Abstract
Background
Chronic obstructive pulmonary disease (COPD) is accompanied by substantial systemic dysregulations that comprise systemic inflammation and neurohormonal activation in addition to many neurological involvements, such as cerebrovascular diseases, polyneuropathies, motor neuron diseases, and cognitive impairment has been described in COPD patients. The aim of the current work was to detect the subclinical affection of the peripheral nervous system in patients with stable COPD.
Results
Forty COPD patients and 30 subjects as healthy control were enrolled. All included subjects were submitted to complete medical history, clinical evaluations, investigations in the form of; arterial blood gases, spirometry, in addition to nerve conduction study. The patients with COPD were classified according to GOLD criteria for severity in grade I in 7.5% grade II in 62.5%, grade III in 20%, and grade IV in 10%. The results show a statistically significant increase in distal latency and a statistically significant decrease of amplitude and conduction velocity in patients with COPD when compared to the examined nerves of control group. The demyelinating nerve affection was the most common.
Conclusion
In COPD patients the peripheral nervous system could be affected subclinically once the severity of COPD increased and the patient should be neurophysiologically observed for early recognition of peripheral nervous system affection.
Similar content being viewed by others
Introduction
COPD is defined as chronic inflammatory lung disease, characterized by progressive pulmonary destruction, shortness of breath, mucus production, and chronic coughing [1]. COPD is the fourth principal reason of death all over the world and an additional increase in the occurrence along with the mortality of the disease is expected to increase for upcoming years. Therefore, there is an impending need to create awareness concerning COPD complication(s) [2]. It is well recognized that COPD is linked to significant systemic abnormalities [3]. Systemic inflammation, neurohormonal activation, Hypoxemia, and hypercapnia, are the chief mechanisms of the pathophysiology of systemic affections [4]. Many neurological affections such as polyneuropathies, motor neuron diseases, cerebrovascular diseases, and cognitive impairment have been described in patients with COPD [5,6,7]. The aim of the present study was to detect the subclinical affection of the peripheral nervous system in patients with stable COPD.
Methods
This study was considered as a case–control study, including 40 patients with COPD and 30 healthy individuals, non-smoker, as a control group, the study was conducted at neurology, internal medicine, and chest departments,
Inclusion criteria: Patients with COPD are diagnosed according to the global initiative for chronic obstructive pulmonary disease (GOLD) criteria [8].
Exclusion criteria: Patients with unstable COPD, Patients with neurological complaints or manifestations suggestive of neuromuscular illness due to co-morbid conditions of COPD (as diabetes mellitus, chronic kidney disease, chronic hepatic disease, and chronic alcoholism).
All included individuals were submitted to the following: (1) complete medical history with an emphasis on the main complaint, age, sex, smoking behaviors, duration of disease, risk factors (pollution, occupation,
Inhabitant area) and medical history of additional systemic diseases. (2) Physical and neurological examination. (3) Arterial Blood Gases including partial arterial oxygen tension, partial arterial carbon dioxide tension, pH, and oxygen saturation all of which were presented in the arterial blood sample, at room air. (4) Spirometry examinations: all patients and control subjects underwent spirometry after the administration of 400 ug of salbutamol whereas the patient was stable; forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and FEV1/FVC ratio were obtained.
Spirometry evaluations were completed according to the American Thoracic Society [9] as follows: (a) Description of the technique to the patient in detail. (b) Making sure that the patient was upright or sitting vertically with feet fixed on the floor. (c) Put on a nasal clip to the patient's nose. (d) Advise the patient to breathe entirely. (e) Closing the lips of the patient around the mouthpiece. (f) Requesting the patient to blast air out as fast and as far as he can until the lungs were empty. (g) Asking the patient to breathe once more as forcibly and entirely as possible. (h) At minimum three technically accepted maneuvers were done [9] the parameters of spirometry were measured to approve the diagnosis and to measure the severity of COPD rendering to GOLD criteria, which categorize patients with COPD into four stages rendering to the value of FEV1; Mild stage of COPD: FEV1/FVC < 0.70 FEV1 ≥ 80% normal, Moderate stage of COPD: FEV1/FVC < 0.70 FEV1 50–79% normal, Severe stage of COPD: FEV1/FVC < 0.70 FEV1 30–49% normal and Very Severe stage of COPD when: FEV1/FVC < 0.70 FEV1 < 30% normal or FEV1 < 50% predicted in addition to chronic respiratory failure. [8].
