Abstract
Background
Several factors affect acute ischemic stroke (AIS) outcomes.
Objective
This study aimed to assess the role of the leukocyte count, neutrophil/lymphocyte ratio (NLR), and c reactive protein (CRP) as early predictors of outcome in AIS patients.
Methods
This study was conducted on 60 AIS patients. They were subjected to detailed history taking, clinical examination, brain imaging, and laboratory assessment including the CRP, white blood cell (WBC) count, absolute neutrophil count (ANC), absolute lymphocyte count (ALC), and NLR which is calculated by dividing ANC by ALC. Neurological scales were used to assess the level of consciousness by the Glasgow Coma Scale (GCS) and stroke severity by the National Institute of Health Stroke Scale (NIHSS) at the first 48 h of stroke onset as well as 1 week and 2 weeks later for the assessment of short-term functional neurological outcome.
Results
Sixty percent of the patients had unfavorable outcomes assessed by the Modified Rankin Scale (mRS). Patients with unfavorable outcomes had higher NIHSS scores. NLR was positively correlated with WBC count, ANC, and CRP. The higher WBC, NLR, and NIHSS, the unfavorable the outcome was.
Conclusion
The higher WBC, the NLR, and the level of CRP at the onset of AIS, the more severe stroke and the poorer the short-term outcome are expected.
Similar content being viewed by others
Introduction
Acute ischemic stroke is one of the major causes of death worldwide, and due to the high mortality and morbidity rates associated with stroke, it is becoming a major community health problem worldwide as the third of these cases are fatal and survivors usually have prolonged or irreversible disabilities [1].
Several factors affect stroke prognosis including age, stroke severity, lesion location, comorbid conditions, clinical findings, and related complications. Knowledge of the factors contributing to early neurologic deterioration after AIS can guide the early management strategies and lead to more favorable outcomes [2].
Aim
This study was designed to determine the role of the leukocyte count, NLR, and CRP in the prediction of short-term outcomes in acute ischemic stroke patients.
Methods
This is a prospective cohort study conducted on 60 AIS patients: 26 males and 34 females, with ages ranging from 45 to 95 years with a mean age of 64.8 ± 10.2 years. This study was done in intensive care and stroke units and neurology department during the period from February 2019 to February 2020.
Ethical consideration
Written informed consent was obtained from each participant or written assent from their relatives, and the ethics of research was put by the Institutional Research Board (IRB) of faculty of medicine which was followed up thoroughly.
Inclusion criteria
Patients within the first 48 h of stroke onset were diagnosed clinically and confirmed by brain imaging (computed tomography (CT) and/or magnetic resonance imaging (MRI)).
Exclusion criteria
The following were excluded: hemorrhagic stroke and other neurological causes of acute focal cerebral dysfunction such as cerebral venous sinus thrombosis, head trauma, and infection. Also, respiratory failure, liver failure, and chronic renal diseases were excluded. Patients with a history of usage of steroids or immunosuppressant drugs, cancer, autoimmune disease, myeloproliferative disorders, hematological disorders, pregnancy, and postpartum stroke were excluded.
All participants were subjected to detailed neurological history taking (with stressing on the vascular, cardiac risk factors) and full general and neurological examination. The Glasgow Coma Scale (GCS) was used to detect the depth of coma [3], and stroke severity was assessed using the National Institutes of Health Stroke Scale (NIHSS) [4], and the Modified Rankin Scale (mRS) [5] assessed the outcome.
Routine laboratory investigations were done within 48 h of stroke onset including complete blood picture (total and differential WBC, ANC, ALC, NLR), CRP, liver function test, kidney function test, erythrocyte sedimentation rate, coagulation profile, and lipid profile.
NLR is calculated by dividing ANC by ALC [6].
Brain imaging was done via CT brain (Philips) and or MRI brain (Philips) to confirm the diagnosis of recent brain infarcts.
Each participant underwent electrocardiogram, echocardiography, and carotid Doppler ultrasonography.
All patients were followed up 1 week and 2 weeks post-stroke onset using NIHSS [4] and mRs [5]. The outcome was defined as favorable if mRS equals 0–2 and unfavorable outcome if mRS >2.
