Abstract
Background
Hemiplegic shoulder pain (HSP) is one of the most common complications of stroke. This work aimed to evaluate and analyze the clinical and radiological features of painful shoulder in hemiplegic stroke patients with evaluating the diagnostic role of shoulder ultrasound and shoulder MR imaging in assessment of the causes of shoulder pain.
Methods
210 stroke patients with shoulder affection within 3 years of stroke development were enrolled. Clinical assessment including Medical Research Council scoring, The Brunnström motor recovery and Ashworth Scale. Shoulder ultrasound and MR imaging were done for 74 patients with painful hemiplegic shoulder.
Results
The prevalence of HSP was 35.2% with statistically significantly higher proportion of shorter disease duration, lower muscle power, lower BMR stage with higher proportion of bicipital tendinitis and complex regional pain syndrome in major versus moderate dependence (P < 0.001, P < 0.001, P < 0.001, P = 0.011 and P = 0.001 respectively). On multivariate analysis only short disease duration was statistically significant independent predictor. Participants with disease duration ≤ 2 months have 21.9 times higher odds to exhibit major rather than moderate dependence. By imaging there was high prevalence of joint effusion (47.3%), bicipital tendinitis (44.6%), bursitis (31%) and adhesive capsulitis (29.7%) in painful hemiplegic shoulder with a very good agreement between MRI and US in diagnosis.
Conclusion
HSP has a high prevalence in stroke patient with increased morbidity due to various factors and US can be used as an alternative or a complementary to MRI for diagnosis of hemiplegic shoulder pain.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Stroke is a focal neurological deficit representing the second cause of death and the third cause of disability all over the world [1, 2]. Several medical complications of stroke are detected such as deep venous thrombosis, infections and hemiplegic shoulder pain (HSP). These complications hinder rehabilitation program with increased mortality and morbidity rate [3].
HSP is one of the most common complications of stroke with incidence ranged from 11 to 40% in many studies [4] and commonly interferes with patient’s quality of life and usually forces patient to compensate by using the unaffected parts in their activities [5]. Majority of HSP develop in first 2 weeks up to 6 months and about 65% of those will continue to experience the problem several months’ after that [6].
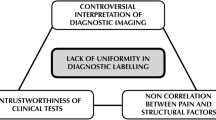
The end results of structural injury and bad posturing of the hemiplegic shoulder with subsequent surrounding tissue damages are reduction in arm function, difficulty with rehabilitation and impaired quality of life [6, 7]. Etiologies of HSP are multifactorial including either central etiology (central post stroke pain), local mechanical causes (rotator cuff tears, shoulder subluxation, bicipital tendonitis, weakness, muscle imbalance and altered scapula position) or neurological factors (weakness, spasticity and altered sensation) [7, 8].
Clinical diagnosis of HSP mainly depending on detecting the source of the pain including changes in pain sensitivity to stimulus, pain arising from joint malalignment, muscle stiffness or shoulder-hand syndrome [9].
Magnetic resonance (MR) and ultrasound imaging (US) are considered as valuable diagnostic imaging tools that used for the evaluation of shoulder disorders. US is a less expensive and non-invasive imaging tool without ionizing radiation that permits both anatomical and functional assessments of the joint [10]. MR is considered as a reference standard for the evaluation of shoulder disorders that can provide both anatomical and structural information about the gleno-humeral joint and rotator cuff muscles [11].
Many studies compared the diagnostic accuracy of ultrasound and MRI in assessment of hemiplegic shoulder pain [10, 11]. In other hand up to the authors’ knowledge there were no previous researches correlating the clinical and radiological features of hemiplegic shoulder pain.
This work aimed to evaluate and analyze the clinical and radiological features of painful shoulder in hemiplegic stroke patients with evaluating the diagnostic role of shoulder ultrasound and shoulder MR imaging in assessment of the causes of shoulder pain.
Methods
This was a cross sectional study performed in period from January 2021 to October 2021 on 210 shoulder affection stroke patients attended outpatient clinic neurology and rehabilitation departments. The study was approved by the Institutional Review Board (IRB), Faculty of Medicine.
All patients recruited in our research gave informed written consent. The demographic and clinical data including age, sex, hemiplegic side (right or left), stroke type (ischemic or hemorrhagic), stroke duration in month, presence or absence of shoulder pain, grade of muscle weakness, Barthel index (BI), sensory disturbance for light touch, Brunnström motor recovery (BMR), Ashworth scale, visual analogue scale (VAS), pattern of shoulder affection and stroke risk factors. All patients were evaluated by expert rheumatologist and neurologist.
Inclusion criteria was stroke patient with shoulder involvement including both sex and age (from 30 to 80 years) while patients with cognitive dysfunction, rheumatic diseases or suffered from any chronic pain prior to stroke were excluded.
Two hundred and ten stroke patients with shoulder affection within 3 years of stroke development were enrolled. Shoulder pain was defined as pain in the shoulder area required analgesia for 2 or more consecutive days and its intensity would be graded on VAS [4].
Demographic data of the patients in this study included right or left handed, duration of stroke, range of motion (ROM) of shoulder joints, level of spasticity in the hemiplegic upper extremities and history of use of anti-spastic agents. The level of spasticity in the affected upper extremities was measured using the Ashworth scale.