Nerve conduction studies: were achieved via Nihon Kohden apparatus; Model UT- 0800 J. Box BOARD (2CH) For JB-942BK. Made in Tokyo, Japan. That includes:
Motor nerve conduction: nerve conduction study was operated by electrical stimulation of peripheral nerves (median, ulnar, radial, common peroneal, and posterior tibial nerves) and reporting amplitude, motor latency and conduction velocity from a muscle supplied by these nerves (abductor pollicis brevis, abductor digitiminimi muscle, extensor indices, extensor digitorum brevis, and abductor halluces, respectively) and the ground electrode: Positioned between the recording electrode and the stimulator.
Sensory nerve conduction (sensory NCS) (antidromic): was operated by electrical stimulation of peripheral nerves (median, ulnar, radial, and sural) and reporting the amplitude, sensory latency, and conduction velocity from a purely sensory part of the nerve, (2nd finger, 5th digit, dorsum of 1st web space and the part behind and under the lateral malleolus, respectively) and the ground electrode: Sited between the stimulator and recording electrode.
Diagnosis of peripheral neuropathy: As demyelinating, axonal and mixed according to the criteria in the following table [10]
CMAP amplitude | Nerve conduction velocity | |
|---|---|---|
Demyelinating | Axonal | |
< 50%LLN | < 80%LLN | > 80%LLN |
> 50% LLN | < 90%LLN | > 90%LLN |
The cut off value for motor median, ulnar, radial, tibial and peroneal nerve studies, the least normal compound motor action potentials (CMAP) were 5.2 mv, 4.2 mv, 3.2 mv, 3.6 mv and 3.1 mv, respectively, and the least motor nerve conduction velocity of median, ulnar, radial, tibial and peroneal nerves were 49 m/s, 51.2 m/s, 62.9 m/s, 42.9 m/s and 48.4 m/s, respectively.
The cutoff value for the sensory median, ulnar, radial, and sural nerve studies, the least normal sensory nerve action potentials (SNAP) were 15 uv, 18.9 uv, 16.4 uv, and 10 uv, respectively, and the least sensory nerve conduction velocity of median, ulnar and sural nerves were 38.8 m/s, 37.9 m/s, and 34.4 m/s, respectively.
Statistical analysis: The obtained data were coded, and statistically studied by the SPSS program for Windows version 16 (SPSS Inc., USA). Parametric numerical data were stated as mean and standard deviation (SD); whereas qualitative data were stated as relative frequency (n) and percent distribution. For the correlation between two parameters, the Spearman's correlation coefficient (r) was used. P value ≤ 0.05 was considered significant for the interpretation of results. Independent samples (t) student test was used for comparison between two means for parametric variables and Mann–Whitney (U) test for non-parametric numerical variables, in adding, qualitative data were compared by Chi-square test (χ2).
Results
Forty patients with stable COPD in addition to 30 healthy subjects as a control were included in this study, the mean age of patients with stable COPD was 63.80 ± 2.13 years, whereas the mean age in the control group was 64.13 ± 1.94 years. Male subjects were 85% of the COPD group and 70% of the control group. Smoking packs/year (mean and standard deviation) in COPD group was (23.62 ± 14.50). 36 patients were smoker and 4 patients were not smoker. Arterial blood gases besides the pulmonary function test showed a statistically significant decrease of pH, PaO2, SO2, FEV1, FEV1/FVC, and FVC% in the COPD group when compared to the control group. In addition, there was a statistically significant increase of PCO2 in the COPD group when compared to the control group (59.85 ± 6.46 vs 41.40 ± 2.11, respectively) (Table 1).
Concerning the severity of COPD rendering to GOLD criteria, it was grade I in 3 cases (7.5%); Grade II in 25 cases (62.5%); grade III in 8 cases (20.0%), and grade IV in 4 cases (10.0%).
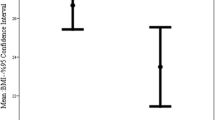
There was a statistically significant increase of distal latency and a statistically significant decrease of amplitude and conduction velocity of the median, ulnar, radial, common peroneal, and posterior tibial nerves motor assessment in the patient group when compared to the control group (Table 2).