Statistical analysis
All data were collected, tabulated, and statistically analyzed using the Statistical Package for the Social Science (SPSS) software version 25 [7]. Quantitative data was presented as mean, median, and interquartile range. Qualitative data was presented as frequencies and proportions. The Kolmogorov-Smirnov and Levene tests were used to determine the distribution characteristics of variables and variance homogeneity. Pearson’s chi-square (χ2) test and Fisher’s exact test were used to analyze qualitative data as appropriate. The Freidman test (F) was used to analyze dependent continuous data. The Student t test (T) and Mann-Whitney test (MW) were used to analyze continuous data between two groups as appropriate. The Kruskal-Wallis H (KW) tests were used to analyze continuous data between more than two groups. Spearman’s correlation coefficient (r) was used to test the correlation between neutrophil/lymphocyte ratio and continuous variables. The sensitivity and specificity of NLR in the prediction of unfavorable outcomes in AIS patients were also assessed by a receiver operating characteristic (ROC) curve (Fig. 1). We found a significant cutoff > 3.7 with a sensitivity of 77.85 % and a specificity of 87.5% for NLR. P value of ≤ 0.05 was accepted as statistically significant, and P value ≤ 0.001 was considered highly significant [8].
Results
The number of AIS patients who fulfilled the criteria for inclusion in the current study was sixty patients (26 male patients and 34 female patients). Their ages ranged from 45 to 95 years with a mean age of 64.8 ± 10.2 years.
The percentage of the studied patients who had unfavorable outcomes (mRS was >2) was 60% as shown in Fig. 2.
There were statistically significant differences between patients with favorable and unfavorable outcomes. Favorable outcome patients had lower WBC count, lower NLR, lower CRP, and smaller size of infarction, and patients with unfavorable outcome had moderate GCS, higher NIHSS, and presence of surrounding edema (Table 1).
There was a high statistically significant association between high NLR and unfavorable mRS (Table 2).
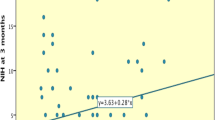
NLR was positively correlated with WBC count, ANC, and CRP. On other hand, NLR was negatively correlated with ALC (Fig. 3).
The significant risk factors for unfavorable outcomes as expressed by mRS in the studied patients were higher WBC count, higher NLR, and higher NIHSS (Table 3).
Discussion
Accurate identification of stroke outcome predictors might help ideal beginning time for immediate intervention and management. So, it is important to detect the new prognostic factors besides the already known to control them at an early stage and help in improving outcomes in ischemic stroke patients [9] (Table 4).
Identification of the relationship between short-term outcomes of ischemic stroke and inflammatory biomarkers such as WBC, NLR, and CRP might aid in supporting that anti-inflammatory therapy might be a potential treatment for AIS. So, a better understanding of immunomodulation therapy might be the balance of anti-inflammatory and proinflammatory therapies to improve outcomes in ischemic stroke patients [6].
Regarding the short-term outcomes of AIS in our study, it was found that 24 patients (40%) had favorable outcomes while 36 patients (60%) had unfavorable outcomes.
This short-term outcome was not significantly related to the mean age. And this was in agreement with the results of Castellanos et al. [10].
This contradicted the findings of Bill et al. [11], who confirmed both functional dependence and death as an independent prognostic role of increasing age. This difference might be due to the different sample size and different ages.
According to the sex of our patients, there was no statistically significant relation with short-term outcomes. This was in agreement with the results of Geng et al. [12] who showed that there was no significant difference in sex between good and poor outcomes.
We found that the outcome of the studied patients was highly significantly related to the level of consciousness assessed by GCS. Similar results were obtained by another study that showed a strong correlation between lower GCS score and patient unfavorable outcomes [13].
Higher NIHSS showed a high significant association with the patient unfavorable outcomes (P value<0.001). This finding met with the finding of another study that found that high NIHSS was an independent predictor of the short-term outcomes in patients with AIS [14].
Concerning NLR as a good predictor of short-term outcomes in the AIS patients, our study showed that 74.4% of the AIS patients with high (>3) NLR was found to have unfavorable outcomes. The median Modified Rankin Scale (mRS) of those patients was 3. There was a highly significant association between patient outcomes assessed by mRS and NLR values (P value <0.001).
