Abstract
Background
Headache disorders are rated among the ten most disabling conditions around the world. The primary headache disorders are more common that of secondary headache. The third edition of the International Classification of Headache Disorders (ICHD-III) is considered as a helpful tool for classification and diagnosis of different headache disorders.
Methods
This is a cross-sectional study that included 500 patients who attended to the headache clinic, between May 2018 and April 2019. Arabic version of headache questionnaire was used to characterize headache, according to ICHD-III.
Results
Primary headache disorders were found in 89% (most of them is episodic in nature 76.2%), secondary headache disorders in about 10%, and painful cranial neuropathy was present in 0.8%. Primary headache associated with sexual activity was present in 1% of the total number of headache patients, and episodic cluster headache was found in 0.8%. Medication overuse headache (MOH) was the most frequent secondary headache with 2.8% of the total number of headache patients, and when overlaps with chronic migraine or chronic tension type of headache (TTH), the percent was 12.8% and 8.8% respectively. Male to female ratio was 1:3, 3:5, and 1:1 in primary headache, secondary headache, and painful cranial neuropathy respectively. Simple analgesia was the most common abortive therapy (44.8%) while the antidepressants were the most common preventive treatment (17%).
Conclusion
This study estimates the frequency and characterizes different headache disorders, according to ICHD-III in an outpatient headache clinic at Sohag Governorate, Egypt.
Similar content being viewed by others
Introduction
Headache disorders are rated among the ten most incapacitating conditions worldwide with a global prevalence of 47% [1, 2], and it may cause a significant social and economic burden [3]. The headache can be classified to primary headache disorders which include migraine, tension-type headache (TTH), and cluster headache, and less common secondary type of headache which may be due to intracranial neoplasms, epileptic seizures, or intracranial infections [4, 5]. A recent meta-analysis indicates that migraine is highly prevalent worldwide, with a prevalence to be 11.6% on the community level [6]. In a study conducted with participants from Eastern Mediterranean Region (EMR), Vosoughi and colleagues [7] emphasized the fact that primary headache disorders are a large cause of disability in this region and highlighted the priority of management and preventive measures to decrease the burden of headache in this region [7]. In Egypt, a population-based study conducted in Fayoum Governorate revealed that the 1-year headache prevalence was 51.4%, and the most common primary headache subtype was episodic tension type headache (24.5%), followed by episodic migraine (17.3%) [8]. Similarly, a study conducted in Saudi Arabia revealed that tension headache was also the commonest primary headache with a prevalence of 9.5% then migraine with prevalence 5.0% [9]. In addition to a study conducted in Qatar and based on face-to-face questionnaire, it was reported that migraine was present in 7.9% [10]. So, the results of epidemiological studies of headache disorders are still inconsistent, particularly in Arab countries in spite of its significant burden and disability.
Worldwide estimate of secondary headache is 18% of headache patients [11] with 1-year prevalence of 2.1% in a population-based study [5] and 12.9% of headache patients when the epidemiological studies conducted in tertiary centers [12]. After publication of ICHD-III in 2018, it was widely accepted for classification and diagnosis of headache disorders [13]. In developing countries particularly Egypt, headache is still poorly managed because of several reasons, including insufficient patient education, over-the-counter self-medications, and improper understanding of impact of headache on patient’s quality of life [8, 14]. The aim of this hospital-based cross-sectional study is to investigate the frequency and characteristics of different types of headache in the light of recent headache classification namely ICHD-III.
Methods
Participants in this cross-sectional study were recruited from the outpatient headache clinic, between May 2018 and April 2019. The hospital is a tertiary center serving a wide geographical area. Sohag is one of the governorates of Egypt. It is located in the southern part of the country (Upper Egypt) and covers a stretch of the Nile Valley. According to population estimates, in 2015, the majority of residents in the governorate lived in rural areas, with an urbanization rate of only 21.4%. Of the approximately 4,603,861 residents in the governorate in 2015, 3,628,543 lived in rural areas and 985,318 in urban areas [15].
The sample [n = 500, 131 males (26.2%) and 369 females (73.8%)] consisted of patients complaining of headache. Each patient was subjected to full medical and neurological evaluation including history of precipitating factors for each headache attack, comorbid medical conditions, and educational level based on the International Standard Classification of Education (ISCED) [16].
