Abstract
Background
Cognitive impairment is an important aspect for stroke survivors. Little data are available about the frequency and risk factors of post-stroke dementia in Egypt.
Objectives
The aim of this study is to evaluate the frequency and predictors of post-stroke dementia and its impact on outcome.
Methods
A total of 380 patients with acute stroke were included. Patients were subjected to demographic data collection, neurological examination, and assessment of vascular risk factors. Furthermore, assessment of stroke severity by Barthel Index was done. After 6 months, patients were assessed for outcome and development of post-stroke dementia.
Results
Post-stroke dementia was detected in 20.8% of patient. It was recorded more in old ages, illiterates, unmarried, unemployed, and those with recurrent stroke and with cerebral infarction (significantly with cardio-embolic).
Conclusion
Post-stroke dementia is high in Egypt, especially in those with illiteracy, atrial fibrillation, brain atrophy, severe strokes, and those presented with hemiplegia, sphincter affection, abnormal gait, and psychotic features. Assessment for post-stroke dementia should be done during follow up of stroke patients.
Similar content being viewed by others
Introduction
Cerebrovascular stroke (CVS) is one of the leading causes of mortality and disability worldwide [1]. Many patients are left with residual cognitive deficits [2, 3]. Post-stroke dementia (PSD) is the second most common cause of dementia [4] and one of the main causes of dependency in survivors [5]. About one-third of stroke survivors are found to have a significant degree of cognitive impairment within the first months after the event [6].
The prevalence of PSD in stroke survivors is about 30% and having a stroke doubles the risk of dementia [7]. The risk factors for PSD are multifactorial and include genetic predisposition, demographic factors such as old age and low education, pre-stroke cognitive and functional status, number of prior transient ischemic attacks or strokes, and vascular risk factors of stroke [8].
The mechanism of PSD remains unclear and its pathological substrates are poorly understood, but the most accepted theory is that the heterogeneous nature of vascular lesions of stroke may have an effect on cognition through altered blood and oxygen supply to brain tissues, chronic inflammation, disruption of axonal tracts, or altered cortical connectivity [9]. Moreover, medical comorbidities such as hypertension and diabetes mellitus can cause cerebral hypoxia or ischemia leading to cerebral hypoperfusion, which serves as a basis for PSD [7].
In a study in NY, USA, dementia diagnosed 3 months after stroke was associated with triple increase in the risk of stroke recurrence and might be a surrogate marker for more severe vascular disease leading to lack of compliance that can contribute to worse outcome [10]. Several studies have shown that PSD was independently associated with increased post-stroke mortality, after adjusting for vascular risk factors and stroke severity [11, 12].
To the best of our knowledge, data about the frequency and risk factors of PSD is still deficient in Egypt and we hypothesize that the frequency and risk factors of PSD varied among different populations due to different genetic and environmental factors. So, this article aimed to discuss the frequency, risk factors, and impacts of PSD on outcome, and consequently recommended early and optimal intervention in the window before dementia sets in for proper health plan.
Methods
The current work was a prospective cohort study. Three hundred eighty patients with acute cerebrovascular stroke (within 1 week) were recruited from stroke unit and neurology ward, and followed up at outpatient clinics of Assiut and Aswan University Hospitals from September 2017 to August 2019 and included in this study.
Patients with transient ischemic attack, brain lesions other than stroke such as brain tumors, with unreliable informant, refuse to participate, known to have serious renal, hepatic dysfunction. Patients with known psychiatric disease, or have mild cognitive impairment and other types of dementia from the history (diagnosed according to DSM-V), inability to communicate such as sensory aphasia and those receiving medications that affect cognition such as antipsychotics and antidepressants were excluded from the study.
To confirm the diagnosis of stroke, all patients underwent CT and /or MRI brain. Patients were classified according to their clinical picture and neuroimaging into ischemic and haemorrhagic stroke (cerebral and subarachnoid hemorrhage) with localization of cerebral lesions.
Data on self or family reported risk factors for stroke, including socio-demographics, hypertension, diabetes mellitus, heart diseases, smoking, family history, and number of recurrence of stroke, were obtained from the patient/or his caregivers. At time of admission, all patients were subjected to meticulous neurological and general examination. Assessment of lipid profile was performed to all patients, where hypercholesterolemia and hypertriglyceridemia were considered when serum levels > 239 mg/dl and > 200 mg/dl respectively [13]. Electrocardiography (ECG) and/or echocardiography were performed to determine any arrhythmias and/or any ischemia (CON-TEC, model: ECG100G, China).
