting a positive association. In first ever acute lacunar stroke patients, both serum matrix metalloproteinase and CRP were significantly elevated in patients with CMBs compared to patients without CMB [21]. In a cross sectional study among community-based stroke free participants, higher levels of circulating tumor necrosis factor receptor 2 and myeloperoxidase were detected in the presence of CMB [22]. Whether hypertensive or CAA, the underlying pathology of CMB seems to result from reciprocal interactions between endothelial dysfunction and inflammatory cascade activation [23]. Therefore, an association between CMB and markers of inflammation can be expected.
Here, we aimed to investigate whether there is an association between CMB load, as a sign of SVD, with inflammatory markers in ischemic stroke (IS) patients.
Methods
All consecutive patients with acute ischemic stroke who were admitted to the emergency and neurology departments of our university hospital between January 2016 and July 2020 were retrospectively reviewed from patient files and the centre’s database. Patient demographics, previous anticoagulant and antiaggregant regimens, history of diabetes mellitus, hypertension, atrial fibrillation, hyperlipidaemia, symptom duration at admission were recorded. Patients admitted within 7 days of symptom onset, with blood samples taken and MRIs performed on admission before any medical or mechanical intervention for stroke treatment were reviewed. We only included patients whose records contained adequate demographic, radiological, and laboratory data. Brain MRIs of the patients were evaluated for the presence and extend of CMBs, which are small (< 10 mm) foci of chronic blood products in brain tissue. Patients with contraindications to MRI, such as intracardiac defibrillator, cardiac pacemaker or metallic heart valve, patients with brain MRIs lacking SWI sequence, transient ischemic attacks with no diffusion restriction on MRI, severe renal or hepatic insufficiency, recent or ongoing immunosuppressive therapy, or admission after 7 days of symptom onset were excluded. No patient had a recent history of an acute infection or an inflammatory disease or received a diagnosis of a secondary inflammatory disease, such as vasculitis at the end of the stroke evaluation.
We reviewed the MRI findings from the picture archiving and communication system (PACS) of the radiology department. The radiologist, who was blinded to clinical information, retrospectively evaluated images of T2 series, fluid attenuated recovery (FLAIR), DWI, apparent diffusion coefficient map and SWI sequences obtained in the 1.5 T MR-system (Magnetom Aera 1.5 T, Siemens Healthcare). CMB was defined as ovoid or rounded signal void spots less than 1 cm on T2* GRE or SWI sequences. Signal voids caused by sulcal vascular structures, old haemorrhagic CVE sequelae, basal ganglion or pineal gland calcifications were excluded. CMB locations were classified into deep, lobar, infratentorial categories and mixed categories. Lobar location corresponded to cortical and subcortical regions (including subcortical U fibers). Deep location included the basal ganglia, thalamus, internal capsule, external capsule, corpus callosum, and deep and periventricular white matter. The infratentorial location included the brainstem and cerebellum (Fig. 1).
MRI image obtained from one of our patients. A large number of susceptibility artifacts consistent with cerebral microbleeds are observed in the form of black dots on axial maximum intensity projection SWI images. This patient was included in the group of those with more than 20 microbleeds and scattered localization patterns
Evaluation of WMH was made on FLAIR images included in the MRI protocol. Fazekas scale was used to determine the gliosis severity by grading WMHs on MRI [24]. The severity of the WMH was graded with the following scale: 0 = absent; 1 = punctuate foci; 2 = beginning of confluence of foci; and 3 = large confluent areas.
Hypertension was considered present if the patient exhibited a systolic blood pressure ≥ 140 mmHg or a diastolic blood pressure ≥ 90 mmHg prestroke, or had a history of diagnosis of hypertension and anti-hypertensive medications. Diabetes mellitus (DM) was considered present when a person used oral antidiabetic drugs or insulin, or when the fasting blood glucose was ≥ 126 mg/dl. Hyperlipidaemia was considered present when the person used lipid-lowering drugs or had a total cholesterol level ≥ 220 mg/dl or LDL cholesterol ≥ 130 mg/dl. Atrial fibrillation (AF) was considered present if the patient had a diagnosis of AF, or their admission electrocardiogram revealed AF or the Holter rhythm recording revealed AF or paroxysmal AF.