We used the Arabic version of headache questionnaire [17] which was completed by patients, and those who are illiterate were helped by a neurologist in the outpatient headache clinic. This questionnaire is composed of two parts: the first part included demographic, personal, and medical aspects (age, gender, education, marital status, occupation, and place of living, contraceptive pill uses, smoking, hypertension, and other relevant medical disorders). The second part of the questionnaire included questions designed to define the nature and assess patterns of the headache including onset, duration, frequency, site, side—unilateral/bilateral, associated symptoms, and precipitating factors. Each type of headache was diagnosed according to most updated criteria of the ICHD-III [13] and classified into 14 different subgroups. Subgroups 1 to 4 were primary headaches, including migraine, TTH, trigeminal autonomic cephalgias (TACs), and the other primary headache. TACs are subdivided into cluster headache, paroxysmal hemicrania, and short-lasting unilateral neuralgiform headache attacks which include [short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) and short-lasting unilateral neuralgiform headache attacks with cranial autonomic symptoms (SUNA)]
Subgroups 5 to 12 were secondary headaches which are consequences of head and/or neck trauma; cranial or cervical vascular disorder; non-vascular intracranial disorder; substance or its withdrawal; infection; disorders of hemostasis; disorders of facial structures (disorders of the eyes, ears, nose, or paranasal structures), cranial structures (cranial bone, jaw disorders), or cervical structures (cervicogenic headache); and lastly psychiatric disorders. Brain computed tomography scan (Siemens Somatom Emotion, 16-CT scanner, Germany) and/or magnetic resonance imaging (Siemens MRI Essenza Machine, 1.5 Tesla, Germany) was done for patients with suspected intracranial lesions.
Subgroup 13 corresponds to painful cranial neuropathies and other facial pain. If the headache could not be accurately categorized as either primary or secondary, it was classified as subgroup 14 (unspecified or not elsewhere classified headaches). Patients with unclassified headache disorders were excluded from the study to accurately estimate the percentage of primary and secondary headache disorders. Patients who reported headaches at a frequency of more than 15 days/month over a period of 3 months were classified as chronic headache which include chronic migraine (CM), chronic tension-type headache (CTTH), medication overuse headache (MOH), new daily persistent headache (NDPH), chronic paroxysmal hemicrania, SUNA, or hemicrania continua (HC). Participants who reported headache ≥ 15 days/month with regular overuse for > 3 months of one or more acute/symptomatic treatment drugs were diagnosed to have MOH. The term probable in a specific headache category means headache is not fulfilling all the criteria in this category for example ICHD-III, coded probable migraine without aura when the participant has had fewer than five attacks of headache [13]. The study was approved by the Ethical Committee on Research Involving Human Subjects at the University of Sohag on March 2018, and informed written consent was taken from each patient before the study.
The statistical analysis was performed using the Statistical Package for the Social Sciences for Windows (SPSS 20.0, IBM Corp., Armonk, NY, USA). Simple descriptive analysis in the form of means and standard deviations was calculated from numerical data. The prevalence was expressed in percentage. Non-parametric tests (chi-square) were used to find its association with other factors. The Student t test was used to compare the continuous variables. A two-way between-groups analysis of variance was conducted to explore the impact of sex and age on different headache disorders with post hoc comparisons using the Tukey test. P ≤ 0.05 was considered statistically significant.
Results
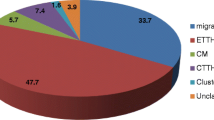
A sum of 500 headache patients was enrolled in this study and classified according to ICHD-III (Figs. 1 and 2). The participants’ age ranged from 11 to 78 years with a mean age of 34.8 ± 13 years. The urban residency was 58.2%, while rural residency was found in 41.8% (Table 1). The socio-demographic characteristics of the participants and precipitating factors of headache are shown in Table 1.
Primary headache (groups 1 to 4 of ICHD-III) was present in 89% of total participants, secondary headaches (groups 5 to 12) were present in 10.2%, and painful cranial neuropathies (group 13) were present only in 0.8% (Table 2).
Because of the availability, simple analgesia was the most common abortive therapy (44.8%) while the antidepressants were most commonly used as preventive treatment (17%) in headache disorders as they are used in both migraine and TTH (Table 2).