Assessment of patients by Barthel Index (BI) [14] was done at the onset of stroke and 6 months later. The severity of all strokes was determined, where there were three grades; very poor: complete dependence (BI score < 60), poor: assisted independence (BI score 60–< 95), and excellent: minimal or no disability (BI score ≥ 95). Stroke was considered severe when the patient had poor or very poor grade on BI.
Within 6 months from onset, all patients were evaluated for the development of PSD. The diagnosis of dementia was made according to Hachinski Ischemic Score [15] and the criteria of vascular dementia in the DSM-V [16]. Mini-Mental State Examination (MMSE) was performed to detect dementia and its grades, where patients with scores 19 ≤ 23 (17 ≤ 21 for illiterates) were diagnosed to have mild dementia, 10 < 19 (9 < 17for illiterates) have moderate, and < 10 (< 9 for illiterates) to have severe dementia [17]. The outcome of all CVS patients was assessed clinically and by BI by the end of the 6 months.
Sample size calculation was carried out using G*Power 3 software [18]. A calculated minimum sample of 154 stroke patients divided into two groups (77 with PSD and 77 without PSD) were needed to detect an effect size of 0.1 in the mean GCS, MMSE, and BI, with an error probability of 0.05 and 90% power on a two-tailed test. The sample was raised to include 79 with and 301 without PSD.
Data were processed by the researchers and analyzed using IBM-SPSS 21.0 (IBM-SPSS Inc., Chicago, IL, USA) [19]. Descriptive statistics: means, standard deviations, and percentages were calculated. Test of significances: chi-square test was used to compare the difference in distribution of frequencies among different groups. Independent t test analysis was carried out to compare the means of dichotomous data. Significant variables from the univariate analysis were entered in multivariable logistic regression model to test the independent predictors of dementia in patients with stroke using odds ratio (OR), 95% confidence interval (CI), and p value. A significant p value was considered when it is equal or less than 0.05.
Results
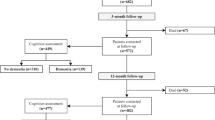
A total number of 432 stroke patients were assessed for eligibility criteria. Twenty-two of them were excluded because they did not met the inclusion criteria, while thirty patients dropped out during the follow up (Fig. 1). Among the 380 stroke patients included and completed the current study, 20.8% developed dementia.
The mean PSD patients’ age was 71.6 ± 9.8 years. PSD was detected in 19.8% and 22% of male and female patients, respectively. Also, it was detected in about one-quarter (24.3%) and one-fifth (19.5%) of rural and urban inhabitant patients, respectively. Furthermore, PSD was recorded in about three-quarters (76%) and four-fifth (81%) of illiterate and non-working patients, respectively (Table 1).
Vascular risk factors such as hypertension, diabetes mellitus, and dyslipidaemias had statistically insignificant effect on PSD (P > 0.05). On the other hand, AF was reported among 21.5% of PSD versus 2.7% of patients without PSD with statistically significant difference (P < 0.001). Moreover, PSD was recorded more in patients with recurrent stroke (Table 2).
Table 3 demonstrated that PSD developed significantly more in patients with severe initial stroke, and in those with certain clinical and neuroimaging presentations (≤ 0.01). In addition, it developed more significantly in patients with cerebral infarction (P = 0.044), especially in those with cardio-embolic strokes (P < 0.001). Assessment of the degree of PSD according to MMSE scores revealed that 27.8% of cases of PSD were mild, 63.3% were moderate, and only 8.9% had severe dementia (Fig. 2).
After adjusting for age and sex, the final multivariate model contained eight independent predictors, illiteracy, AF, brain atrophy, poor prognosis, hemiplegia, sphincteric affection, abnormal gait, and psychotic features at onset. In other words, illiterate patients and those with AF were 1.6 and 6.1 times more at risk of having PSD [AOR = 1.60 and 6.11, P = 0.041 and 0.005, respectively] (Table 4).
Figure 3 showed the patient’s improvement. According to clinical evaluation, the majority of patients with PSD (98.7%) either did not improve or deteriorated compared to 36.5% of those without dementia (P < 0.001). Likewise, about three-quarters (77.2%) of patients with PSD had poor/very poor outcome as compared to less than half (45.5%) of patients without dementia, according to BI (P < 0.001).
