Abstract
Background
Prognostic significance of troponin-I (T-I) elevation for poor short-term outcome in thrombolyzed ischemic stroke patients remains uncertain.
Objectives
To evaluate its role as a predictive biomarker of short-term outcome in thrombolyzed ischemic stroke patients.
Methods
This study included 72 acute ischemic stroke patients who were treated with intravenous thrombolytic therapy. All patients were subjected to clinical assessment and measurement of serum T-I level on admission. Outcome was assessed 3 months after stroke onset using the National Institute of Health Stroke Scale (NIHSS) and modified Rankin scale.
Results
Thirteen patients had elevated serum T-I level (group 1) and the remaining 59 were classified as group 2. Group 1 had a higher statistically significant older age, history of diabetes mellitus (DM), previous stroke, atrial fibrillation (AF), and admission NIHSS score, with significant decrease in high-density lipoprotein cholesterol (P < 0.05). Regarding the outcome of both groups, good outcome was significantly less common among group 1. Also, death was significantly more common among group I. Poor outcome in group 1 were significantly associated with older age, DM, AF, elevated serum T-I level at admission, and higher admission NIHSS score (P = 0.03, 0.04, 0.02, 0.05, and 0.001 respectively). The predictors of poor outcome in group 1 were elevated serum T-I level at admission, higher admission NIHSS score, and DM (P = 0.001, 0.02, and 0.05 respectively).
Conclusion
Elevated serum T-I levels on admission is a reliable prognostic predictor of poor outcome in thrombolyzed ischemic stroke patients.
Trial registration
ClinicalTrials.govNCT03925298 (19 April 2019) “retrospectively registered,”
Similar content being viewed by others
Introduction
Ischemic stroke is a leading cause of mortality and disability [1]. Early restoration of blood flow to the infarct brain tissue is the only way to rescue those patients [2]. Intravenous thrombolysis with recombinant tissue plasminogen activator is the only approved treatment of acute ischemic stroke patients presenting within 4.5 h of symptom onset [3].
Troponin is sensitive and specific biomarker of myocardial necrosis. It has been reported that elevated serum troponin levels are found in acute stroke patients. In addition, elevated serum troponin levels have been linked to poor outcome of cerebrovascular diseases [4]. The etiology of elevated serum troponin levels in acute ischemic stroke patients is not completely understood, but may be related to increased cardiac strain in the setting of acute hypertension, thrombotic coronary ischemia, may reflect the underlying ischemic stroke etiology such as atrial fibrillation, or may be secondary myocardial injury attributable to central activation of the sympatho-adrenal system [5].
To date and up to our knowledge, the prognostic significance of troponin elevation for poor short-term outcomes in thrombolyzed ischemic stroke patients is not well established. We, therefore, investigated the prognostic significance of troponin elevation for poor short-term outcome after intravenous thrombolysis with recombinant tissue plasminogen activator in patients presented with acute ischemic stroke.
Methods
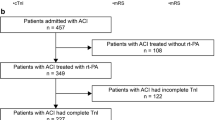
This prospective cohort study was conducted during the period from January 2017 to January 2019 in the intensive care and stroke units of the Neurology Department at our university hospitals. Eighty-one thrombolyzed ischemic stroke patients were enrolled in this study. Patients who did not complete the study (9 patients were lost during follow-up) were eliminated. So the study included seventy-two patients (34 males and 38 females) who fulfilled the inclusion and exclusion criteria.
The inclusion and exclusion criteria were according to the guidelines from the American Heart Association/American Stroke Association [6].
Inclusion criteria
Patients presented with acute ischemic stroke that lasted for ≤ 4.5 h. Ischemic stroke was diagnosed clinically and radiologically. Those patients were treated with intravenous thrombolytic therapy (recombinant tissue plasminogen activator (rt-PA)).
Exclusion criteria
The exclusion criteria were according to the American Stroke Association exclusion criteria for intravenous thrombolytic therapy.
All patients in this study were subjected to both clinical evaluation and investigations:
Clinical evaluation that included the following:
-
Thorough history taking
-
Thorough general and neurological examination
-
Assessment of stroke severity using the National Institute of Health Stroke Scale (NIHSS) at admission [7]
Assessment of neurological outcome after 3 months was done by using the NIHSS and the modified Rankin scale (mRS). The mRS consists of 6 grades, from 0 to 5, with the best score 0 (no symptoms) and the worst score 5 (severe disability). Poor outcome was defined as death or disability (mRS scores ≥ 2) [8]. While, good outcome (neurological improvement) was defined as mRS scores of 0 to 1 or 8 points improvement in NIHSS [9].
Clinical evaluation and neurological outcome assessment of all included participants was performed blinded to troponin-I levels.