Among primary headache, migraine was the most prevalent subtype (50.6%), then TTH (33.6%), and lastly painful cranial neuropathy (0.8%) (Table 3).
Sixty six percent of the total migraine participants have fulfilled the criteria for migraine without aura (including probable migraine without aura) while migraine with aura and chronic migraine were present in 13.8% and 19.7% respectively (Table 3).
The frequency of different headache subtypes in males and females is shown in Table 3.
Male to female ratio was 1:3, 3:5, and 1:1 in primary headache, secondary headache, and painful cranial neuropathy respectively (Table 3).
Gender and age distribution in different headache subtypes is shown in Table 3.
Episodic and chronic headache was present in 76.2% and 23.8% respectively of the participants (Table 3). The percent of chronic headache in males was 30.5% while in females was 21.4% with P value 0.03.
Most of the patients with MOH have chronic migraine and chronic TTH with 12.8% and 8.8% respectively (Table 3).
Discussion
The prevalence of headache disorders, including migraine, tension-type headache, and MOH, is high [18]. In population-based studies, migraine was found in 9.6 to 24.6%, and 1-year prevalence of TTH is in a wide range between 15 and 90%. In an Egyptian study conducted in Fayoum Governorate, the observed 1-year prevalence of migraine and episodic TTH was 17.3 and 24.5% respectively [8]. In our series, we found that primary headache was present in 89%, while secondary headache in 10.2% and painful cranial neuropathy in 0.8%, and these results are in line with Guerrero and colleagues [19] who reported that primary headaches was present in 77.1% and secondary headaches in 10.9%. Among the total headache participants, we found that the percent of migraine and TTH was 50.6% and 33.6% respectively. The percent of other primary headache and TACs was 2.6% and 2.2% respectively. These results are consistent with those obtained from previous studies [20,21,22,23,24].
Pedraza and colleagues [25] reported that primary headache was present in 72% and secondary headache in 12%, and among the primary headache group, migraine was present in 53%, TTH in 10.5%, TACs in 2.5%, and other types of primary headache were present in 5.9%, and they explained the low rate of TTH in their series by the lower impact of TTH on the patients, and few patients seek medical consultation for their headaches [25].
In a Hungarian study conducted on 327 patients, primary headache migraine was found in 42%, TTH in 31%, cluster headache in 1%, and 26% had a combination headache [22]. Many previous studies documented that migraine is the most frequently assigned diagnosis in specialist clinics or headache units [12, 25,26,27,28].
Although some previous studies reported that TTH is the most common type of primary headache all over the world [1], migraine was the most common presentation in our series, and this may be explained by the under-recognition of TTH by patients and health practitioners for its less disability than migraine.
In contrast, a Turkish study was conducted in 245 of headache patients and revealed that TTH was present in 70% and migraine only in 44.9%, [29] and this difference may be explained by a relatively small number of patients and different methodology as they used the ICHD-II criteria.
We reported that only 2.2% of total patients corresponds to TACs which is in line with the results obtained by Guerrero and colleagues [19] who reported that TACs were present in 2.6% of the patients and lower than that obtained by Dong and colleagues [12] who reported 5.3% of total patients were classified into TAC which may be explained by regional and racial reasons.
In our series, we found only 0.8% of the participants corresponds to painful cranial neuropathy namely trigeminal neuralgia, which is low frequency in comparison to Pedraza and colleagues [25] who reported that about 4% of the patients’ headaches corresponded to cranial neuralgias while Felício and colleagues [27] reported that 2.6% of the participants suffer from cranial neuralgias. This difference may be explained by the painful cranial neuralgias particularly trigeminal neuralgia (TN) which is a relatively rare condition with a lifetime prevalence of up to 0.3% [30], and most patients with TN consulted their dentist first.
As in previous studies [12, 19, 31], we found a low frequency (10.2%) of secondary headache. Among the patients with secondary headache, we found that the percent of MOH was 5.3% of total headache participants and 27.5% of the patients with secondary headache, a finding confirmed by previous studies [25, 32]. However, other studies reported higher frequency of secondary headaches ranging from 22.1 to 42% in which participants were selected from the emergency departments [33,34,35,36] because most of the emergency room (ER) doctors recognize headache as a disease with underlying somatic reasons, and some racial, regional, selection bias may contribute to these differences.
