Abstract
Background
Aneurysmal subarachnoid hemorrhage (aSAH) can have serious consequences related to vasospasm and delayed cerebral ischemia (DCI). Serum biomarkers have emerged as a promising assessment tool to facilitate earlier diagnosis of cerebral vasospasm (CV) and to identify pre-clinical vessel narrowing.
Objectives
Our aim was to detect the predictive value of serum biomarkers such as von Willebrand factor (vWF), vascular endothelial growth factor (VEGF) and matrix metalloproteinase9 (MMP-9) in CV after aSAH.
Subjects and methods
Thirty five patients with recent aSAH were included. Patients were divided into two groups; 19 patients (CV group) and 16 patients (non-CV group). The CV group was further subdivided into 9 symptomatic (DCI) and 10 asymptomatic patients. All patients underwent transcranial Doppler (TCD) evaluations three times a week for 2 weeks measuring the mean flow velocities. Serum level of vWF, MMP-9, and VEGF were assessed twice (at onset and within 2 weeks).
Results
A statistically significant increase in serum biomarker levels was found in the CV group. Cutoff value for vWF, MMP-9, and VEGF were > 4985 ng/ml, > 495 ng/ml, and > 184 pg/ml, respectively. Statistically significant positive correlations were found between serum levels of biomarkers and degree of vasospasm. No difference was found in the biomarkers between symptomatic CV and asymptomatic CV.
Conclusion
Serum biomarkers are a reliable tool to predict CV following aSAH, their levels reflect the severity of vascular vasospasm, yet, they cannot predict DCI. TCD has a strong role in early detection, monitoring of post subarachnoid vasospasm and successfully capturing asymptomatic DCI.
Similar content being viewed by others
Introduction
Aneurysmal subarachnoid hemorrhage (aSAH) is a neurologic emergency caused by a brain aneurysm burst, resulting in a bleeding into the subarachinoid space. Around 10.5 per 100,000 persons per year developed subarachnoid hemorrhage (SAH) [1]. Approximately 20 to 30% of patients with aSAH suffer from delayed cerebral ischemia (DCI) due to cerebral vasospasm (CV) [2]. Cerebral vasospasm is a heterogeneous process that has both radiographic and clinical subtypes. Radiographic CV (RCV) is a complex transient narrowing of intradural subarachnoid arteries and occur in up to 70%, while clinical CV (CCV) occur in about 50% and it is a syndrome of neurologic deterioration related to initial aSAH [3]. A variety of different tools had been used to detect DCI such as the occurrence of focal neurological impairment, a decrease of at least 2 points on the Glasgow Coma Scale which lasts for at least 1 h or daily transcranial Doppler (TCD) bedside monitoring [2]. Transcranial Doppler is a recognized guideline tool for early detection of vasospasm [2]. Yet, the interval between TCD velocity changes and subsequent ischemia is insufficient for optimizing the benefits of medical management and early intervention [4]. Discovery of serum biomarkers in the context of SAH in relation to CV such as von Willebrand Factor (vWF), vascular endothelial growth factor (VEGF) and Matrix metalloproteinase 9 (MMP-9) have been shown to be a reliable method for predicting CV and improve monitoring of the response to treatment [5]. Aim of this work is to detect the role of serum vWF, MMP-9 and VEGF as a predictive value in CV following aSAH and to find a relationship between these biomarkers and actual occurrence and degree of CV and also to evaluate their advantages over clinical scales and radiological tools in predicting CV.
Subjects and methods
This is a cross-sectional study conducted on 35 patients with recent aSAH (recruited within the first 3 days). The number of patients is calculated with sample size for frequency in population by Openepi software with confidence interval 95%. We excluded patients with aSAH for more than 72 h, patients who were taking anticoagulants such or antiplatelet drugs last month, patients who had blood diseases, patients who had liver and kidney dysfunction and women who were in pregnancy and lactation stages that may affect level of biomarkers.
They were selected from emergency departments of Neurology and Neurosurgery departments, Cairo University Hospitals.
The patients were divided into two groups; the first group included patients who developed cerebral vasospasm (CV group, n = 19, 54.3%) and the second group included patients who did not develop vasospasm (non-CV group, n = 16, 45.7%). The first group (patients who developed vasospasm) was further subdivided into symptomatic (DCI) group (n = 9, 47.4%) and asymptomatic group (n = 10, 52.6%).