Baseline complete blood count, serum CRP, renal and liver function tests were recorded. NLR and PLR were defined as whole neutrophils and total number of platelets divided by whole lymphocyte count. The MPV/PLT ratio was calculated by dividing the mean platelet volume by the platelet count. Fasting blood glucose and total cholesterol levels were recorded from the tests performed after 12 h of fasting. Admission electrocardiography and 24–48 h Holter rhythm reports were recorded.
Statistical analyses were conducted in IBM SPSS Statistics 20 programme by removing the extreme values in the data set. First, we categorized CMB burden as CBM (−) and CMB (+). We also grouped CMB (+) patients as low (CMB < 5) and high (CMB ≥ 5) burden in line with studies in the literature [25,26,27]. Afterward, we categorized CMB as follows: CMB = 0, low burden-CMB = 1–4 and high burden -CMB ≥ 5. Then, all the steps in the analysis were repeated among the three CMB groups.
Clinical characteristics of the participants (sex, stroke age, hypertension, diabetes mellitus, hyperlipidemia, clinical stroke history, laboratory findings, and MRI results) according to CMB levels (CBM (−) and CMB (+)) were provided. While the categorical variables were reported as frequency and percentage, the continuous variables were reported as mean ± standard deviation. Furthermore, these clinical characteristics were compared among the CMB levels using the independent sample t-test for continuous variables and the χ2 test for categorical variables. When the parametric test assumptions were not satisfied for the continuous variables, the Mann–Whitney U test was used instead of the independent sample t-test. p-values < 0.05 were considered as statistically significant. Logistic regression analyses were performed to determine the factors associated with CMB. The models were not affected by the multicollinearity problem. The results of the logistic regression analysis were reported in terms of Odds Ratio (OR) and 95% Confidence Intervals (CI) for the parameters of the model.
After performing these analyses for the two CMB groups (CMB (−) and CMB (+)), we repeated these steps for the three CMB levels (no CMB–CMB = 0, low burden-CMB = 1–4 and high burden -CMB ≥ 5). In the multinomial regression model created according to the number of CMBs, Fazekas grade was not included in the model due to the lack of observations.
Results
The characteristics of the study patients are shown in Table 1. Our study enrolled 127 patients with IS. The mean age was 66.5 (range 18–99) years and 42% (n = 53) were female. Ninety-four percent (n = 119) of patients admitted within the first 72 h after stroke onset and 82% (n = 104) admitted within the first 24 h after stroke onset. Cerebral microbleeds were detected in 37% (n = 47) of the patients. Of those with microbleeds (n = 47), 17 (36%) had CMBs in a strictly lobar location. Strictly deep or infratentorial locations were seen in a lower proportion (17.0% and 6.4%, respectively). In 19 patients (40.4%), CMBs had mixed location.
Patient age and leukoaraiosis severity were the only predictors of having CMB in the univariate analysis (p < 0.05).
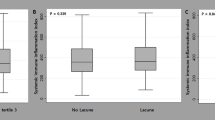
The proportion of patients with Fazekas scores reflecting moderate to severe WMH (Fazekas grades 2–3) was higher in patients with CMB compared to patients without (p < 0.001) (Fig. 2).
There was no statistically significant difference between the two groups in terms of CRP, NLR, PLR, MPV and MPV/platelet ratio (p > 0.05, for each). Of note, none of the inflammatory markers showed an association with WMH severity indicated as Fazekas grades.
In the logistic regression analysis, only the Fazekas grade was significantly associated with CMB presence. There was a graded association between having CMB and the Fazekas score. While the odds of having micro bleeding was 3.86 times greater for Fazekas grade 1 as opposed to Fazekas grade 0, the odds of having micro-bleeding was 6.41 and 14.71 times greater for Fazekas grades 2 and 3, respectively, as opposed to Fazekas grade 0 (p values 0.105, 0.024 and 0.003, 95% confidence intervals 0.694–21.518, 1.153–35.717, and 2.490–86.930 respectively). Stroke age lost its statistical significance for CMB presence after logistic regression analysis (p > 0.05).