In this work, we found that headache attributed to cranial and/or cervical vascular disorder (group 6 of ICHD-III) which had been rarely observed (1.4%), and this may be due to the patients with cerebrovascular events, mostly coming to the emergency room (ER), and headache as a symptom may not attract the attention of the ER doctors.
We found women’s dominance in primary headache, particularly migraine because of the well-established hormone influence in migraine [37]. The percent of female participants was 73.8% of the total number of the patients with male to female ratio of 1:2.3 which is in line with worldwide prevalence data from the 2015 Global Burden of Disease Study [38] showing that migraine is two to three times more prevalent in women than in men. Okumura and colleagues [34] reported that migraine about 3 times higher rate was observed in female than in male patients.
In the current study, we found that male to female ratio for TTH is 1:5 which indicates that women are more prone to TTH than in men, and this is in line with the previous studies that have reported that tension-type headache is more frequently seen in women with male to female ratio of 1:6 [39,40,41]. In contrast to El-Sherbiny and colleagues [8] who reported that male to female ratio for TTH was 2:3, Stovner and colleagues [42] observed that male to female ratio for TTH was 4:5 which is lower than our results as most of our series are females (73.8%) who consists about three fourths of the total number of the participants, and women are more likely to seek medical advice.
We found that episodic migraine was found in 40.6% of the total number of headache patients, chronic migraine in 10%, episodic TTH in 29.2% of the total number of headache participants, chronic TTH in 4.4%, and episodic cluster headache in 0.8% of the total number of headache participants, and this in agreement with previous study which reported that episodic migraine was present in 35.3%, chronic migraine in 3.9%, episodic TTH in 45.3%, chronic TTH in 5.6%, and cluster headache in 3.4% [8]. Like previous studies [8, 43], we also found that primary headache disorders, especially, migraine is more common in urban areas.
This study is a cross-sectional study and not a population-based survey; moreover, patients with unclassified headache disorders (group 14) were excluded from this study; therefore, the data cannot be used to accurately estimate the prevalence of primary headaches, and epidemiological studies will be needed. Our data based on clinical background including Arabic version of headache questionnaire and brain imaging studies were not routinely done for all patients, and finally, we did not do any anxiety or depression scale for patients with TTH to investigate the underlying anxiety or depression. In spite of these limitations, the present study has shown the frequency and characteristics of different headache disorders according to ICHD-III.
Conclusion
This study is among the few studies that characterize the headache patients by using the Arabic version of headache questionnaire according to the third edition of ICHD-III in Sohag Governorate, Egypt.
Availability of data and materials
The data set of this work is available.
Abbreviations
- ASDH:
-
Acute subdural hematoma
- CM:
-
Chronic migraine
- CT:
-
Computed tomography scan
- CTTH:
-
Chronic tension-type headache
- CVT:
-
Cerebral venous thrombosis
- EMR:
-
Eastern Mediterranean Region
- ER:
-
Emergency room
- GCA:
-
Giant cell arteritis
- ICHD-III:
-
The third edition of the International Classification of Headache Disorders
- IIH:
-
Idiopathic intracranial hypertension
- ISCED:
-
The International Standard Classification of Education
- MOH:
-
Medication overuse headache
- MRI:
-
Magnetic resonance imaging
- NDPH:
-
New daily persistent headache
- PT:
-
Pericranial tenderness
- SPSS:
-
Statistical Package for the Social Sciences for window
- SUNA:
-
Chronic short-lasting unilateral neuralgiform headache attacks with cranial autonomic symptoms
- SUNCT:
-
Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing
- TACs:
-
Trigeminal autonomic cephalgias
- TIA:
-
Transient ischemic attack
- TN:
-
Trigeminal neuralgia
- TTH:
-
Tension type of headache
References
Stovner L, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210.
Steiner TJ, Birbeck GL, Jensen RH, Katsarava Z, Stovner LJ, Martelletti P. Headache disorders are third cause of disability worldwide. J Headache Pain. 2015;16:58.
Selekler HM, Gökmen G, Alvur TM, Steiner TJ. Productivity losses attributable to headache, and their attempted recovery, in a heavy-manufacturing workforce in Turkey: implications for employers and politicians. J Headache Pain. 2015;16(1):96.
Grande RB, Aaseth K, Gulbrandsen P, Lundqvist C, Russell MB. Prevalence of primary chronic headache in a population-based sample of 30-to 44-year-old persons. Neuroepidemiology. 2008;30(2):76–83.