Concerning the number of cases with affected median, ulnar and radial nerves there was a statistically significant increase of different abnormalities in the COPD group when compared to the control group denoting demyelinating more than axonal neuropathy of median nerve in COPD patients. However, when considering cases with abnormal ulnar and radial nerve changes, there was no statistically significant difference between COPD and control groups. Although demyelinating more than axonal neuropathy of ulnar and radial nerves in COPD patients (Table 3).
Considering the number of abnormal cases of the common peroneal nerve and posterior tibial nerves, there was a statistically significant increase in the COPD group when compared to the control group denoting demyelinating more than axonal neuropathy of common peroneal and posterior tibial nerves in COPD patients (Table 3).
As regards the number of cases with affected sensory median, ulnar, radial, and sural nerves there was no statistically significant difference between COPD and control groups regarding the frequency of abnormal median and ulnar nerve sensory changes but there is a statistically significant difference between COPD and control groups as regards to frequency of abnormal radial and sural sensory changes (Table 3).
The findings showed that a statistically significant increase of distal latency and a statistically significant decrease of amplitude and conduction velocity of the median, ulnar, radial, and sural nerves in the COPD group when compared to control group (Tables 4, 5).
The result of the nerve conduction study of peripheral nerves of the upper and lower limbs in the COPD group the affection of sensory fibers is more than the motor fibers and there were no differences between the affection on upper and lower limbs.
As regards the correlation between COPD severity and peripheral nerve affection, there was a statistically significant increase of nerve affection with increased severity of COPD for all studied nerves except the ulnar nerve (Table 6).
Discussion
Forty patients with stable COPD in addition to 30 healthy subjects as a control were included in this study, the mean age of patients with stable COPD was 63.80 ± 2.13 years, whereas the mean age in the control group was 64.13 ± 1.94 years. Male subjects were 85% of the COPD group and 70% of the control group. Arterial blood gases besides the pulmonary function test showed a statistically significant decrease of pH, PaO2, SO2, FEV1, FEV1/FVC, and FVC% in the COPD group when compared to the control group. In addition, there was a statistically significant increase of PCO2 in the COPD group when compared to the control group (59.85 ± 6.46 vs 41.40 ± 2.11, respectively).
The pulmonary function tests revealed a significant decrease of FEV1, FEV1/FVC, and FVC% in the COPD group when compared to the control group. These results are similar to those stated by Calik-Kutukcu et al. [11] who described that FVC, FEV1, FEV1/FVC, FEF25-75% and PEF values of patients with COPD were statistically significantly lower than those of healthy people (P = 0.001).
The assessment of COPD severity, rendering to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria was grade I (mild) in 3 patients (7.5%); grade II (moderate) in 25 patients (62.5%); grade III (severe) in 8 patients (20%) and grade IV (very severe) in 4 patients (10%). Similarly, a study by Calik-Kutukcu et al. [11] described that 5% of COPD patients had mild, 45% moderate, 30% severe, and 20% very severe concerning to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria [8],. In addition, Karthikkeyan et al. [12] described that the severity of mild, moderate type-IIA and moderate type-IIB forms of the disease were established to happen in 17, 63, and 20 percent, respectively, in the sample population.
The most important cause of peripheral nervous system involvement is hypoxemia [13] as it causes peripheral-nerve damage, harming the vasonervorum [14]. In addition, Karthikkeyan et al. [12] has described that the reason for peripheral neuropathy in patients with COPD is reduced spirometric measurements besides chronic severe hypoxemia.
Furthermore, Agrawal et al. [7] suggested that malnutrition, tobacco smoking, besides drugs used in COPD management, may be probably linked with neuropathy seen in patients with COPD.
Jindal et al. [15] Poza and Martí-Massó [16] detected a greater prevalence of peripheral neuropathy in patients with severe hypoxemia and/ or hypercapnia discovered by neurophysiological analysis. Stoebner et al. [17] reported that hypoxia is linked to nerve capillary endothelial cell hyperplasia and hypertrophy, prompting luminal occlusion that causes microangiopathy in peripheral nerves in COPD patients.
In different studies conducted by Agrawal et al. [7] and Kayacan et al. [13] have suggested the prevalence of peripheral neuropathy varied markedly from one study to another which can be explained by non-uniformity between study subjects from different studies.