Muscle power of the shoulder girdle was examined in each direction when performing the motions of abduction, adduction, flexion and extension using the Medical Research Council scoring system [12], the score was summed to give a composite muscle power score: grade 5 (muscle contracts normally against full resistance), grade 4 (muscle strength is reduced but muscle contraction can still move joint against resistance), grade 3 (muscle strength is further reduced such that the joint can be moved only against gravity with the examiner’s resistance completely removed) grade 2 (muscle can move only if the resistance of gravity is removed), grade 1 (only a trace or flicker of movement is seen or felt in the muscle or fasciculation’s are observed in the muscle) and grade 0 (no movement is observed).
The Brunnström motor recovery (BMR) stages, gleno-humeral subluxation, passive ROM of the hemiplegic shoulder and shoulder pain also was evaluated for all patients. The BMR stages in the upper extremity were: stage I (flaccid limbs without any voluntary movement), stage II (spasticity with weak flexor synergy), stage III (voluntary movement of the limbs, but the action was within a flexor synergy pattern), stage IV (selective activation of muscles outside the flexor synergy), stage V (decrease in muscle spasticity with selective muscle activation which was mostly selective and independent of limb flexor synergy) and stage VI (well-coordinated movements) [13].
Barthel Index score (BI) is an ordinal scale consisting of ten tasks (total score from 0 to 100) used to assess performance in the activities of daily living (ADL) with low scores need greater nursing dependency [14].
Ashworth Scale evaluates the resistance for passive movement around the joint with different degree of velocity with scores from 0 to 4 (0 indicate no increase in tone while 4 indicate limb rigid in flexion or extension) [15].
VAS Scale is a scale used for measurement of pain intensity in different diseases including rheumatoid arthritis comprised of vertical or horizontal line usually 100 mm in length [16, 17].
Imaging techniques
MRI and ultrasound of the affected shoulder were done for all patients presented with shoulder pain. The nature of the studies was explained to all patients and or their caregivers. Shoulder ultrasound and MR imaging were done for 74 patients who suffered from shoulder pain. Imaging was done by single radiologist with more than 10-year experience in musculoskeletal imaging. US examination was performed first then shoulders MRI for all 74 patients on separate cession for each examination.
Shoulder US examination was done for all 74 patients using TOSHIBA ultrasound machine (Xario 200, Canon Medical System, Toshiba, Japan) with linear phased array transducer ranging from 7 to 14 MHz. by using technique previously described by Mack et al. [18] and Middleton [19] in which the patient with exposed shoulder was sit on a rotating chair. This technique allows easy assessment of both ventral and dorsal parts of the shoulder and facilitates any need for change position during examination. US imaging was done in both longitudinal and transverse axis planes for rotator cuff, subacromial/subdeltoid bursa and biceps tendon groove.
Shoulder MR imaging were done for all 74 patients using Siemens 1.5 T MR machine (Magnetom aera, Siemens health care, Germany) with a surface array shoulder coil. On the MR table the patient laid in supine position, the examined shoulder was in horizontal position and the patient’s arm by his side. The protocol of MR shoulder included:
-
Fat-suppressed proton sequences in coronal oblique, sagittal oblique and axial planes with repetition time (TR) 1500 ms, echo-time (TE) 25 ms, field of view (FOV) 120 mm and slice thickness 4 mm.
-
T2 weighted FSE imaging in sagittal oblique and coronal oblique planes with TR 1800 ms, TE 100 ms, FOV 120 mm and slice thickness 4 mm.
-
T1 weighted FSE imaging in axial and coronal oblique planes with TR 400 ms, TE 20 ms, FOV 120 mm and slice thickness 4 mm.
Image analysis
In both US and MR images all the following were evaluated: presence of glenohumeral joint effusion, rotator cuff disorders, sub-acromion/sub-deltoid bursal fluid, acromio-clavicular joint capsular hypertrophy (Figs. 1, 2), long head of biceps tendinitis, effusion or tear (Figs. 3, 4) and signs of adhesive capsulitis (including thickening of the glenohumeral joint capsule, thickening of coraco-humeral ligament, thickening of axillary pouch, obliteration of sub-coracoid fat triangle, increase the MR T2 signal of the rotator cuff joint capsule in MR images or restriction of abduction and external rotation of the shoulder on dynamic US imaging) (Fig. 5) [20, 21].