All the patients were subjected to the Evaluation by World Federation of Neurosurgical Societies (WFNS) scale, Hunt and Hess (H and H) scale as a clinical tool for severity assessment, and noncontrast CT brain with GE multislice 64 32 detector*2 USA 2015 HS60, Korea and graded by the modified Fisher scale as a radiological tool for severity assessment.
Evaluation and follow-up of vasospasm and VC severity were done by TCD using EZ-DOP with software version DWL2000TM Doppler, Germany GmbH (2009) three times per week till day 14. Measurements included the mean flow velocity of the middle cerebral artery and ipsilateral internal carotid artery (ICA) through the submandibular window. The Lindegaard ratio was then calculated by dividing the MFV of MCA by MFV of ICA [6]. Patients were classified to have vasospasm if the MFV of MCA was > 120 cm/s and the Lindegaard ratio of ipsilateral MCA and ICA was > 3, with mild-to-moderate vasospasm 3–4, moderate to sever 5–6 and sever vasospasm ≥ 6 [6].
Two venous serum samples for measurement of vWF, VEGF and MMP-9 were collected using Diagnostic Automation Sm ELISA test kit used in ELISA DR 200D R-200Bs Microplate Reader, 2016 China; the first sample was collected on day 2 of aSAH onset and the second samples were collected at day 15 for the non-CV group, and at the time of identification of vasospasm for the CV group. Collected blood samples were centrifuged and the resulting supernatants were immediately frozen at – 80 °C until analysis in the ELISA Unit of Kasr Al Ainy University Hospital, Cairo.
Statistical analysis
Data were coded and entered using the statistical package SPSS, version 25 (SPSS Inc., Chicago, IL, USA, 2009). Data were summarized using mean and standard deviation for quantitative variables and frequencies (number of cases) and relative frequencies (percentages) for categorical variables. Comparisons between groups were done using analysis of variance (ANOVA) with multiple comparisons post hoc test or unpaired test in normally distributed quantitative variables while nonparametric Kruskal–Wallis test and Mann–Whitney test were used for non-normally distributed quantitative variables. For comparing categorical data, Chi square (χ2) test was performed. Exact test was used instead when the expected frequency is less than 5. Correlations between quantitative variables were done using Spearman correlation coefficient. Multivariate linear regression model was conducted. p values less than 0.05 were considered as statistically significant.
Results
Demographic and clinical data at presentation are represented in Table 1.
TCD of the CV group shows markedly higher flow velocity at the time CV compared to non-CV group throughout their course. The CV group MCA MV mean was 132.15 ± 12.4, ICA MV was 34.05 ± 5.28 and Lindegaard ratio ranged from 3 to 5.7 (11 patients had mild to moderate while 8 patients had moderate to severe). In the non-CV group, the mean MCA MV was 45.44 ± 11.97, ICA was 29.19 ± 4.10 and Lindegaard ratio ranged from 1.1 to 2.
No statistically significant relations were found between demographic and prior medical history data (age, sex, smoking, diabetes and hypertension) and WFNS or H and H grades (p > 0.05). Also, these data did not show a difference between the CV and the non-CV groups (p > 0.05).
No statistically significant relation was detected between WFNS, Hunt and Hess grades and occurrence of CV or DCI.
A higher proportion of patients with high grades of modified Fisher scale was found in the CV group compared to the non-CV group (p = 0.019) yet no difference was found between symptomatic and asymptomatic groups.
Serum biomarkers did not differ according to sex, age, smoking, HTN or DM.
Serum concentration of vWF, VGEF and MMP-9 in the CV and non-CV groups in the 2nd day, were increased in a statistically significant way in the CV group (prior to occurrence of vasospasm) compared with the non-CV group (p < 0.001, Table 2).
Correlation between Lindegaard ratio and serum biomarker concentrations of vWF, VGEF and MMP-9 in the study group shows highly significant positive correlation with p value < 0.001.
Binary Logistic Multi-Regression analysis was done for vasospasm and serum biomarker variables. It showed that serum vWF (ng/ml), VGEF (pg/ml) and MMP-9 (ng/ml) were significant predictors of vasospasm with p values of 0.044, 0.028 and 0.012, respectively.