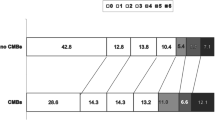
In terms of the quantitative burden of CMBs, we classified all patients into three groups according to CMB number as CMB = 0 (n = 80), low burden-CMB = 1–4 (n = 27) and high burden-CMB ≥ 5 (N = 20) (Table 2). The 5 CMBs threshold was chosen based on the methodology of two recent trials [26, 27].
Patients with a high burden of CMB were significantly older than patients both with CMB = 1–4 and without CMBs (74.08 ± 4.941 vs 63.88 ± 15.521 vs 63.64 ± 15.62, respectively, p < 0.05). The proportion of patients with Fazekas grades reflecting moderate-to-severe WMH increased stepwise as the number of CMBs increased (p < 0.001).
Forty percent of patients had a previous history of AF or newly diagnosed AF. Patients with a high CMB burden had significantly higher prevalence of AF compared to patients with a low burden or no CMBs (65% vs 37% vs 29%, respectively, p = 0.035).
There was no statistically significant difference between the three groups in terms of CRP, NLR, PLR, MPV and MPV/platelet ratio (p > 0.05 for each).
In the logistic regression analysis for burden of CMBs (Table 3), we included AF, stroke age and previous stroke/TIA variables. Here, Fazekas score was not included into the model since observations were not enough and none of the patients with CMB ≥ 5 had Fazekas grade 0 or 1. According to our findings, it is more likely that stroke age of the patients without CMB (CMB = 0) is significantly younger than the patients with CMB ≥ 5.
In Fig. 3, the confidence interval error bar chart for stroke age is provided. The results in Fig. 3 are compatible with the post-hoc tests.
Discussion
In our study, cerebral microbleeds were found to be present in 37% of patients with ischemic stroke and this is compatible with the literature. In a review on the prevalence and associations of CMBs, the CMB rate was 5.7% (range 4.5 to 7.7%) in cohorts without cerebrovascular disease and 40% (range 0 to 78%) in patients with ischemic cerebrovascular disease [7].
Patient age was the only clinical predictor of CMB burden in our cohort. The Rotterdam Scan Study investigated the prevalence of and risk factors for microbleeds in the general population aged 60 years and older. The prevalence of microbleeds increased significantly with age and did not differ between men and women [28]. Age was independently associated with the prevalence of CMBs in patients with and without ischemic stroke [7]. As mentioned before, hypertensive vasculopathy and CAA are the main underlying pathologies of the CMBs. Increased incidence of both factors with aging clearly explains the independent effect of age on CMBs [3,4,5,6].
Despite the impact of aging, we included stroke patients aged 18 years and older. CMBs and WMHs are generally seen in elderly and knowledge about their incidence in young population is lacking. However, CMBs were detected in young ischemic stroke patients. In cross sectional analysis of young ischemic stroke patients aged below 50 years (ranged from 19 to 49 years of old), CMBs were detected in 11% of cases without drug or cocaine induced vasospasm, infectious meningoencephalitis, vasculitis, sickle cell anemia, mitochondrial disorder, congenital or acquired coagulopathy. CMBs were strongly associated with systemic hypertension [29]. In our study only 4 patients were aged under 40 years of age. These patients lacked any detectable underlying disease. CMB was detected only in one, which was a single infratentorial CMB. All of these 4 patients were scored as Fazekas grade 0 in terms of WMH.
In our study population, hypertension did not show a statistically significant association with CMB existence and burden. In a review, hypertension was not consistently found to be associated with CMB and the authors attributed this in part to probable positive confounding by age [7]. In a systematic review in patients with cerebrovascular disease, hypertension was associated with CMBs (although the association was a little weaker than in the healthy cohorts) [30]. In the Rotterdam Scan Study, high systolic blood pressure was associated with the presence of microbleeds in a deep or infratentorial brain location [28], but not with lobar CMBs. It is known that hypertension is mostly associated with CMBs located in the basal ganglia, pons and cerebellum, while strictly lobar CMBs are related to CAA [31, 32]. The reason for the lack of an association with hypertension in our cohort could be the lower proportion of patients with strictly deep (17%) or infratentorial (6%) CMBs compared to strictly lobar.