Gupta et al. [18] stated that about one-third of patients with COPD have clinical confirmation of polyneuropathy, also two-thirds have abnormalities on electrophysiological studies, in addition, some patients with no clinical evidence of polyneuropathy still have electrophysiological deficit suggestive of polyneuropathy. In addition, concluded that polyneuropathy is not an uncommon systemic manifestation of COPD., Knowledge of its coexistence may be valuable in early diagnosis of polyneuropathy, thereby framing the preventive strategies and well-controlled chronic airway obstruction, keeping the PaO2 levels above the definition of hypoxemia (i.e., PaO2 > 60 mmHg) may probably help prevent or slow down the manifestations of polyneuropathy in COPD patients, and avoid another disability.
Results of the nerve conduction study showed that there was a statistically significant increase of peripheral nerve motor and sensory changes in the COPD group when compared to the control group. In addition, there was a statistically significant positive correlation between nerve affection and grades of COPD. In addition, COPD affecting sensory fibers more than motor fibers and causing axonal sensory neuropathy. These results are equivalent to those described by Kayacan et al. [13], and Ozge et al. [19], who reported that the incidence of subclinical or clinical peripheral neuropathy in COPD was 28–95%. In addition, Kazi et al. [20], stated that, 96% of the patients with COPD were having neuropathy mainly subclinical detected by nerve conduction study, as most of the patients did not have any signs and symptoms of neuropathy. In addition, the neuropathy involved was sensory nerves; mainly the sural nerve and the most common changes of neuropathy were of axonal type. They added, there was a significant association and correlation between stages of COPD (according to FEV1%) with sural NCV and amplitude.
In addition, our results co agree with those described by El-Shinnawya et al. [21], who stated that the incidence of neuropathy is high, and a statistically significant positive correlation between the severity of neuropathy and the degree of hypoxemia, while it showed a negative correlation between spirometry values (FEV1 and FEV1 /FVC ratio) and median nerve distal latency.
Demir et al. [22], noticed peripheral neuropathy in (93.5%) of the studied patients (31 subjects) on EMG the sensory nerve conduction abnormalities were the most common, the sural nerve affected in (29 subjects), the ulnar nerve (26), median nerve (28), and motor nerve conduction abnormalities; peroneal (7), median nerve (2), tibial and ulnar nerve (1). And they concluded that the frequency of neuropathy, particularly sensorial, was more than expected, with a significant positive correlation between the degree of hypoxemia and the severity of neuropathy. In addition, they advise the use of electrophysiological studies for the detection of peripheral neuropathy in patients with COPD.
Conclusions
In COPD patients the peripheral nervous system could be affected subclinically once the severity of COPD increased and the patient should be neurophysiologically observed for early recognition of peripheral nervous system affection.
Availability of data and materials
Findings on which the conclusions of the manuscript rely are summarized in the manuscript. For further inquiries, please contact the corresponding author.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- GOLD:
-
Global initiative for chronic obstructive lung disease
- MNCS:
-
Motor Nerve Conduction Study
- SNCS:
-
Sensory Nerve Conduction Study
- CMAP:
-
Compound motor action potential
- SNAP:
-
Sensory nerve action potential
References
Jiang Z, Zhu L. Update on molecular mechanisms of corticosteroid resistance in chronic obstructive pulmonary disease. Pulm Pharmacol Ther. 2016;37:1–8.
Kazi K, Mehta A, Mulla M. Electrophysiological evaluation of peripheral nerves in patients with COPD. IJBAP. 2012;1(1):83–7.
Tkác J, Man SF, Sin DD. Systemic consequences of COPD. Ther Adv Respir Dis. 2007;1:47–59.
Van Gestel AJ, Steier J. Autonomic dysfunction in patients with COPD. J Thorac Dis. 2010;2:215–22.
Doehner W, Haeusler KG, Lainscak M. Neurological and endocrinological disorders: orphans in COPD. Respir Med. 2011;105(Suppl 1):S12-19.
Kirkil G, Tug T, Muz MH. The evaluation of cognitive functions with P300 test for COPD patients in attack and stable period. Clin Neurol Neurosurg. 2007;109:553–60.