Aaseth K, Grande R, Kvárner K, Gulbrandsen P, Lundqvist C, Russell M. Prevalence of secondary chronic headaches in a population-based sample of 30-44-year-old persons. The Akershus study of chronic headache. Cephalalgia. 2008;28(7):705–13.
Woldeamanuel YW, Cowan RP. Migraine affects 1 in 10 people worldwide featuring recent rise: a systematic review and meta-analysis of community-based studies involving 6 million participants. J Neurol Sci. 2017;372:307–15.
Vosoughi K, Stovner LJ, Steiner TJ, Moradi-Lakeh M, Fereshtehnejad S-M, Farzadfar F, et al. The burden of headache disorders in the Eastern Mediterranean Region, 1990-2016: findings from the Global Burden of Disease study 2016. J Headache Pain. 2019;20(1):40.
El-Sherbiny NA, Masoud M, Shalaby NM, Shehata HS. Prevalence of primary headache disorders in Fayoum Governorate, Egypt. J Headache Pain. 2015;16(1):85.
Rajeh SA, Awada A, Bademosi O, Ogunniyi A. The prevalence of migraine and tension headache in Saudi Arabia: a community-based study. Eur J Neurol. 1997;4(5):502–6.
Bener A. Frequency of headache and migraine in Qatar. Neuroepidemiology. 2006;27(2):61–6.
Organization WH. Atlas of headache disorders and resources in the world 2011. Geneva: World Health Organisation; 2011.
Dong Z, Di H, Dai W, Liang J, Pan M, Zhang M, et al. Application of ICHD-II criteria in a headache clinic of China. PLoS One. 2012;7(12):e50898.
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1–211.
Kandil M, Hamed S, Fadel K, Youssef A, Abd El Hamed M, KJJNN M. Epidemiology of tension-type headache (TTH) in Assuit Governorate, Egypt. J Neurol Neurosci. 2014;5(1):2.
CAPMAS - Central Agency for mobilization and Statistics. Egypt in Figures 2015. CAPMAS. 2015. from: https://article.wn.com/view/2015/03/02/Egypt_in_Figures_2015_CAPMAS_Central_Agency_for_mobilization/.
Schneider SL. The international standard classification of education 2011. Class Stratif Anal. 2013:365–79.
El-Sherbiny NA, Shehata HS, Amer H, Elmazny A, Masoud M, Helmy H, et al. Development and validation of an Arabic-language headache questionnaire for population-based surveys. J Pain Res. 2017;10:1289.
Saylor D, Steiner TJ. The global burden of headache. Semin Neurol. 2018;38(2):182–90.
Guerrero ÁL, Rojo E, Herrero S, Neri MJ, Bautista L, Peñas ML, et al. Characteristics of the first 1000 headaches in an outpatient headache clinic registry. Headache. 2011;51(2):226–31.
Wang SJ, Chung CS, Chankrachang S, Ravishankar K, Merican JS, Salazar G, et al. Migraine disability awareness campaign in Asia: migraine assessment for prophylaxis. Headache. 2008;48(9):1356–65.
Wang Y, Zhou J, Fan X, Li X, Ran L, Tan G, et al. Classification and clinical features of headache patients: an outpatient clinic study from China. J Headache Pain. 2011;12(5):561–7.
Gesztelyi G, Bereczki D. Primary headaches in an outpatient neurology headache clinic in East Hungary. Eur J Neurol. 2004;11(6):389–95.
Murtaza M, Kisat M, Daniel H, Sonawalla AB. Classification and clinical features of headache disorders in Pakistan: a retrospective review of clinical data. PLoS One. 2009;4(6):e5827.
Goldstein J, Camargo C Jr, Pelletier A, Edlow J. Headache in United States emergency departments: demographics, work-up and frequency of pathological diagnoses. Cephalalgia. 2006;26(6):684–90.
Pedraza M, Mulero P, Ruíz M, de la Cruz C, Herrero S, Guerrero A. Characteristics of the first 2000 patients registered in a specialist headache clinic. Neurología (English Edition). 2015;30(4):208–13.