We found no association between CMB presence or burden and a history of previous transient ischemic attack (TIA) or ischemic stroke. However CMBs were more prevalent among people with recurrent strokes than those with first-ever strokes in a systematic review (23% vs 44%, respectively) [30]. The relatively small size of our sample of only 26 patients (20.4%) with a history of TIA or ischemic stroke may explain the lack of an association.
Atrial fibrillation was present in 40% of patients in our cohort. The prevalence of AF did not differ significantly according to the existence of CMB, but tended to be higher in patients with high burden CMBs compared to patients with low burden CMBs in univariate analysis. In a systematic review [30], CMBs were observed less frequently in cardioembolic strokes compared to lacunar strokes (53.5% vs 19.4%, respectively). However, in a retrospective study involving ischemic stroke and TIA patients, the prevalence of CMBs in patients with AF was higher compared with patients without AF [33]. In cardioembolic ischemic strokes, similar findings were observed [34]. Prior use of antithrombotics was associated with the presence of lobar CMBs in both studies. Although AF was associated with high burden CMBs in our study, in the multivariate regression analysis, it lost its significance for predicting the overall CMB burden. Antiplatelet use (monotherapy or dual antiplatelet), oral anticoagulant use, and antiplatelet plus anticoagulant use were not associated with CMB presence or burden. While in the Rotterdam study, aspirin was related to lobar and clopidogrel was related to deep or infratentorial CMBs [35, 36], in the Framingham study antiplatelet use was associated with non-lobar CMBs [37]. A recent population based study of aging did not found any association between antiplatelet use and CMBs [38]. On the other hand, the same study found anticoagulant use to be associated with lobar CMB presence and frequency [38]. In a recent review, the association between anticoagulant therapy and CMB was restricted to strictly lobar CMBs and warfarin users rather than novel oral anticoagulants [39]. In our study, 15 (11.8%) patients had prior anticoagulant use, only 4 of which were using warfarin and 39 patients (30.7%) had antiplatelet use (2 patients were on both antiplatelet and anticoagulant therapy). The sample size and limited number of patients on warfarin may affect the dissimilarities between our study’s findings and the literature, especially in terms of anticoagulant effect.
In our study, the Fazekas scores showed a significant association with both CMB presence and number. These findings are consistent with the literature, where CMB prevalence increases with MRI correlates of cerebral microangiopathy as defined by leukoaraiosis, confluent white matter lesions, or lacunes in healthy subjects, in patients with ischemic stroke or intracranial haemorrhage [7, 28, 40].
In our study, we did not find any association between CRP, NLR, PLR or MPV levels and white matter lesions or CMBs. Studies have revealed controversial outcomes regarding the association between inflammation biomarkers and MRI findings. In the study of Chung et al. [18], although NLR was correlated with large artery atherosclerosis, no association was found between NLR and silent lacunar infarctions or WMHs, similar to the findings of the study by Costa et al. [41]. High levels of NLR were associated with larger volumes of WMH, but were not closely associated with silent brain infarcts and CMB [42]. Higher plasma CRP levels were significantly associated with the presence of cerebral white matter lesions [28, 31], CMBs [43] and lacunar infarcts [32]. Despite the large number of publications on inflammation and cerebral SVD in recent years, our current knowledge is too fragmentary to justify a clear association. Timing of the cell counts, which is performed during acute phase of stroke, could affect our results. Most of the studies that have investigated the association of inflammation markers with MRI correlates of SVD were conducted with healthy volunteers without cerebrovascular disorders. It is known that acute stroke can alter inflammatory cell populations in the blood as it induces a complex interaction between the brain and the immune system. Stroke-induced brain inflammation, and responses of the peripheral innate and adaptive immune systems to stroke (inflammation, immunodepression, autoreactivity, or protective immunity), play roles in this inflammatory cascades [44, 45]. In our study, NLR values were interpretated from blood samples taken on admission within the first 7 days of ischemic stroke. Therefore, inflammation markers on admission could be affected by immune alterations at acute onset of stroke and may not directly reflect their association with CMBs, which are chronic in nature.