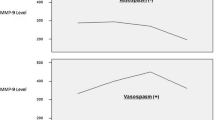
ROC curves were constructed for serum biomarkers in the second day of aSAH as predictors of CV in all included patients. All serum biomarkers were significant predictors as denoted by the significantly large area under the curves (AUCs); elevated serum vWF levels of more than 4985 ng/ml, MMP-9 levels of more than 495 ng/ml, and VEGF levels of more than 184 pg/ml each independently increased the odds of subsequent vasospasm (Fig. 1, Table 3).
Statistically significant positive correlation was found between Lindegaard ratio and each serum biomarker in the CV group (p < 0.001).
Statistically significant increase in serum biomarkers occurred in follow-up serum samples at the time of vasospasm in the CV group (p < 0.05) compared to first sample (Table 4), unlike the non-CV group who showed no difference between the two samples (p > 0.05).
No statistically significant difference was found in serum biomarkers of the second sample between the symptomatic group (DCI) and non-symptomatic group (p > 0.05, Table 4).
Diagnostic performance including cut-off values, sensitivity and specificity of serum biomarker concentration are represented in Table 5.
Discussion
Prediction of vasospasm and delayed cerebral ischemia in patients with aneurysmal subarachnoid hemorrhage remains a challenge. So far, clinical predictors and imaging have offered controverted prognostic values [4]. This study showed that serum biomarkers can be predictors for CV yet they are less accurate in the prediction of delayed cerebral ischemia (DCI). Therefore, TCD is used as a continuous monitoring system of the CBF in patients with aSAH to detect early signs suggestive of CV, and TCD can successfully capture asymptomatic DCI. In our study, age, gender, smoking, HTN and DM were not risk factors for the occurrence of CV. Contradictory studies have shown relation of age to CV; one stating that it was related to younger age [7,8,9] and another relating it to older age [10]. Most authors have concluded that there was no correlation between the age and incidence or severity of CV [11,12,13]. Gender and diabetes mellitus have been rejected as well by Mijiti and colleagues (2016) as a possible cause of CV [14]. Numerous studies found that cigarette smoking or pre-existing HTN were not associated with CV [15, 16]. Regarding clinical and radiological severity data, our results demonstrated that there was a positive correlation between the high grades of modified Fisher scale and the development of CV, yet, we noticed no relation between H and H scale grades or WFNS grades and development of CV. Previous studies have shown different results concerning CT finding in relation to worse outcome; some showed that the higher the modified Fisher grades, the higher the incidence of CV [17,18,19], while others found no relation [7, 9]. Clinical scales relation to outcome have shown more consistent observations as most of the studies could not correlate initial clinical presentation of the patient to the occurrence of CV or DCI [7, 9, 20]. In this study, we investigated the association between initial concentrations of serum MMP-9, vWF and VEGF which represents markers for endothelial dysfunction with the occurrence of the CV. We also took a second sample either following vasospasm or at day 14 in patients who did not develop vasospasm to follow the serum level variability in different clinical progression. The main finding of our study was a highly statistically significant crude positive association between serum biomarker concentrations in the first sample and incidence of CV. Furthermore, we found that there was highly significant positive correlation between Lindegaard ratios with serum concentration levels of these biomarkers in all patients included in the study. The study demonstrated that early concentrations of serum MMP-9, vWF and VEGF were highly sensitive and specific for predicting subsequent CV with MMP-9 being the most significant predictor. Yet, no difference was found between patients who developed DCI and those who did not. This finding rejects the fact that the biomarkers were related to ischemic stroke [4]. The biomarker serum levels were not affected by demographic, medical history or clinical scales. Also, these biomarkers had low statistically significant correlation with modified Fisher scale grades which suggest that these biomarkers may be an independent predictor of CV. Our results were in accordance with many studies that confirmed the relation of the serum levels of MMP-9 [21] and vWF levels [22] to the occurrence of the CV group compared to the non-CV group.