These results were consistent with the findings of Tokgoz et al. [9]; also, Xue et al. [6] found that a higher NLR was associated with stroke severity at admission and short-term unfavorable outcomes.
There was a significant association between patient unfavorable outcomes and elevation of admission CRP (P value = 0.02) in our study. This finding agreed with the results of Mitchell et al. [15] who found that the levels of CRP, an acute-phase reactant, were strongly associated with stroke severity and showed that elevation in CRP levels at the time of first ischemic stroke was associated with unfavorable outcomes.
Our study showed a statistically significant positive correlation between NLR and higher admission CRP, and these results were matched with the finding of Lee et al. [16].
We found that there was a statistically significant correlation between elevated WBC count and patients’ outcomes, and this finding matched with the results of Geng et al. [12]. In our study, the elevated WBC count was statistically positively correlated with NLR values (P = 0.002). This was consistent with the results of Xue et al. [6].
Also, we found a highly significant positive association between NLR and ANC (P value <0.001), and this matched with the results of Xue et al. [6].
In our study, we found a highly significant negative association between NLR and ALC (P value <0.001), and this was consistent with the results of Kim et al. [17]. This result did not match with Kim et al. [18] who stated that lymphocytes were the sources of proinflammatory cytokines and cytotoxic substances and had a main negative contribution to ischemic brain.
The most independent factors of unfavorable outcomes of ischemic stroke in our study were higher NIHSS, higher WBC count, higher NLR, and higher CRP.
Conclusion
The higher the biomarkers (total WBCs, NLR, and the level of CRP) at the onset of AIS, the poorer the short-term outcomes are expected.
Recommendations
We recommend using inflammatory blood biomarkers such as total WBC count, NLR values, and CRP values in predicting the short-term outcomes of acute ischemic stroke patients. These are easy methods in the prediction of short-term outcomes of AIS. Further studies should be done to evaluate the impact of these biomarkers on predicting the long-term outcomes in patients with acute ischemic stroke; also, other inflammatory biomarkers can be included in future studies such as several pro-inflammatory cytokines, especially interleukin-6, d-dimer, B-natriuretic peptide, matrix metallopeptidase-9 caspase-3, sRAGE, chimerin II, and secretagogin.
Availability of data and materials
The data supporting the results of this article are included within the article.
Abbreviations
- AIS:
-
Acute ischemic stroke
- NLR:
-
Neutrophil/lymphocyte ratio
- CRP:
-
C-reactive protein
- WBC:
-
White blood cell count
- ANC:
-
Absolute neutrophil count
- ALC:
-
Absolute lymphocyte count
- GCS:
-
Glasgow Coma Scale
- NIHSS:
-
National Institute of Health Stroke Scale
- mRS:
-
Modified Rankin Scale
- IRB:
-
Institutional Research Board
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- SPSS:
-
Statistical Package for the Social Science
- MW:
-
Mann-Whitney test
- KW:
-
Kruskal-Wallis H
- ROC:
-
Receiver operating characteristic
- sRAGE:
-
Soluble receptor for advanced glycation end products
References
Adeloye D. An estimate of the incidence and prevalence of stroke in Africa: a systematic review and meta-analysis. PLoS One. 2014;9(6):100–14.
Al-Mufti F, Thabet AM, Singh T, El-Ghanem M, Amuluru K, Gandhi CD. Clinical and radiographic predictors of intracerebral hemorrhage outcome. Interv Neurol J. 2018;7(2):118–36.
Gill M, Windemuth R, Steele R, Green SM. A comparison of the Glasgow Coma Scale score to simplified alternative scores for the prediction of traumatic brain injury outcomes. Ann Emerg Med. 2005;45(1):37–42.
Fonarow GC, Saver JL, Smith EE, Broderick JP, Kleindorfer DO, Sacco RL, Pan W, Olson DM, Hernandez AF, Peterson ED, Schwamm LH. Relationship of national institutes of health stroke scale to 30-day mortality in medicare beneficiaries with acute ischemic stroke. J Am Heart Assoc. 2012;1(1):12–4.
Saposnik G, Di Legge S, Webster F, Hachinski V. Predictors of major neurologic improvement after thrombolysis in acute stroke. Neurology. 2005;65(8):1169–74.