Discussion
Prevalence of PSD has been found to be higher than previously expected, its course is non-linear, being higher in the first 6 months after stroke, and it is reported to be between 6 and 32%. This wide range may be due to methodological differences [20]. In our hospital-based study, the frequency of PSD was 20.8%, which was comparable to previous studies; (19.3%) in America, (23.2%) in Iran, and (24.6%) in Italy [21, 22].
The prevalence of our PSD was significantly higher in unmarried, non-working, old aged, and illiterate subjects, likewise other studies that proved non marriage [23, 24], unemployment [25], advanced age [26, 27], and low education [28,29,30,31,32,33] were the major determinants of PSD. The cognitive reserve hypothesis postulated that a higher level of education is a protective against dementia, where it increases neuronal plasticity and connectivity [34].
Also, likewise other studies [28, 35, 36], we reported that the prevalence of PSD was more frequent in rural than urban inhabitants, but the difference was insignificant (P = 0.234). This could be explained by the protective role of education, where in our country urban inhabitants have higher concern with education more than rural.
Although, most studies [37,38,39] concluded that the risk of PSD did not depend on gender and likewise other studies [40,41,42], our results detected PSD among female more than male patients but the difference was insignificant (P = 0.344). This high prevalence may be explained by hormonal changes, lifestyles, and low level of education among females, and it supported the hypothesis that gender has an important role in development and organization of brain function [43].
The present study demonstrated that AF is an important predictor of cognitive outcome after stroke. A cohort study on AF diagnosed after stroke, published by Michal and colleagues, 2019 [44] showed that AF diagnosed after stroke increased the incident dementia, and patients on anticoagulant have a lower risk to develop dementia. The high incidence of PSD in patients with AF may be explained by the high frequency of subclinical micro infarcts and recurrent stroke, in addition to the severity of stroke in patients with AF. Furthermore, patients with AF may have atrial cardiomyopathy, endothelial dysfunction and fibrosis, and atrial hypercoagulability, which may act as a source of embolization [45].
The results of our study like previous studies [46,47,48] had shown that diabetes mellitus was associated with an increased risk of PSD; this may be attributed to the high prevalence of atherosclerosis and arteriosclerosis in diabetics, impaired cerebral autoregulation, and increased blood viscosity. On the other hand, the other vascular risk profiles, other than diabetes, indirectly affect PSD through cerebral infarcts and white matter changes.
In the current study, recurrent or severe stroke, multi-infarcts or small vessel disease in neuroimaging, and sphincter disturbance were associated with increased risks of PSD. This may be attributed to intracerebral circuit interruption or functional cortical disconnection, in addition to the effect of inflammatory mediators of the vascular insult or the systemic complications. A recent study by Pendlebury and Rothwell [48] mentioned that long-term risk of dementia can be reduced by appropriate stroke car.
Although, previous studies [38,39,40] stated that the risk of PSD and its severity were not influenced by the type of stroke (ischemic or haemorrhagic), our study demonstrated PSD more significantly among ischemic than hemorrhagic stroke patients (P = 0.044). This could be explained by the fact that cerebral infarction causes more wide spread massive damage to brain parenchyma and its occurrence in relatively old age with impaired vascular supply increases the probability of dementia.
Our results showed that stroke survivors who presented by focal neurological manifestations such as hemiplegia, dysarthria, affected sphincters, gait disorder, extrapyramidal signs, or psychotic manifestations had a significantly higher risk of PSD. This may be attributed to the site of the lesion, and decreased physical activity.
In the current study, PSD was found to be associated with psychotic symptoms. The relationship between psychotic manifestations and PSD is still undefined, as the relation may be bidirectional, or they may occur independently. Robertson and colleagues [49] stated that both psychotic symptoms and cognitive deficits were related to the site of the lesion, as they noticed that patient with psychotic manifestations had left sided lesion, but in the current study, we cannot confirmed that as we excluded patients with severe aphasia. Furthermore, another study demonstrated that psychotic symptoms were prevalent in patients with severe cognitive deficit [50].
More than 90% of our patients had mild and moderate degrees of PSD which were comparable to those of El Tallawy and his colleagues in their studies in Al Kharga and Al-Quseir cities [28, 29]. So that, the majority of our PSD patients were candidates for treatment, this encourages us for further studies on PSD treatment protocols.