Our study’s strength is due to the availability of blood test results and MRI scans involving SWI before any therapeutic intervention in IS patients. Imaging modalities used for detecting SVD were uniform in all patients. The relatively optimal number of patients with high CMB burden gave us the opportunity to compare with patients with low burden. However it was a retrospective study in a single centre with a relatively small sample size. Other limitations can be the absence of analysing cerebral SVD forms other than CMBs and WMHs such as subclinical lacunar infarcts or dilated perivascular spaces. Also, we evaluated the association of CMBs with inflammatory markers irrespective of the ischemic stroke classification such as lacunar or territorial. In a further study with a larger sample size, association of inflammatory markers and different SVD forms can be investigated in-between subtypes of ischemic stroke.
Conclusions
Our findings suggest that the major factors associated with CMB presence and number in ischemic stroke patients are leukoaraiosis and advanced age, respectively. In the acute stroke onset, inflammatory markers were not associated with CMB presence or number. Future studies with larger prospective cohort of acute IS patients, additively investigating other types of SVD are needed in this field.
Availability of data and materials
The data sets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AF:
-
Atrial fibrillation
- CMB:
-
Cerebral microbleed
- CRP:
-
C-reactive protein
- DM:
-
Diabetes mellitus
- FLAIR:
-
Fluid attenuated recovery
- GRE:
-
Gradient-recalled echo
- IS:
-
Ischemic stroke
- MPV:
-
Mean platelet volume
- MRI:
-
Magnetic resonance imaging
- NLR:
-
Neutrophil–lymphocyte ratio
- PLR:
-
Platelet-lymphocyte ratio
- SVD:
-
Small vessel disease
- SWI:
-
Susceptibility-weighted imaging
- TIA:
-
Transient ischemic attack
- WMH:
-
White matter hyperintensity
References
Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9(7):689–701.
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12(8):822–38.
Greenberg SM, Vernooij MW, Cordonnier C, Viswanathan A, Salman RA-S, Warach S, et al. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol. 2009;8(2):165–74.
Fazekas F, Kleinert R, Roob G, Kleinert G, Kapeller P, Schmidt R, et al. Histopathologic analysis of foci of signal loss on gradient-echo T2*-weighted MR images in patients with spontaneous intracerebral hemorrhage: evidence of microangiopathy-related microbleeds. Am J Neuroradiol. 1999;20(4):637–42.
Tanaka A, Ueno Y, Nakayama Y, Takano K, Takebayashi S. Small chronic hemorrhages and ischemic lesions in association with spontaneous intracerebral hematomas. Stroke. 1999;30(8):1637–42.
Knudsen KA, Rosand J, Karluk D, Greenberg SM. Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria. Neurology. 2001;56(4):537–9.
Koennecke H-C. Cerebral microbleeds on MRI: prevalence, associations, and potential clinical implications. Neurology. 2006;66(2):165–71.
Casolla B, Cordonnier C. Intracerebral haemorrhage, microbleeds and antithrombotic drugs. Revue Neurologique. 2020.
Chacon-Portillo MA, Llinas RH, Marsh EB. Cerebral microbleeds shouldn’t dictate treatment of acute stroke: a retrospective cohort study evaluating risk of intracerebral hemorrhage. BMC Neurol. 2018;18(1):1–7.
Liu C, Dong Z, Xu L, Khursheed A, Dong L, Liu Z, et al. MR image features predicting hemorrhagic transformation in acute cerebral infarction: a multimodal study. Neuroradiology. 2015;57(11):1145–52.
Zand R, Shahjouei S, Tsivgoulis G, Singh M, McCormack M, Noorbakhsh-Sabet N, et al. Cerebral microbleeds are associated with higher mortality among ischemic stroke patients. J Stroke Cerebrovasc Dis. 2018;27(11):3036–42.
Charidimou A, Shoamanesh A, Initiative IMM. Clinical relevance of microbleeds in acute stroke thrombolysis: comprehensive meta-analysis. Neurology. 2016;87(15):1534–41.
Yan J, Qiu J, Wu X, Ge Y, Wang J, Wang Y. Pretreatment cerebral microbleeds and symptomatic intracerebral hemorrhage post-thrombolysis: a systematic review and meta-analysis. J Neurol. 2020;267(2):301–7.
Dong G, Huang A, Liu L. Platelet-to-lymphocyte ratio and prognosis in STEMI: a meta-analysis. Eur J Clin Invest. 2021;51(3): e13386.