In the current study, cutoff values showed that elevated serum levels of more than 4985 ng/ml, 495 ng/ml and 184 pg/ml in vWF, MMP-9 and VEGF, respectively independently increase the odds of subsequent CV. McGrit and colleagues (2002) reported that elevated plasma vWF levels > 5,500 ng/ml, MMP-9 levels > 700 ng/ml and VEGF levels > 0.12 ng/ml each independently increased the odds of CV [4]. We, thus, recommend that every institution must have their own reference cutoff value. The serum levels of these biomarkers kept increasing in the second sample in patients who developed CV unlike those who did not have CV. The results of this study also showed that the serum concentrations of these biomarkers in the non-CV group did not increase or decrease significantly along with time, so we considered level of serum biomarkers in the non-CV patients (as control) a reference value. These findings suggest that these markers may be specific for the arterial changes associated with CV. Yet, absence of difference between patients who developed delayed cerebral ischemia (DCI) and those who did not exclude the possibility of relation between these biomarkers and ischemic sequelae as stated before [22] making them specific for vasospasm. Doppler ultrasound findings showed a highly significant positive correlation between the Lindegaard ratio (reflecting degree of vasospasm) and serum concentration level of each one of the biomarkers in all patients irrespective of CV. This finding confirms that these biomarkers may play a role in the pathophysiological mechanism of vasoconstriction, yet, that the development of CV begins when these biomarkers cross a certain threshold level.
Conclusion
TCD has a significant role in early detection, monitoring of post subarachnoid vasospasm and successfully capturing asymptomatic DCI. VEGF, MMP-9 and vWF are strong independent predictors of vasospasm in patients with aSAH, yet, they cannot predict delayed cerebral ischemia. These biomarkers show better predictive value for CV compared to patient’s initial clinical presentation and brain imaging.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to the current Cairo University regulations and Egyptian legislation but are available from the corresponding author on reasonable request and after institutional approval.
Abbreviations
- ANOVA:
-
Analysis of variance
- aSAH:
-
Aneurysmal subarachnoid hemorrhage
- CCV:
-
Clinical CV
- CT:
-
Computed tomography
- CTA:
-
CT angiography
- CV:
-
Cerebral vasospasm
- DIC:
-
Delayed cerebral ischemia
- H and H:
-
Hunt and Hess
- HTN:
-
Hypertension
- ICA:
-
Internal carotid artery
- IQR:
-
Interquartile range
- MCA:
-
Middle cerebral artery
- MFV:
-
Mean flow velocity
- MMP-9:
-
Matrix metalloproteinase 9
- RCV:
-
Radiographic CV
- ROC:
-
Receiver operating characteristic
- TCD:
-
Transcranial Doppler
- VEGF:
-
Vascular endothelial growth factor
- vWF:
-
von Willebrand factor
- WFNS:
-
World Federation of Neurosurgical Societies
References
Grasso G, Alafaci C, Macdonald RL. Management of aneurysmal subarachnoid hemorrhage: state of the art and future perspectives. Surg Neurol Int. 2017;8:11.
Vergouwen MD, Vermeulen M, van Gijn J, Rinkel GJ, Wijdicks EF, Muizelaar JP, et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke. 2010;41(10):2391–5.
Velat GJ, Kimball MM, Mocco JD, Hoh BL. Vasospasm after aneurysmal subarachnoid hemorrhage: review of randomized controlled trials and meta-analyses in the literature. World Neurosurg. 2011;76(5):446–54.
McGirt MJ, Lynch JR, Blessing R, Warner DS, Friedman AH, Laskowitz DT. Serum von Willebrand factor, matrix metalloproteinase-9, and vascular endothelial growth factor levels predict the onset of cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2002;51(5):1128–34.
Przybycien-Szymanska MM, Ashley WW Jr. Biomarker discovery in cerebral vasospasm after aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2015;24(7):1453–64.
Gonzalez NR, Boscardin WJ, Glenn T, Vinuela F, Martin NA. Vasospasm probability index: a combination of transcranial Doppler velocities, cerebral blood flow, and clinical risk factors to predict cerebral vasospasm after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2007;107(6):1101–12.
Kale SP, Edgell RC, Alshekhlee A, Borhani Haghighi A, Sweeny J, Felton J, et al. Age-associated vasospasm in aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2013;22(1):22–7.
Malinova V, Schatlo B, Voit M, Suntheim P, Rohde V, Mielke D. Identification of specific age groups with a high risk for developing cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurg Rev. 2016;39(3):429–36.
Arias MR, Pacheco CD, Agudelo Y. Risk factors for cerebral vasospasm in patients with spontaneous subarachnoid hemorrhage. Rev Colomb Radiol. 2017;28(2):4657–62.
de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. 2007;78(12):1365–72.