Shows MRI and US images of different patients with rotator cuff disorders. A Coronal oblique fat-suppressed proton image of the left shoulder shows left supraspinatus partial thickness tendon tear (black arrow), sub-acromion/sub-deltoid bursal fluid (white arrows), A-C joint capsular hypertrophy (thick white arrow) and gleno-humeral joint effusion (asterisks). B Coronal oblique fat-suppressed proton image of the left shoulder of the same patient in A shows fluid filled intramuscular gap (asterisks) is seen in the teres minor muscle (white arrows) diagnostic of intramuscular teres minor tear. C Axial fat suppressed proton image of left shoulder in another patient than A and B shows partial thickness subscapularis tendon tear (black arrow) and gleno-humeral joint effusion (asterisks). D US image of another patient than A and C shows hypo-echoic full-thickness defect within the left supraspinatus tendon (black arrow) diagnostic of supraspinatus full thickness tear
Shows MRI and US images of two different patients with rotator cuff disorders. A Coronal oblique fat-suppressed proton image of the left shoulder shows increase supraspinatus tendon thickness with high signal areas inside diagnostic of left supraspinatus tendinitis (black arrow). B US image of another patient than A shows increase supraspinatus tendon thickness with hypoechoic areas inside (asterisks) diagnostic of supraspinatus tendinitis with multiple hyperehoic supraspinatus tendon calcification (white arrows)
Shows MRI and US images of two different patients with long head of biceps tendinitis/effusion. A Axial fat-suppressed proton image of the left shoulder shows fluid signal within bicipital groove (white arrow) with thickened hypo-intense biceps tendon inside and gleno-humeral joint effusion (asterisks). B US image of another patient than A shows biceps tendinitis and bicipital groove effusion (white arrow)
Shows MRI and US images of 65 years old patient with long head of biceps tendon complete tear and retraction. A Axial fat suppressed proton image shows empty bicipital groove (no tendon inside) (black arrow). B Coronal oblique fat-suppressed proton image of the right shoulder shows downward retracted long head of biceps tendon (black arrow). C US image of the same patient shows empty bicipital groove (no tendon inside) (white arrow)
shows right shoulder MRI of 45 years old male patient with adhesive capsulitis; A Axial fat-suppressed proton image, B Coronal oblique fat-suppressed proton image and C Sagittal oblique T2 images show thickened inferior gleno-humeral ligament (white arrow in A), bicipital tendinitis and effusion (black arrow in A), increase thickness of axillary pouch capsule (curved white arrows in B), thickened coraco-humeral ligament (white arrow in C) and obliteration of sub-coracoid fat triangle (asterisk in C). MRI images also show supraspinatus tendinitis (thick white arrow in B), Hill sachs lesion (thin white arrow in B), subacromial bursitis (black arrow in B) and gleno-humeral joint effusion (asterisks in A and B). D Axial US image of right shoulder of the another patient with adhesive capsulitis shows rotator cuff interval containing long head of biceps (LHB), thickened coraco-humeral ligament (asterisk) and thickened superior gleno-humeral ligament (curved white arrow)
Rotator cuff disorders including diagnoses of rotator cuff muscles complete tear, partial tear, tendinitis or atrophy. US signs used for diagnosis of rotator cuff full thickness tear included presence of hypo-echoic full-thickness defect within the tendon. US signs used for diagnosis of rotator cuff partial thickness tear were presence of multiple hypo-echoic areas within the tendon (> 3 mm in size) that was not reach tendon margins. US signs used for diagnosis of rotator cuff tendinitis was heterogeneous echo-pattern with increase tendon thickness more 8 mm [22].
Tendon effusion diagnosed by US as presence of compressible, freely mobile and anechoic fluid with no vascularity on color Doppler around the tendon [22]. Sub-acromion/sub-deltoid bursal fluid diagnosed by US as presence of linear anechoic fluid collection more than 2 mm in thickness present between the deltoid muscle and the tendons of supraspinatus and infraspinatus muscles [10].
Statistical analysis
Data were entered and analyzed using IBM-SPSS software (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). Qualitative data were expressed as N (%). Chi-square test or Fisher’s exact test according to sample size of cells (expected counts) was used for comparing qualitative data. Quantitative data were initially tested for normality using Shapiro–Wilk’s test with data being normally distributed if P > 0.050. Presence of significant outliers (extreme values) was tested for by inspecting boxplots. Quantitative data were not normally distributed, so data were expressed as median and interquartile range (IQR) and compared between two groups using Mann–Whitney U test. The cutoff point of a test to discriminate diseased cases from non-diseased cases was evaluated using Receiver Operating Characteristic (ROC) curve analysis. Binary logistic regression analysis was used to predict the likelihood of occurrence of major versus moderate dependence. Crude odds ratio was initially calculated for each predictor and then a model was run to get the odds ratios of independent predictors. For any of the used tests, results were considered as statistically significant if P value ≤ 0.050 and appropriate charts were used to graphically present the results whenever needed.
Results
The demographic and clinical data including age, sex, hemiplegic side (right or left), stroke type (ischemic or hemorrhagic), stroke duration in month, presence or absence of shoulder pain, grade of muscle weakness, BI, sensory disturbance for light touch, BMR, Ashworth scale, VAS, pattern of shoulder affection and stroke risk factors are collected and analyzed.
Table 1 showed statistically significantly higher proportions of female sex, left-sided hemiplegia, hemorrhagic stroke, adhesive capsulitis, supraspinatous calcification, and diabetes mellitus (DM) in those with shoulder pain versus those without. It also showed shorter disease duration, lower BIS, and lower BMR stage in those with shoulder pain versus those without. The following parameters were observed in those with shoulder pain only: Sensory disturbance for light touch, shoulder subluxation, shoulder joint effusion, bicipital Tendinitis, acromio-clavicular joint capsular hypertrophy, Rotator Cuff disorders and CRPS. Also, those with shoulder have median VAS score of 2.
Table 2 showed statistically significantly higher proportions of female sex, shorter disease duration (Fig. 6), lower muscle power (Fig. 7), lower BMR stage (Fig. 8), and higher proportion of bicipital tendinitis and CRPS in major versus moderate dependence. The following parameters were observed in those with major shoulder pain only: adhesive capsulitis, supraspinatus calcification and right-sided hemiplegia.