Goyal N, Tsivgoulis G, Chang JJ, Malhotra K, Pandhi A, Ishfaq MF, et al. Admission neutrophil-to-lymphocyte ratio as a prognostic biomarker of outcomes in large vessel occlusion strokes. Stroke. 2018;49(8):1985–7.
Song Q, Li Y, Wang Y, Wei C, Liu J, Liu M. Increased neutrophil-to-lymphocyte ratios are associated with greater risk of hemorrhagic transformation in patients with acute ischemic stroke. Curr Neurovasc Res. 2018;15(4):326–35.
Maestrini I, Strbian D, Gautier S, Haapaniemi E, Moulin S, Sairanen T, et al. Higher neutrophil counts before thrombolysis for cerebral ischemia predict worse outcomes. Neurology. 2015;85(16):1408–16.
Chung D, Lee KO, Choi J-W, Kim NK, Kim O-J, Kim S-H, et al. Blood neutrophil/lymphocyte ratio is associated with cerebral large-artery atherosclerosis but not with cerebral small-vessel disease. Front Neurol. 2020. https://doi.org/10.3389/fneur.2020.01022.
Guo Z, Yu S, Xiao L, Chen X, Ye R, Zheng P, et al. Dynamic change of neutrophil to lymphocyte ratio and hemorrhagic transformation after thrombolysis in stroke. J Neuroinflamm. 2016;13(1):1–8.
Ross R. Atherosclerosis–an inflammatory disease. N Engl J Med. 1999;340(2):115–26.
Koh SH, Park CY, Kim MK, Lee KY, Kim J, Chang DI, et al. Microbleeds and free active MMP-9 are independent risk factors for neurological deterioration in acute lacunar stroke. Eur J Neurol. 2011;18(1):158–64.
Shoamanesh A, Preis SR, Beiser AS, Vasan RS, Benjamin EJ, Kase CS, et al. Inflammatory biomarkers, cerebral microbleeds, and small vessel disease: Framingham Heart Study. Neurology. 2015;84(8):825–32.
Wang HL, Zhang CL, Qiu YM, Chen AQ, Li YN, Hu B. Dysfunction of the blood–brain barrier in cerebral microbleeds: from bedside to bench. Aging Dis. 2021;12(8):1898–919.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 15 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149(2):351–6.
Wilson D, Ambler G, Lee KJ, Lim JS, Shiozawa M, Koga M, et al. Cerebral microbleeds and stroke risk after ischaemic stroke or transient ischaemic attack: a pooled analysis of individual patient data from cohort studies. Lancet Neurol. 2019;18(7):653–65.
Lau KK, Lovelock CE, Li L, Simoni M, Gutnikov S, Kuker W, et al. Antiplatelet treatment after transient ischemic attack and ischemic stroke in patients with cerebral microbleeds in 2 large cohorts and an updated systematic review. Stroke. 2018;49(6):1434–42.
Dannenberg S, Scheitz JF, Rozanski M, Erdur H, Brunecker P, Werring DJ, et al. Number of cerebral microbleeds and risk of intracerebral hemorrhage after intravenous thrombolysis. Stroke. 2014;45(10):2900–5.
Vernooij M, van der Lugt A, Ikram MA, Wielopolski P, Niessen W, Hofman A, et al. Prevalence and risk factors of cerebral microbleeds: the Rotterdam Scan Study. Neurology. 2008;70(14):1208–14.
Shoamanesh A, Catanese L, Romero JR, Lau H, Babikian VL, Benavente OR, et al. High prevalence of cerebral microbleeds in inner city young stroke patients. J Stroke Cerebrovasc Dis. 2016;25(4):733–8.
Cordonnier C, Al-Shahi Salman R, Wardlaw J. Spontaneous brain microbleeds: systematic review, subgroup analyses and standards for study design and reporting. Brain. 2007;130(8):1988–2003.
Fornage M, Chiang YA, O’Meara ES, Psaty BM, Reiner AP, Siscovick DS, et al. Biomarkers of inflammation and MRI-defined small vessel disease of the brain: the Cardiovascular Health Study. Stroke. 2008;39(7):1952–9.
Mitaki S, Nagai A, Oguro H, Yamaguchi S. C-reactive protein levels are associated with cerebral small vessel-related lesions. Acta Neurol Scand. 2016;133(1):68–74.