Jung SW, Lee CY, Yim MB. The relationship between subarachnoid hemorrhage volume and development of cerebral vasospasm. J Cerebrovasc Endovasc Neurosurg. 2012 Sep;14(3):186–91.
Ryttlefors M, Enblad P, Ronne-Engström E, Persson L, Ilodigwe D, Macdonald RL. Patient age and vasospasm after subarachnoid hemorrhage. Neurosurgery. 2010;67(4):9117.
Inagawa T, Yahara K, Ohbayashi N. Risk factors associated with cerebral vasospam following aneurysmal subarachnoid hemorrhage. Neurol Med Chir. 2014;54(6):465–73.
Mijiti M, Mijiti P, Axier A, Amuti M, Guohua Z, Xiaojiang C, et al. Incidence and predictors of angiographic vasospasm, symptomatic vasospasm and cerebral infarction in Chinese patients with aneurysmal subarachnoid hemorrhage. PLoS One. 2016;11(12):e0168657.
Badjatia N, Topcuoglu MA, Buonanno FS, Smith EE, Nogueira RG, Rordorf GA, et al. Relationship between hyperglycemia and symptomatic vasospasm after subarachnoid hemorrhage. Crit Care Med. 2005;33(7):1603–9.
Dupont SA, Wijdicks EF, Manno EM, Lanzino G, Rabinstein AA. Prediction of angiographic vasospasm after aneurysmal subarachnoid hemorrhage: value of the Hijdra sum scoring system. Neurocrit Care. 2009;11(2):172–6.
Eagles ME, Jaja BNR, Macdonald RL. Incorporating a modified Graeb Score to the modified Fisher scale for improved riskv prediction of delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. Neurosurgery. 2018;82(3):299305.
Platz J, Güresir E, Wagner M, Seifert V, Konczalla J. Increased risk of delayed cerebral ischemia in subarachnoid hemorrhage patients with additional intracerebral hematoma. J Neurosurg. 2017;126(2):504–10.
Griessenauer CJ, Starke RM, Foreman PM, Hendrix P, Harrigan MR, Fisher WS, et al. Associations between endothelin polymorphisms and aneurysmal subarachnoid hemorrhage, clinical vasospasm, delayed cerebral ischemia, and functional outcome. J Neurosurg. 2018;128(5):1311–7.
Smith ML, Abrahams JM, Chandela S, Smith MJ, Hurst RW, Le Roux PD. Subarachnoid hemorrhage on computed tomography scanning and the development of cerebral vasospasm: the Fisher grade revisited. Surg Neurol. 2005;63(3):229–34.
Wang L, Gao Z. Expression of MMP-9 and IL 6 in patients with subarachnoid hemorrhage and the clinical significance. Exp Ther Med. 2018;15(2):1510–4.
Li WH, Hui CJ, Ju H. Expression and significance of vWF, GMP-140 and ADAMTS13 in patients with aneurysmal subarachnoid hemorrhage. Eur Rev Med Pharmacol Sci. 2017;21(19):4350–6.
Acknowledgements
Not applicable
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MMA participated in the concept and the study design. AAN applied the inclusion and exclusion criteria and drafted the manuscript. SMA participated in the concept and design of the study. AMA participated in the concept and design of the study and is responsible for the laboratory handling, preparation, and analysis of the blood samples. AMAS participated in the design of the study and analysis of data, helped in the clinical examination, helped in applying the inclusion and exclusion criteria, and performed the statistical analysis. AAE is responsible for the coordination and recruitment of participants. SHO helped in the clinical examination and data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consent was taken from each patient. All data obtained from every patient were confidential and were not used outside the study. The patients have the rights to withdraw from the study at any time without giving any reason. All the cost of the investigations was afforded by the researcher. Our study was approved by the ethical committee of the Department of Neurology, Faculty of Medicine, Cairo University, on 5th of May 2017, but Cairo University does not provide the approval reference number.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Abdelnaseer, M.M., Nemr, A.A., Ahmed, S.M. et al. Role of serum biomarkers and transcranial Doppler in predicting cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Egypt J Neurol Psychiatry Neurosurg 56, 27 (2020). https://doi.org/10.1186/s41983-020-0156-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-020-0156-x