Silva AA, Jr., Tavares RM, Lara RP, Faleiros BE, Gomez RS, Teixeira AL. Frequency of types of headache in the tertiary care center of the Hospital das Clínicas of the Universidade Federal de Minas Gerais, MG, Brazil. Revista da Associacao Medica Brasileira (1992). 2012;58(6):709–13.
Felício AC, Bichuetti DB, WACd S, CdO GJ, Marin LF, DdS C. Epidemiology of primary and secondary headaches in a Brazilian tertiary-care center. Arquivos Neuro-Psiquiatria. 2006;64(1):41–4.
Dowson AJ. Analysis of the patients attending a specialist UK headache clinic over a 3-year period. Headache. 2003;43(1):14–8.
Tuğba T, Serap Ü, Esra O, Özlem C, Ufuk E. Features of stabbing, cough, exertional and sexual headaches in a Turkish population of headache patients. J Clin Neurosci. 2008;15(7):774-7.
Mueller D, Obermann M, Yoon MS, Poitz F, Hansen N, Slomke MA, et al. Prevalence of trigeminal neuralgia and persistent idiopathic facial pain: a population-based study. Cephalalgia. 2011;31(15):1542–8.
Manzoni GC, Stovner LJ. Epidemiology of headache. Handb Clin Neurol. 2010;97:3–22.
Pascual J, Mateos V, Gracia M, Láinez J. Medication overuse headache in Spain. Cephalalgia. 2008;28(11):1234–6.
Dermitzakis EV, Georgiadis G, Rudolf J, Nikiforidou D, Kyriakidis P, Gravas I, et al. Headache patients in the emergency department of a Greek tertiary care hospital. J Headache Pain. 2010;11(2):123.
Okumura T, Tanno S, Ohhira M, Tanno S, Nozu T. Characteristics in patients with headache in an outpatient clinic in Japan. Asia Pac Fam Med. 2010;9(1):10.
Relja G, Granato A, Capozzoli F, Maggiore C, Catalan M, Pizzolato G, et al. Nontraumatic headache in the emergency department: a survey in the province of Trieste. J Headache Pain. 2005;6(4):298–300.
Friedman BW, Hochberg ML, Esses D, Grosberg B, Corbo J, Toosi B, et al. Applying the International Classification of Headache Disorders to the emergency department: an assessment of reproducibility and the frequency with which a unique diagnosis can be assigned to every acute headache presentation. Ann Emerg Med. 2007;49(4):409-419, 19.e1-9.
Bolay H, Ozge A, Saginc P, Orekici G, Uludüz D, Yalın O, et al. Gender influences headache characteristics with increasing age in migraine patients. Cephalalgia. 2015;35(9):792–800.
Steiner TJ, Stovner LJ, Vos T. GBD 2015: migraine is the third cause of disability in under 50s. J Headache Pain. 2016;17(1):104.
Group THES. An epidemiologic study of headache in Turkey: a nationwide survey. Neurology. 1998;50(4):225.
Chen T, Leviton A, Edelstein S, Ellenberg J. Migraine and other diseases in women of reproductive age: the influence of smoking on observed associations. Arch Neurol. 1987;44(10):1024–8.
Bayraktutan OF, Demir R, Ozel L, Ozdemir G, Ertekin A. Prevalence of tension-type headache in individuals aged between 18-65 years in the eastern parts of Turkey. Eurasian J Med. 2014;46(2):78–83.
Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):954–76.
Rho YI, Chung HJ, Lee KH, Eun BL, Eun SH, Nam SO, et al. Prevalence and clinical characteristics of primary headaches among school children in South Korea: a nationwide survey. Headache. 2012;52(4):592–9.
Acknowledgements
Not applicable
Funding
None
Author information
Authors and Affiliations
Contributions
AAB, as a single author, is solely responsible to the design and implementation of the research, to the analysis of the results, and to the writing and reviewing of the manuscript. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by local ethical committee in Faculty of Medicine, Sohag University, in March 2018. (The committee’s reference number is not available.)
Informed written consent was obtained from all patients for participation and publication of this study.
Consent for publication
Not applicable
Competing interests
There were no financial or non-financial conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohamed, AA.B. Characteristics of headache disorders, according to ICHD-III in an outpatient headache clinic in Sohag Governorate, Egypt. Egypt J Neurol Psychiatry Neurosurg 57, 16 (2021). https://doi.org/10.1186/s41983-021-00271-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-021-00271-x