Table 3 showed the results of binary logistic regression analysis which was run to ascertain the effects of disease duration, muscle power score, sex, nature of stroke (ischemic vs hemorrhagic), sensory disturbance, bicipital tendinitis and complex regional syndrome. On the likelihood that participants with stroke will exhibit major dependence rather than moderate dependence.
On univariate analysis all 7 predictor variables were statistically significant. Multivariate analysis was run incorporating 6 of these variables. Muscle power was excluded due to very few cases in major group (only one case with power more than 3). The model was statistically significant (χ2[6] = 41.760, P less than 0.001). The model correctly classified 86.5% of cases with sensitivity and specificity of 85.7% and 88%, respectively. Of the 6 predictor variables only short disease duration was statistically significant independent predictor. Participants with disease duration ≤ 2 months have 21.9 times higher odds to exhibit major rather than moderate dependence.
Shoulder ultrasound and MR imaging were done for 74 hemiplegic patients who suffered from shoulder pain. From 74 patients MR imaging was normal in 19 patients (25.6%) and was abnormal in 55 patients (74.3%) while US was normal in 21 patients (28.3%) and was abnormal in 53 patients (71.6%). The most detected imaging finding were shoulder joint effusion (47.3%) followed by bicipital Tendinitis (44.6%) and then sub acromial sub deltoid/sub acromial bursitis (31.1%).
Adhesive capsulitis was diagnosed in 22 patients by MRI and in 20 patients by US (two patients were missed by US). Subacromial/subdeltoid bursitis was diagnosed in 23 patients by MRI and in 19 patients by US (four patients were missed by US). Bicipital tendinitis, effusion or tear was diagnosed in 33 patients by MRI and in 31 patients by US (two patients were missed by US). Shoulder subluxation was diagnosed in 10 patients by MRI and in 8 patients by US (two patients were missed by US). Gleno-humeral joint effusion was diagnosed in 35 patients by MRI and in 31 patients by US (four patients were missed by US). Acromio-clavicular joint capsular hypertrophy was diagnosed in 6 patients by both MRI and US. Rotator cuff disorders were diagnosed in 19 patients by MRI and in 15 patients by US. Four patients were missed by US as the pathologies were small and hidden by the acromion shadow (Table 4).
By using MRI as a reference standard US showed high sensitivity and specificity in diagnosis of adhesive capsulitis, bicipital tendinitis, effusion or tear, and acromio-clavicular joint capsular hypertrophy. US showed moderate sensitivity and high specificity in diagnosis of Subacromial/Subdeltoid bursitis, Gleno-humeral joint effusion, and Rotator Cuff disorders. US showed moderate sensitivity and specificity in diagnosis of shoulder subluxation (Table 5).
Cohen’s κ was run to determine if there was agreement between the two radiological modalities (US & MRI) judgment on presence or absence of 10 parameters assessed in the 74 patients. There was moderate agreement (k = 0.41–0.60) between the two modalities’ judgments for Shoulder subluxation, good agreement (k = 0.61–0.80) for Supraspinatus complete tear, Supraspinatus partial tear, Supraspinatus tendinopathy, and Supraspinatus atrophy. There was very good agreement (k = 0.81–1.00) for other parameters, adhesive capsulitis, Subacromial subdeltoid bursitis, bicipital tendinitis, effusion or tear and gleno-humeral joint effusion, and perfect agreement for acromio-clavicular joint capsular hypertrophy (Table 6).
Discussion
Hemiplegic shoulder pain is the fourth medical complication after a stroke alongside post stroke depression, falls, and infection especially in urinary tract [23]. The prevalence of hemiplegic shoulder pain in our study was 35.2% while was varying in different studies between 16 and 84% the discrepancy in prevelences between different studies can be attributed to many reasons as pain is a subjective and more difficult to be evaluated and expressed especially in stroke patients with cognitive impairment, aphasia or dysarthria also using different ways for pain definition in different studies (using questionnaires or pain with passive movement) [24,25,26].
The current study revealed that females had higher stroke incidence than males this was agreed with Girijala et al. [27] they found that stroke incidence was common in females than males also shoulder pain had a higher statistically significant in females than males (P = 0.019). Female sex considers one of the most important predictors for development of post stroke shoulder pain in addition to old age and sensory deficit [28]. Westerlind et al. found that gender did not significantly contribute to the final development of post stroke shoulder pain [29], but disagreed with Wang et al. they found stroke was higher incidence in men than women and this was partly explained by several different risk factors between males and females [30].
This study revealed that prevalence of left sided hemiplegia was higher than right sided and those patients with left sided were more prone to develop shoulder pain (P < 0.001). This was agreed with Lindgren et al. they found that left sided hemiparesis considered one of the most important factors to develop shoulder pain in addition to decrease passive shoulder range of abduction and pain frequency [31].
As regard type of stroke this study found that patients with ischemic stroke were statistically significant higher when compared with hemorrhagic stroke (P < 0.001) this was concordant with many studies [28, 32].
The current study revealed that sensory disturbance for light touch was statistically significant higher in patients with shoulder pain versus patients without shoulder pain (P < 0.001) many studies reported that sensory disturbance was one of the most important risk factor for development of hemiplegic shoulder pain [6, 33,34,35].