Xue J, Huang W, Chen X, Li Q, Cai Z, Yu T, Shao B. Neutrophil-to-lymphocyte ratio is a prognostic marker in acute ischemic stroke. J Stroke Cerebrovasc Dis. 2017;26(3):650–7.
IBM. IBM SPSS Statistics for Windows, version 25. Armonk: IBM Corp; 2017.
Petrie A, Sabin C. Medical Statistics at a Glance, 3rd edn. Oxford: Wiley-Blackwell; 2009. pp. 118–121.
Tokgoz S, Kayrak M, Akpinar Z, Seyithanoğlu A, Güney F, Yürüten B. Neutrophil lymphocyte ratio as a predictor of stroke. J Stroke Cerebrovasc Dis. 2013;22(7):1169–74.
Castellanos M, Leira R, Tejada J, Gil-Peralta A, Davalos A, Castillo J. Predictors of good outcome in medium to large spontaneous supratentorial intracerebral haemorrhages. J Neurol Neurosurg Psychiatry. 2005;76(5):691–5.
Bill O, Zufferey P, Faouzi M, Michel P. Severe stroke: patient profile and predictors of favorable outcome. J Thromb Haemost. 2013;11(1):92–9.
Geng HH, Wang XW, Fu RL, Jing MJ, Huang LL, Zhang Q, Wang XX, Wang PX. The relationship between C-reactive protein level and discharge outcome in patients with acute ischemic stroke. Int J Environ Res Public Health. 2016;13(7):636.
Bakhshayesh-Eghbali B, Roudbary SA, Jafari SB, Nabizadeh SP, Naderi-Asrami N, Sohrabnejad R. Ability of serum C-reactive protein and white blood cell count in predicting acute ischemic stroke. A short-term follow-up study. Caspian J Intern Med. 2016;7(3):206–12.
Qun S, Tang Y, Sun J, Liu Z, Wu J, Zhang JI, Guo J, Xu Z, Zhang D, Chen Z, Hu F. Neutrophil-to-lymphocyte ratio predicts 3-month outcome of acute ischemic stroke. Neurotox Res. 2017;31(3):444–52.
Mitchell C, Korcarz CE, Gepner AD, Kaufman JD, Post W, Tracy R, Gassett AJ, Ma N, McClelland RL, Stein JH. Ultrasound carotid plaque features, cardiovascular disease risk factors and events: The Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2018;276:195–202.
Lee KJ, Jung KH, Byun JI, Kim JM, Roh JK. Infarct pattern and clinical outcome in acute ischemic stroke following middle cerebral artery occlusion. Cerebrovasc Dis. 2014;38(1):31–8.
Kim J, Song TJ, Park JH, Lee HS, Nam CM, Nam HS, Kim YD, Heo JH. Different prognostic value of white blood cell subtypes in patients with acute cerebral infarction. Atherosclerosis. 2012;222(2):464–7.
Kim JY, Kawabori M, Yenari MA. Innate inflammatory responses in stroke: mechanisms and potential therapeutic targets. Curr Med Chem. 2014;21(18):2076–97.
Acknowledgements
The work was carried out in the Neurology Department, Faculty of Medicine, Zagazig University. The authors acknowledge the subjects for their participation and cooperation in this study.
Funding
There is no source of funding for the research.
Author information
Authors and Affiliations
Contributions
YA, RN, PM, and AB carried out the work. YA designed the study, coordinated with the research team, and wrote the manuscript. YA and PM recruited the patients and gathered the clinical data. AB statistically analyzed and reviewed the manuscript. All authors were involved in writing the article or critically revising it for relevant intellectual material, and the final version to be published was accepted by all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional ethics committee of the Faculty of Medicine, Zagazig University (number 4973, November 2018). Written consent was taken from all of the participants after explaining the details, benefits, and risks to them.
Consent for publication
Consent for publication has been obtained from the participants involved in the study to report their individual patient data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
AlTaweel, Y.A.A.H., Nageeb, R.S., Metwally, P.M. et al. Role of some inflammatory biomarkers in prediction of short-term outcome in acute ischemic stroke. Egypt J Neurol Psychiatry Neurosurg 57, 41 (2021). https://doi.org/10.1186/s41983-021-00294-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-021-00294-4