Our results confirmed the postulation of other studies [9,10,11], which stated that PSD can contribute to worse outcome through lack of compliance and less intensive stroke management, where only about 1% of our patients with PSD showed clinical improvement. These patients were highly dependent in instrumental activities of daily living that required more complex tasks [51] and according to BI, more than three-quarters (77.2%) of them had poor and very poor outcome as compared to less than half of patients without dementia (45.5%).
The results of the present study should be interpreted in the light of the following limitations. First, lack of a uniform diagnostic criteria, specific assessment tools, and reliable markers such as a biochemical marker for identification of PSD. Second, inability to have serial assessments of cognitive function with inability to assess different cognitive domains.
Multi-centres’ future researches should be given high priority on the pathophysiology and long-term cognitive outcomes of stroke patients; this may come up with new diagnostic neuroimaging techniques and biomarkers for early recognition of PSD.
Conclusion
This research indicated that PSD is a quite common problem and may adversely affect outcome of stroke. So, assessment of cognitive status at an early stage of stroke and identifying post-stroke risk factors and predictors of cognitive impairment are very important. This will assist in the prevention of further cognitive decline and improve psychological wellbeing through effective intervention.
Availability of data and materials
Data and materials supporting the results of this article are available with the authors on reasonable request.
Abbreviations
- PSD:
-
Post-stroke dementia
- AF:
-
Atrial fibrillation
- BI:
-
Barthle Index
- CVS:
-
Cerebrovascular stroke
- ECG:
-
Electrocardiography
References
Delbari A, Roghani RS, Tabatabaei SS, Rahgoza M, Lokk J. Stroke epidemiology and one-month fatality among an urban population in Iran. Int J Stroke. 2011;6(3):195–200.
Ankolekar S, Geeganage C, Anderton P, Hogg C, Bath PM. Clinical trials for preventing post stroke cognitive impairment. J Neurol Sci. 2010;299(12):168–74.
Stephens S, Kenny RA, Rowan E, Allan L, Kalaria RN, Bradbury M, et al. Neuropsychological characteristics of mild vascular cognitive impairment and dementia after stroke. Int J Geriatr Psychiatry. 2004;19(11):1053–7.
Erkinjuntti T. Diagnosis and management of vascular cognitive impairment and dementia. J Neural Transm Suppl. 2002;63:91–109.
Leys D, Hénon H, Cordoliani M, Pasquier F. Post stroke dementia. Lancet Neurol. 2005;4(11):752–9.
Gorelick PB, Nyenhuis D. Stroke and cognitive decline. JAMA. 2015;314(1):29–30.
Chi Hu G, Chen Y. Post-stroke dementia: epidemiology, mechanisms and management. Int J Gerontol. 2017:1–5.
Moroney JT, Bagiella E, Tatemichi TK, Paik MC, Stern Y, Desmond DW. Dementia after stroke increases the risk of long-term stroke recurrence. Neurology. 1997;48:1317–25.
Iadecola C. The pathology of vascular dementia. Neuron. 2013;80:844–66.
Barba R, Morin MD, Cemillán C, Delgado C, Domingo J, Del Ser T. Previous and incident dementia as risk factors for mortality in stroke patients. Stroke. 2002;33(8):193–8.
Hénon H, Durieu I, Lebert F, Pasquier F, Leys D. Influence of pre-stroke dementia on early and delayed mortality in stroke patients. J Neurol. 2003;250(1):10–6.
Melkas S, Oksala NK, Jokinen H, Pohjasvaara T, Vataja R, Oksala A, et al. Post stroke dementia predicts poor survival in long-term follow-up: influence of pre-stroke cognitive decline and previous stroke. J Neurol Neurosurg Psychiatry. 2009;80(8):865–70.
Xiu S, Zheng Z, Liao Q, Chan P. Different risk factors for cognitive impairment among community- dwelling elderly with impaired fasting glucose or diabetes. Diabetes Metab Syndr Obes. 2019;12:121–30.
Mahoney FI, Barthel D. Functional evaluation: the Barthel Index. Md Med J. 1965;14:61–5.
Hachinski VC, Iliff LD, Zilhka E, Du Boulay GH, McAllister VL, Marshall J, et al. Cerebral blood flow in dementia. Arch Neurol. 1975;32:632–7.