As regard risk factors for stroke only diabetes mellitus (DM) showed statistically significant effect as risk factor for development of HSP (P = 0.006) this was concordant with Thomas et al. [36] also with Klit et al. [37] they found that DM patients were twice more likely to develop post-stroke shoulder pain versus stroke patients without DM and was attributed to the numerous complications of DM including musculoskeletal particular shoulder pain but other risk factors of stroke like hypertension, ischemic heart disease (IHD), atrial fibrillation (AF), smoking nor dyslipidemia did not exhibit any statistically difference between patients with HSP and without pain.
This research exhibit that shoulder pain was evident in the first 6 months from stroke onset in which the shorter duration of the disease was highly statistically significant when comparing patients with HSP versus patients without HSP (P < 0.001), Poduri [38] found that shoulder pain can occur early post stroke in first 2 weeks but the typical onset was 2–3 months after stroke onset. many factors may contribute to early development of HSP including neurological factors (initial flaccid paralysis, impaired sensation and hemispatial neglect) and factors attributed to shoulder joint (subluxation of the humeral head or rotator cuff injury) [39,40,41,42].
In this study during assessment of daily living activities using Barthel index score we found that patients with HSP had lower score performance when compared with those without hemiplegic shoulder pain this was highly statistically significant lower (P < 0.001). This was consistent with Roy et al. [43] they found that patients with HSP had impaired arm function with poor performance on BI score and showed also a longer hospital stay period in acute stroke.
The current study revealed that stroke patients with shoulder pain had statistically significant lower recovery stages when comparing stroke patients without shoulder pain (P = 0.010) this was in agreement with Yetisgin [44] who found patients with shoulder pain had lower Brunnstrom hand stage when comparing patients without shoulder pain.
This study exhibited that there was no statistically significant difference between hemiplegic patients with and without shoulder pain as regard age, number of risk factors for stroke, muscle power score and Ashworth scale while VAS scale was statistically significant in patients with HSP.
When we compared patients with major dependence and those with moderate dependence on BI score we found that majority of patients with shoulder pain had major dependent with higher statistical significant in females than males (P = 0.031).
In current research we found that there were statistically significantly higher proportion of shorter disease duration, lower muscle power, lower BMR stage and higher proportion of bicipital tendinitis and CRPS in major vs. moderate dependence (P < 0.001, P < 0.001, P < 0.001, P = 0.011 and P = 0.001 respectively).
As regard predictors of the likehood of major versus moderate dependence we found the short disease duration was statistically significant independent predictors on multivariate analysis (P < 0.001) while binary logistic regression analysis on disease duration, muscle power score, sex, nature of stroke (ischemic vs hemorrhagic), sensory disturbance, bicipital tendinitis and complex regional syndrome were statistically significant (P < 0.001, P < 0.001, P = 0.037, P = 0.002, P = 0.002, P = 0.013 and P = 0.006 respectively) on univariate analysis.
In this study shoulder ultrasound and MR imaging were done for 74 patients who suffered from shoulder pain. From 74 patients MR imaging was normal in 19 patients (25.6%) and was abnormal in 55 patients (74.3%) while US was normal in 21 patients (28.3%) and was abnormal in 53 patients (71.6%). The two missed cases by US were diagnosed by MRI as minimal subacromial/subdeltoid bursitis and early adhesive capsulitis.
In the current study the prevalence of gleno-humeral joint effusion, bicipital tendinitis, effusion or tear, subacromial/subdeltoid bursitis, adhesive capsulitis, rotator cuff disorders, shoulder subluxation, and acromio-clavicular joint capsular hypertrophy in painful hemiplegic shoulder were 47.3%, 44.6%, 31%, 29.7, 25.6%, 13.5% and 8% respectively.
Many studies stated that there was high prevalence of bicipital tendinitis, gleno-humeral joint effusion and sub-acromial/sub-deltoid bursitis in patients with hemiplegic shoulder pain [45, 46]. These were matched with current study as we concluded that there was high prevalence of gleno-humeral joint effusion, bicipital tendinitis and sub-acromial/sub-deltoid bursitis in 74 hemiplegic patients with shoulder pain.
In the current study the incidence of adhesive capsulitis was relatively high (29.7%) and this was in agreement with the study of Tavora et al. they concluded that adhesive capsulitis of gleno-humeral joint was significantly higher in hemiplegic shoulder than in other shoulder disorders [47].
In the current study MRI diagnosed 22 patients with adhesive capsulitis while US diagnosed 20 patients with US sensitivity 90.9%, specificity 94.2% and accuracy 93.2%. The two missed cases by US were diagnosed as early adhesive capsulitis by MRI. This was in agreement with the study of Choi and Kim as they reported that MRI could diagnose the increasing of axillary recess capsular thickening and the increasing of T2 signal intensity that occurs in early stage of adhesive capsulitis [21].
In the current study MRI diagnosed 23 case of subacromial/subdeltoid bursitis while US diagnosed 19 cases with high US sensitivity (82.6%) and specificity (98%). The four missed cases by US were diagnosed as minimal subacromial/subdeltoid bursitis by MRI. This was in agreement with the study of El-Shewi et al. they reported that US is less accurate in diagnosis minimal subacromial/subdeltoid bursitis [48]. This study was also in agreement with the study of Zaiton et al. they reported that US had high sensitivity and specificity for diagnosis of subacromial/subdeltoid bursitis (81% and 98%, respectively) [46].