Agrawal D, Vohra R, Gupta P. Subclinical peripheral neuropathy in stable middle-aged patients with COPD. Singap Med J. 2007;48(10):887.
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 Report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–82. https://doi.org/10.1164/rccm.201701-0218PP (PMID: 28128970).
American Thoracic Society. Standard for the diagnosis and care of patients with COPD. Am J Respir Crit Care Med. 1995;152:S77-121.
Mark A, Ross MD. Polyneuropathy. In: Tan FC, editor. EMG secrets. Philadelphia (PA): Hanley and Belfus; 2004. p. 177–83 (Chapter 27).
Calik-Kutukcu E, Savci S, Saglam M. A comparison of muscle strength and endurance, exercise capacity, and fatigue in patients with COPD and healthy subjects: a cross-sectional study. BMC Pulm Med. 2014;14:6–13.
Karthikkeyan K, Padma K, Rao VB. Evaluation of visual evoked potential in patients with COPD. Indian J Physiol Pharmacol. 2015;59(2):182–8.
Kayacan O, Beder S, Karnak D. Neurophysiological changes in COPD patients with chronic respiratory insufficiency. Acta Neurol Belg. 2001;101:160–5.
Ozge A, Atis S, Sevim S. Subclinical peripheral neuropathy associated with COPD. Electromyogr Clin Neurophysiol. 2001;41:185–91.
Jindal SK, Gupta D, Aggarwal AN. WHO-Government of India Biennium (2002–2003) Programme. Guidelines for the management of chronic obstructive pulmonary disease (COPD) in India: a guide for physicians (2003). Indian J Chest Dis Allied Sci. 2004;46:137–53.
Poza JJ, Martí-Massó JF. Peripheral neuropathy associated with chronic obstructive pulmonary disease. Neurologia. 1997;12:389–94.
Stoebner P, Mezin P, Vila A, Grosse R, Kopp N, Paramelle B. Microangiopathy of endoneurial vessels in hypoxemic chronic obstructive pulmonary disease (COPD). A quantitative ultrastructural study. Acta Neuropathol. 1989;78:388–95.
Gupta N, Patil C, Gupta R, Asfahan S. Case report, peripheral neuropathy in chronic obstructive airway disease. J Med Sci. 2015;35(2):79–81.
Ozge A, Atış S, Sevim S. Subclinical peripheral neuropathy associated with chronic obstructive pulmonary disease. Electromyogr Clin Neurophysiol. 2001;41(3):185–91.
Kazi K, Mehta A, Mulla M. Electrophysiological evaluation of peripheral nerves in patients with COPD. Int J Basic Appl Physiol. 2012;1(1):83–6.
El-Shinnawya MO, Khedrb E, Metwallya M, Hassana T, Shaddada A. Peripheral neuropathy in chronic obstructive pulmonary disease. J Curr Med Res Pract. 2017;(2):17–24.
Demir R, Özel L, Özdemir G, Kocatürk I, Ulvi H. Neurophysiological changes in patients with chronic obstructive pulmonary diseases. Eur J Gen Med. 2014;11(3):153–6.
Acknowledgements
Not applicable.
Funding
No funding sources for this research had been declared (financial or non-financial). Funding was provided by the researchers.
Author information
Authors and Affiliations
Contributions
HA contributed to the research idea, methodology, data collection, analysis and data interpretations, general supervision of the research group, writing of the manuscript, drafting and revising the manuscript. AS contributed of data collection, data analysis, data interpretations, writing of the manuscript, drafting and revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local Ethics committee of Damietta faculty of medicine Al-Azhar University. Registration Number: IRB 00012367-20-05-002. Issuing: 15 May. 2020, Expiration Date: valid until 14 May 2022, Damietta faculty of medicine IRB, Al-Azhar University. Before participation in the study, the study procedure was clarified for each subject, and informed written consent was provided by each person of the participants, and was approved by the ethical committee as the study procedure don't interfere with any medical conditions and no effects on the health of participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ali, H.A.E.M., Al-Adl, A.S. Neurophysiological biomarkers of peripheral nervous system affection in patients with stable chronic obstructive pulmonary disease (COPD). Egypt J Neurol Psychiatry Neurosurg 57, 144 (2021). https://doi.org/10.1186/s41983-021-00400-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-021-00400-6