American Psychiatric Association [APA]. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Folstein M, Folstein S, Mc HP. Mini-Mental State: a practical guide for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;53:189–98.
Faul F, Erdfelder E. George lang A. Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(1):175–91.
IBM_SPSS, Statistical Package for Social Science. Ver.21. Standard version, S. Inc, Editor 2012, Copyright © SPSS Inc: NY-USA
Hénon H, Pasquier F, Leys D. Post-stroke dementia. Cerebrovasc Dis. 2006;22:61–70.
Cristina SI, Sudha S, Alexa B, Rhoda A, Carlos SK, Margaret KH, et al. Dementia after stroke: The Framingham Study. Stroke. 2004;35:1264–8.
Iranmanesh F, Sheykholeslami NZ, Rahimdel A, Gadari F, Vazirinajad R, SyedYazdi F. Post-stroke dementia and its putative risk factors: a hospital-based study. Pakistan J Neurol Sci (PJNS). 2015;10(1):192–8.
Lindén T, Skoog I, Fagerberg B, Steen B, Blomstrand C. Cognitive impairment and dementia 20 months after stroke. Neuroepidemiology. 2004;23(12):45–52.
Tu Q, Ding B, Yang X, Bai S, Tu J, Liu Z, et al. The current situation on vascular cognitive impairment after ischemic stroke in Changsha. Arch Gerontol Geriatr. 2014;58(2):236–47.
Mahon S, Parmar P, Barker-Callo S, Krishnamurthi R, Jones K, Theadom R, et al. Determinants, prevalance, and trajectory of long-term post-stroke cognitive impairment: results from a 4-year follow-up of the ARCOS-IV study. Neuroepidemiology. 2017;49:129–34.
Borenstein AR, Copenhaver CI, Mortimer JA. Early life risk factors for Alzheimer disease. Alzheimer Dis Assoc Disord. 2006;20:63–72.
Zhou DH, Wang JY, Li J, Deng J, Gao C, Chen M. Study on frequency and predictors of dementia after ischemic stroke: Chongqing stroke study. J Neurol. 2004;251:421–7.
El Tallawy HN, Farghly WM, Shehata GA, Hakeem NA, Rageh T, Abo-Elfetoh N, et al. Prevalence of dementia in Al Kharga District, New Valley Govern., Egypt. Neuroepidemiology. 2012;38(3):130–7.
El Tallawy HN, Farghly WM, Rageh TA, Badry R, Abdelhakim N, Abd elhameed M, et al. Prevalence of dementia in Al-Quseir city, Red Sea Governorate, Egypt. Clin Interv Aging. 2014;(9):9–14.
Khedr E, Fawi G, Abbas MA, Mohammed T, Aboelfotoh N, Noaman M, et al. Prevalence of mild cognitive impairment and dementia among the elderly population of Qena Governorate, Upper Egypt: a community-based study. J Alzheimers Dis. 2015;45(1):117–26.
Perneczky R, Wagenpfeil S, Lunnetta KL, Cupples LA, Green RC, Decarli C, et al. Education attenuates the effect of medial temporal lobe atrophy on cognitive function in Alzheimer’s disease: The MIRAGE study. J Alzheimers Dis. 2009;17:855–62.
Sharp ES, Gatz M. Relationship between education and dementia: an updated systematic review. Alzheimer Dis Assoc Disord. 2011;25(4):289–304.
Brayne C, Ince PG, Keage HA, McKeith IG, Matthews FE, Polvikoski T, et al. Education, the brain and dementia: Neuroprotection or compensation? Brain. 2010;13(3):2210–6.
Mirza SS, Portegies ML, Wolters FJ, Hofman A, Koudstaal PJ, Tiemeier H, et al. Higher education is associated with a lower risk of dementia after a stroke or TIA. The Rotterdam Study. Neuroepidemiology. 2016;46:120–7.
Farrag A, Farwiz HM, Khedr EH, Mahfouz RM, Omran SM. Prevalence of Alzheimer’s disease and other dementing disorders: Assiut-Upper Egypt study. Dement Geriatr Cogn Disord. 1998;9(6):323–8.
Rorsman B, Hagnell O, Lanke J. Prevalence and incidence of senile and multi-infarct dementia in the Lundby Study: a comparison between the time periods 1947–1957 and 1957–1972. Neuropsychobiology. 1986;15(3–4):122–9.