In the current study US diagnosed 31 cases of gleno-humeral joint effusion while MRI diagnosed 35 cases with high US sensitivity (88.5%) and specificity (100%). The four missed cases by US were diagnosed as minimal effusion by MRI. This was in agreement with the studies of Melanie et al. and Mc Nally et al. they reported that US able to discriminate between synovial fluid and the hypoechoic thickened synovium by compression test [49, 50].
In this study there were very good US and MRI agreement for diagnosis of adhesive capsulitis, Subacromial subdeltoid bursitis, bicipital tendinitis, effusion or tear and gleno-humeral joint effusion. This was in agreement with the study of Choi and Kim they reported that there was a good correlation between ability of MRI and US for accurate measurements of axillary recess capsule thickness in patient with adhesive capsulitis [21]. Also this study results were in agreement with study of Zaiton et al. they reported that there was excellent agreement between US and MRI in diagnosis of subacromial/subdeltoid bursitis, diagnosis of bicipital tendinitis, effusion or tear and diagnosis of gleno-humeral joint effusion [46].
In the current study US diagnosed 8 cases of shoulder subluxation while MRI diagnosed 10 cases with 80% US sensitivity, 85.9% US specificity and a moderate US and MRI agreement for diagnosis of shoulder subluxation (kappa = 0.509). This was matched with the study of the Simao et al. they reported that US sensitivity for diagnosis of gleno-humeral joint instability ranged from 20 to 100% and specificity ranged from 25 to 90% [51].
In this study US showed lower sensitivity and specificity than MRI for diagnosis of rotator cuff disorders with a good US and MRI agreement. This was explained in the study of Lenza et al. they concluded that small supraspinatus tendon thickness tears could be missed by US [52].
Our results were matched with the study of El-Shewi et al. they reported the same US sensitivity with our study (83%) for diagnosis of rotator cuff tendinitis and the study of Strobel et al. concluded that US had lower accuracy than MRI in diagnosis of rotator cuff atrophy. [48, 52, 53].
Ii this study US showed the same sensitivity, specificity and accuracy (100%) as MRI in diagnosis of acromio-clavicular joint capsular hypertrophy with perfect agreement (100%) between US and MRI. This was in agreement with the studies of El-Shewi et al. and Melanie et al. as they concluded that dynamic US can directly visualized degenerative changes of acromio-clavicular joint [48, 49].
This study concluded that shoulder US had high accuracy in diagnosis of acromio-clavicular joint capsular hypertrophy, bicipital tendinitis, effusion or tear, Gleno-humeral joint effusion, adhesive capsulitis, and Subacromial/Subdeltoid bursitis. US had moderate accuracy in diagnosis of rotator Cuff disorder and shoulder subluxation.
This study concluded that there were perfect agreement between shoulder US and MRI for diagnosis of acromio-clavicular joint capsular hypertrophy, very good agreement in diagnosis of adhesive capsulitis, subacromial/subdeltoid bursitis, bicipital tendon disorders and gleno-humeral joint effusion, good agreement for diagnosis of rotator cuff disorders and moderate agreement for diagnosis of shoulder subluxation.
US can be used as an alternative or a complementary to MRI for diagnosis of hemiplegic shoulder disorders. The choice between both techniques depends on the clinical condition of the patients, availability of the techniques and the operator US skills. The advantage of US over MRI it is cheaper, not time-consuming, and more applicable for obese patients, critically ill patients and patients who have contraindication for MRI. Also US permit both anatomical and functional assessments of the joint by evaluation of both tissue structure and the dynamic movement of the affected hemiplegic shoulder.
The first limitation of this study was the absence of assessment of depression for the patients enrolled in the study. The second limitation was absence of the correlation between the site and size of the brain insult and their relation with hemiplegic shoulder pain as in this research we studied the local mechanical causes of HSP. Further studies are required to assess the central causes of HSP.
Conclusion
HSP has a high prevalence in stroke patients with increased morbidity due to various factors that commonly interferes with patient’s quality of life and rehabilitation program if not identified and treated early. US can be used as an alternative or a complementary to MRI for diagnosis of hemiplegic shoulder pain.
Availability of data and materials
The data supporting the results of this article are included within the article.
Abbreviations
- HSP:
-
Hemiplegic shoulder pain
- MRI:
-
Magnetic resonance imaging
- US:
-
Ultrasound
- BI:
-
Barthel index
- BMR:
-
Brunnström motor recovery
- VAS:
-
Visual analogue scale
- ROM:
-
Range of motion
- RT:
-
Repetition time
- FOV:
-
Field of vie
- IQR:
-
Interquartile range
- ROC:
-
Receiver Operating Characteristic
- IHD:
-
Ischemic heart disease
- AF:
-
Atrial fibrillation
- COR:
-
Crude odds ratio
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- DM:
-
Diabetes mellitus
- TP:
-
True positive
- FN:
-
False negative
- TN:
-
True negative
- FP:
-
False positive
- A-C:
-
Acromio-clavicular
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- SE:
-
Standard error
References
WHO. The 10 leading causes of death by broad income group, 2008. In: The top 10 causes of death. Geneva: World Health Organization; 2011.
Pinzon RT, Wijaya VO. Complications as poor prognostic factors in patients with hemorrhagic stroke: a hospital-based stroke registry. Int J Neurol Neurother. 2020;7:096.
Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ Res. 2017;120:439–48.
Akhlaq U, Ayaz SB, Akhtar N, Khan AA. Frequency and intensity of shoulder pain after stroke: a hospital based study. Pak Armed Forces Med J. 2016;66(1):71–4.