Horstmann S, Mohlenbruch M, Wegele C, Rizos T, Laible M, Rauch G, et al. Prevalence of atrial fibrillation and association of previous antithrombotic treatment in patients with cerebral microbleeds. Eur J Neurol. 2015;22(10):1355–62.
Kim BJ, Yoon Y, Sohn H, Kang DW, Kim JS, Kwon SU. Difference in the location and risk factors of cerebral microbleeds according to ischemic stroke subtypes. J Stroke. 2016;18(3):297–303.
Vernooij MW, Haag MD, van der Lugt A, Hofman A, Krestin GP, Stricker BH, et al. Use of antithrombotic drugs and the presence of cerebral microbleeds: the Rotterdam Scan Study. Arch Neurol. 2009;66(6):714–20.
Darweesh SK, Leening MJ, Akoudad S, Loth DW, Hofman A, Ikram MA, et al. Clopidogrel use is associated with an increased prevalence of cerebral microbleeds in a stroke-free population: the Rotterdam study. J Am Heart Assoc. 2013;2(5): e000359.
Romero JR, Preis SR, Beiser A, DeCarli C, Viswanathan A, Martinez-Ramirez S, et al. Risk factors, stroke prevention treatments, and prevalence of cerebral microbleeds in the Framingham Heart Study. Stroke. 2014;45(5):1492–4.
Graff-Radford J, Lesnick T, Rabinstein AA, Gunter JL, Przybelski SA, Noseworthy PA, et al. Cerebral microbleeds: relationship to antithrombotic medications. Stroke. 2021;52(7):2347–55.
Cheng Y, Wang Y, Song Q, Qiu K, Liu M. Use of anticoagulant therapy and cerebral microbleeds: a systematic review and meta-analysis. J Neurol. 2021;268(5):1666–79.
Soo YO, Yang SR, Lam WW, Wong A, Fan YH, Leung HH, et al. Risk vs benefit of anti-thrombotic therapy in ischaemic stroke patients with cerebral microbleeds. J Neurol. 2008;255(11):1679–86.
Costa AF, Zambrano M, Del Brutto OH. Relationship between the neutrophil-to-lymphocyte ratio and silent cerebral small vessel disease in community-dwelling older adults. The Atahualpa Project. Geriatr Gerontol Int. 2017;17(12):2637–9.
Nam K-W, Kwon H-M, Jeong H-Y, Park J-H, Kim SH, Jeong S-M, et al. High neutrophil to lymphocyte ratio is associated with white matter hyperintensity in a healthy population. J Neurol Sci. 2017;380:128–31.
Gu Y, Gutierrez J, Meier IB, Guzman VA, Manly JJ, Schupf N, et al. Circulating inflammatory biomarkers are related to cerebrovascular disease in older adults. Neurol Neuroimmunol Neuroinflamm. 2019;6(1): e521.
Chamorro A, Meisel A, Planas AM, Urra X, Van De Beek D, Veltkamp R. The immunology of acute stroke. Nat Rev Neurol. 2012;8(7):401.
Macrez R, Ali C, Toutirais O, Le Mauff B, Defer G, Dirnagl U, et al. Stroke and the immune system: from pathophysiology to new therapeutic strategies. Lancet Neurol. 2011;10(5):471–80.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
SD, UB have substantial contributions to the conception and design of the work; SD, UB, AE, PG, BK, SM, AE have substantial contributions to the acquisition, analysis, and interpretation of data; SD, UB, AE have drafted the work or substantively revised I; SD, UB, AE, PG, BK, SM, AE approved the submitted version (and any substantially modified version that involves the author's contribution to the study); SD, UB, AE, PG, BK, SM, AE agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Cyprus International University Faculty of Medicine (number EKK21-22/04/001, date 11/11/2021). All study protocols and procedures were conducted in accordance with the declaration of Helsinki. Informed written consent was taken from all participants for participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Diker, S., Gelener, P., Eker, A. et al. Association between cerebral microbleeds and inflammatory biomarkers in patients with ischemic stroke. Egypt J Neurol Psychiatry Neurosurg 58, 43 (2022). https://doi.org/10.1186/s41983-022-00478-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-022-00478-6