Tang WK, Chan SS, Chiu HF, Ungvari GS, Wong KS, Kowk T, et al. Frequency and determinants of post-stroke dementia in Chinese. Stroke. 2004;35:930–5.
Henon H, Durieu I, Guerouaou D, Lebert F, Pasquier F, Leys D. Post-stroke dementia: incidence and relationship to pre-stroke cognitive decline. Neurology. 2001;57:1216–22.
Altieri M, Di Piero V, Pasquini M. Delayed post-stroke dementia: a 4-year follow-up study. Neurology. 2004;62:2193–7.
Nitrini R, Bottino CM, Albala C, Capunay SC, Ketzoian C, Rodriquez JJ, et al. Prevalence of dementia in Latin America: a collaborative study of population-based cohorts. Int Psychogeriatr. 2009;21(4):622–30.
Bennett DA, Wilson RS, Schneider JA, Evans DA, Beckett LA, Aggarwal NT, et al. Natural history of mild cognitive impairment in older persons. Neurology. 2002;59:198–205.
Guerchet M, M’belesso P, Mouanga AM, Bandzouzi B, Tabo A, Houinato DS, et al. Prevalence of dementia in elderly living in two cities of Central Africa: the EDAC survey. Dement Geriatr Cogn Disord. 2010;30:261–8.
Gabelli C, Codemo A. Gender differences in cognitive decline and Alzheimer’s disease. Ital J Gender-Specific Med. 2015;1:21–8.
Michal K, Sebastian F, Cheng Y, Jiming F, Gustavo S. Atrial fibrillation diagnosed after stroke and dementia risk: cohort study of first-ever ischemic stroke patients aged 65 or older. Europace. 2019;(0):1–9.
Heijman J, Voigt N, Nattel S, Dobrev D. Cellular and molecular electrophysiology of atrial fibrillation initiation, maintenance, and progression. Circ Res. 2014;114:1483.
Yang J, Wong A, Wang Z, Liu W, Au L, Xiong Y, et al. Factors for incident dementia after stroke and transient ischemic attack. Alzheimer Dement. 2015;11:16–23.
Béjot Y, Aboa-Eboulé C, Durier J, Rouaud O, Jacquin A, Ponavoy E, et al. Prevalence of early dementia after first ever stroke: a 24-year population-based Study. Stroke. 2011;42:607–12.
Pendlebury ST, Rothwell PM. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol. 2009;8(11):1006–18.
Turner-Stokes L. Post stroke depression: getting the full picture. Lancet. 2003;361:1757–8.
Rasquin S, Lodder J, Verhey F. The association between psychiatric and cognitive symptoms afer stroke: a prospective study. Cerebrovasc Dis. 2005;19(5):309–16.
Claesson L, Linden T, Skoog I, Blomstrand C. Cognitive impairment after stroke impact on activities of daily living and costs of care for elderly people: the Goteborg 70+ stroke study. Cerebrovasc Dis. 2005;19(2):102–9.
Acknowledgements
We acknowledge the help and support of the medical and administrative staff of the neuropsychiatric department, Aswan and Assuit University Hospitals. It was not possible to complete this work without the help, support, and approval of the patients’ caregiver.
Funding
No funding received in this study.
Author information
Authors and Affiliations
Contributions
BA: concept, design, literature search, clinical studies, manuscript preparation, editing, and review. MA: definition of intellectual content, literature search, and manuscript review. AI: methodological design, data analysis, statistical analysis, manuscript preparation, editing, and review. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval for this study was obtained from IRB of Medical Faculty, Aswan University prior to study execution (IRB No. Asw-376-7-19). The research complied with Helsinki. In addition, all subjects (or their parents or legal guardians) have given their written informed consent. The written informed consent was clear and indicated the purpose of the study, and their freedom to participate or withdraw at any time without any obligation. Furthermore, participants’ confidentiality and anonymity were assured by assigning each participant with a code number for the purpose of analysis only. The study was not based on any incentives or rewards for the participants.
Consent for publication
Not applicable in this section.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al Fawal, B., Ibrahim, A. & Abd Elhamed, M. Post-stroke dementia: frequency, predictors, and health impact. Egypt J Neurol Psychiatry Neurosurg 57, 15 (2021). https://doi.org/10.1186/s41983-021-00270-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-021-00270-y