Bonifer N, Anderson KM. Application of constraint-induced movement therapy for an individual with severe chronic upper-extremity hemiplegia. Phys Ther. 2003;83:384–98.
Paolucci S, Iosa M, Toni D, Barbanti P, Bovi P, Cavallini A, et al. Prevalence and time course of post-stroke pain: a multicenter prospective hospital-based study. Pain Med. 2016;17:924–30.
Vasudevan JM, Brownie BJ. Hemiplegic shoulder pain: an approach to diagnosis and management. Phys Med Rehabil Clin N Am. 2014;25:411–37.
Bender L, McKenna K. Hemiplegic shoulder pain: defining the problem and its management. Disabil Rehabil. 2001;23(16):698–705.
Kilt H, Finnerup NB, Jensen TS. Central post-stroke pain: clinical characteristics, pathophysiology, and management. Lancet Neurol. 2009;8:857–68.
Doğun A, Karabay I, Hatipoğlu C, Özgirgin N. Ultrasound and magnetic resonance findings and correlation in hemiplegic patients with shoulder pain. Top Stroke Rehabil. 2014;21(Suppl 1):S1-7.
Pompa A, Clemenzi A, Troisi E, Mario MD, Tonini A, Pace L, et al. Enhanced-MRI and ultrasound evaluation of painful shoulder in patients after stroke: a pilot study. Eur Neuro. 2011;66(3):175–81.
Medical Research Council. Aids to the examination of the peripheral nervous system. Memorandum No. 45. London: Her Majesty’s Stationary Office; 1976.
Brunnstrom S. Movement therapy in hemiplegia: a neurophysiological approach. New York: Harper & Row. Movement Therapy in Hemiplegia Brunnstrom. 1970.
Terence JQ, Langhorne P, Stott DJ. Barthel Index for stroke trials. Development, properties, and application. Stroke. 2011;42:1146–51.
Brashear A, Zafonte R, Corcoran M, Galvez-Jimenez N, Gracies JM, Gordon MF, et al. Inter- and intrarater reliability of the Ashworth Scale and the Disability Assessment Scale in patients with upper-limb poststroke spasticity. Arch Phys Med Rehabil. 2002;83:1349–54.
McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med. 1988;18:1007–19.
Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117–26.
Mack LA, Nyberg DA, Matsen FA III. Sonographic evaluation of the rotator cuff. Radiol Clin Northm Am. 1988;26:161.
Middleton WD. Ultrasonography of the shoulder. Radiol Clin North Am. 1992;30:927.
Tandon A, Dewan S, Bhatt S, Jain AK, Kumari R. Sonography in diagnosis of adhesive capsulitis of the shoulder: a case–control study. J Ultrasound. 2017;20:227–36.
Choi YH, Kim DH. Correlations between clinical features and MRI findings in early adhesive capsulitis of the shoulder: a retrospective observational study. BMC Musculoskelet Disord. 2020;2020(21):542.
Lee IS, Shin YB, Moon TY, Jeong YJ, Song JW, Kim DH. Sonography of patients with hemiplegic shoulder pain after stroke: correlation with motor recovery stage. Am J Roentgenol. 2009;192:W40–4.
Janus-Laszuk B, Mirowska-Guzel D, Sarzynska-Dlugosz L, Czlon-kowska A. Effects of medical complications on the after- stroke rehabilitation outcome. Neuro-Rehabilitation. 2017;40(2):223–32.
Koog YH, Jin SS, Yoon K, Min BI. Interventions for hemiplegic shoulder pain: systematic review of randomised controlled trials. Disabil Rehabil. 2010;32(4):282–91.
Zorowitz RD, Hughes MB, Idank D, Ikai T, Johnston MV. Shoulder pain and subluxation after cerebrovascular accident: correlation or coincidence? Am J Occup Ther. 1996;50(3):194–201.
Cheng P-T, Lee C-E, Liaw M-Y, Wong M-K, Hsueh T-C. Risk factors of hemiplegic shoulder pain in cerebrovascular accident patients. J Musculoskelet Pain. 1995;3(3):59–73.
Girijala RL, Sohrabji F, Bush RL. Sex differences in stroke: review of current knowledge and evidence. Vasc Med. 2017;22(2):135–45.
Harrison RA, Field TS. Post stroke pain: identification, assessment, and therapy. Cerebrovasc Dis. 2015;39(3–4):190–201.
Westerlind E, Singh R, Persson HC, Katharina S. Experienced pain after stroke: a cross-sectional 5-year follow-up study. BMC Neurol. 2020;20:4.
Wang Y, Dai Y, Zheng J, Xie Y, Guo R, Guo X, et al. Sex difference in the incidence of stroke and its corresponding influence factors: results from a follow-up 8.4 years of rural China hypertensive prospective cohort study. Lipids Health Dis. 2019;18:72.
Lindgren I, Lexell J, Jönsson AC, Brogårdh C. Left-sided hemiparesis, pain frequency, and decreased passive shoulder range of abduction are predictors of long-lasting poststroke shoulder pain. PMR. 2012;4:561–8.
Lindgren I, Jönsson AC, Norrving B, Lindgren A. Shoulder pain after stroke. A prospective population-based study. Stroke. 2007;38:343–8.
Sackley C, Brittle N, Patel S, Ellins J, Scott M, Wright C, et al. The prevalence of joint contractures, pressure sores, painful shoulder, other pain, falls, and depression in the year after a severely disabling stroke. Stroke. 2008;39:3329–34.
Kwon YH, Kwon JW, Lee NK, Kang KW, Son SM. Prevalence and determinants of pain in the ipsilateral upper limb of stroke patients. Percept Mot Skills. 2014;119:799–810.
Anwer S, Alghadir A. Incidence, prevalence, and risk factors of hemiplegic shoulder pain: a systematic review. Int J Environ Res Public Health. 2020;17(14):4962.
Thomas SJ, McDougall C, Brown IDM, Jaberoo MC, Stearns A, Ashraf R, et al. Prevalence of symptoms and signs of shoulder problems in people with diabetes mellitus. J Should Elb Surg. 2007;16(6):748–51.
Klit H, Finnerup NB, Overvad K, Andersen G, Jensen ST. Pain following stroke: a population-based follow-up study. PLoS ONE. 2011;6:e27607.
Poduri KR. Shoulder pain in stroke patients and its effects on rehabilitation. J Stroke Cerebrovasc Dis. 1993;3(4):261–6.
Yamaguchi K, Sher JS, Andersen WK, Garretson R, Uribe JW, Hechtman K, et al. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Should Elb Surg. 2000;9:6–11.
Chantraine A, Baribeault A, Uebelhart D, Gremion G. Shoulder pain and dysfunction in hemiplegia: effects of functional electrical stimulation. Arch Phys Med Rehabil. 1999;80:328–31.
Vuagnat H, Chantraine A. Shoulder pain in hemiplegia revisited: contribution of functional electrical stimulation and other therapies. J Rehabil Med. 2003;35:49–54.
Meskers CG, Koppe PA, Konijnenbelt MH, Veeger DH, Janssen TW. Kinematic alterations in the ipsilateral shoulder of patients with hemiplegia due to stroke. Am J Phys Med Rehabil. 2005;84:97–105.
Roy CW, Sands MR, Hill LD, Harrison A, Marshall S. The effect of shoulder pain on outcome of acute hemiplegia. Clin Rehabil. 1995;9:21–7.
Yetisgin A. Clinical characteristics affecting motor recovery and ambulation in stroke patients. J Phys Ther Sci. 2017;29(2):216–20.
Pong YP, Wang L-Y, Wang L, Leong CP, Huang Y, Chen YK. Sonography of the shoulder in hemiplegic patients undergoing rehabilitation after a recent stroke. J Clin Ultrasound. 2009;37(4):199–205.
Zaiton F, Tantawy HI, Elsharkawy KAM, Sanad G. Painful post stroke shoulder: comparison of magnetic resonance imaging and high frequency ultrasonography. Egypt J Radiol Nucl Med. 2011;42:47–55.
Távora DGF, Gama RL, Bomfim RC, Nakayama M, Silva CEP. MRI findings in the painful hemiplegic shoulder. Clin Radiol. 2010;65(10):789–94.
El-Shewi IEA, El Azizy HM, Gadalla AAH. Role of dynamic ultrasound versus MRI in diagnosis and assessment of shoulder impingement syndrome. Egypt J Radiol Nucl Med. 2019;50:100.
Melanie F, Karen F, Terry P, Gary S, Peter S, Lawrence F. Sonography of full-thickness supraspinatus tears: comparison of patient positioning technique with surgical correlation. AJR. 2005;184:180–4.
McNally EG, Rees JL. Imaging in shoulder disorders. Skelet Radiol. 2007;36(11):1013–6.
Simao MN, Nogueira-Barbosa MH, Mglia VF, Barbieri C. Anterior shoulder instability: correlation between magnetic resonance arthrography, ultrasound arthrography and intraoperative findings. Ultrasound Med Biol. 2012;4(3):551–60.
Lenza M, Buchbinder R, Takwoingi Y, et al. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. 2013;9:139.
Strobel K, Hodler J, Meyer DC, Pfirrmann CWA, Pirkl C, Zanetti M. Fatty atrophy of supraspinatus and infraspinatus muscles: accuracy of US. Radiology. 2005;237:584–9.
Acknowledgements
The authors are grateful to all patients for their willingness to participate in this study.
Funding
There is no source of funding for the research.
Author information
Authors and Affiliations
Contributions
HAE, CAZ, ASB and AAM carried out the work. HAE and ASB design the protocol, shared collected scientific data and in statistical analysis, AAM and CAZ shared for collecting the scientific data, did the statistical analysis and were responsible for writing the initial draft of the manuscript, CAZ interpreted the radiology of all patients. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors obtained permission to conduct this study that was approved by the Institutional Review Board (IRB), Faculty of Medicine—Mansoura university (Proposal Code Number: R.21.05. 1331). All patients gave written agreement. The procedures followed were in accordance with our protocol. We recruited 210 patients from Outpatient clinics of Neurology, Rheumatology and Rehabilitation Departments, Mansoura University Hospitals.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Sonbaty, H.AE., Abou Elmaaty, A.A., Zarad, C.A. et al. Clinical and radiological assessment of hemiplegic shoulder pain in stroke patients. Egypt J Neurol Psychiatry Neurosurg 58, 41 (2022). https://doi.org/10.1186/s41983-022-00474-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-022-00474-w