Investigations that included the following:
-
A-
Laboratory investigations. Once we obtained the consent of the patient or his family to participate in the research, serum samples from the patients were drawn using standard venipuncture techniques. Serum troponin-I (T-I) samples were left to clot for about 4 h at room temperature and then centrifuged to obtain the serum which was stored frozen at −20 °C. Serum T-I levels were quantified in an enzyme-linked immune-sorbent assay technology following the manufacturer’s instructions (ALPCO, 26G Keewaydin Drive, Salem NH, 03079, USA).
The upper reference levels of serum T-I for apparently healthy subjects is < 0.01 μg/l. The participants were divided into two groups. Those with elevated serum troponin-I levels (≥ 0.01 μg/L) were in group 1 (46% of them were males and 54% were females), and those with normal serum troponin level (< 0.01 μg/L) were in group 2 (47% of them were males and 53% were females). Studying their clinical data, laboratory values, and neurological outcomes after 3 months has been done.
Also, routine laboratory investigations were done at admission including complete blood count, liver and kidney function tests, random plasma glucose levels, fasting and 2 h post-prandial plasma glucose assessment in diabetic patients, lipid profile including total cholesterol, triglycerides, high-density lipoprotein (HDL), and low-density lipoprotein (LDL), coagulation profile: prothrombin time (PT), international normalized ratio (INR), and activated partial thromboplastin time (aPTT).
-
B-
Cardiac investigation. Electrocardiogram (ECG) was done to all participants. Transthoracic echocardiography also was done when indicated.
-
C-
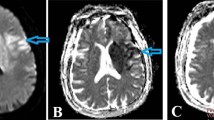
Brain imaging. All of the participants enrolled in this research were subjected to brain computed tomography (CT) scan or brain magnetic resonance imaging (MRI) as early as possible after stroke (within the first 3 h) to exclude stroke mimics or hemorrhagic ones and to detect accurately the site of brain infarction. Brain infarction was evaluated according to their localization as anterior and posterior circulation. Indefinite radiological diagnosis in ischemic stroke patients presented with negative brain CT was the indication for their examination by brain MRI.
Statistical analysis
Statistical Package for Social Science (SPSS) version 22 was used for data analysis [10]. Quantitative data were presented as means and standard deviations. Qualitative data were presented as numbers and percentages. T test was used for comparison of quantitative variables. Comparison of quantitative data was performed using the chi-square (χ2) test, and Fisher’s exact test. Multivariable regression analysis and logistic regression analysis were done to assess independent risk factors that were significantly associated with poor outcome after 3 months among participants. The P value < 0.05 was the cut-off value for significance and P value < 0.001 was the cut-off value for high significance.
Results
This study included seventy-two thrombolyzed ischemic stroke patients (34 males and 38 females). Thirteen patients (18%) out of 72 patients had elevated serum troponin-I level at admission, those patients were classified as group 1 (6 of them were males and 7 were females) and 59 patients (82%) had average normal serum troponin-I level at admission, those patients were classified as group 2 (28 of them were males and 31were females).
Comparison between group 1 and group 2 showed that group 1 had older age, higher incidence of diabetes mellitus, previous stroke, and atrial fibrillation which was statistically significant (P = 0.02, 0.01, 0.003, and 0.04 respectively) (Table 1).
In comparison between group 1 and group 2, we found a statistical significant decrease in high-density lipoprotein cholesterol in group 1 (P = 0.02) and statistical significant increase of admission NIHSS score in group 1 (P = 0.01) (Table 2).
Regarding the neurological outcome of both groups after 3 months of stroke onset, we found that the frequency of neurological improvement (good outcome) was significantly higher in group 2. Also, death (poor outcome) was significantly higher in group I. But as regard disability (poor outcome), there was no statistical significant difference between both groups (Fig. 1).
Poor outcome in group 1 were significantly associated with older age, diabetes mellitus, atrial fibrillation, elevated serum troponin I level at admission, and higher NIHSS score on admission (P = 0.03, 0.04, 0.02, 0.05, and 0.001 respectively) (Table 3).
In logistic regression analysis for detection of poor outcome (death or disability) in group 1, the most significant risk factors were elevated serum troponin-I level at admission (> 0.01 μg/L), higher NIHSS score on admission, and diabetes mellitus (P = 0.001, 0.02, and 0.05 respectively) (Table 4).
Discussion
The presence of troponin elevation in high catecholamine states such as in ischemic stroke has been confirmed. But, the etiology of increased troponin levels in acute stroke patients is still incompletely understood. Jensen et al. studied acute ischemic stroke patients with no overt coronary heart disease. Their findings suggested that etiologies other than an acute coronary syndrome, such as congestive heart failure and renal failure were responsible for the observed elevated troponin levels [11].
Also, it has been suggested that cardiac injury in acute stroke patients is caused by patchy subendocardial hemorrhage or swollen myocytes surrounding the epicardial nerves (myocytolysis) [12]. Jespersen et al. suggested that increased catecholamine release in the myocardium, that likely to originate from the insular cortex, could lead to an excessive release of intracellular calcium ions which can cause myocyte dysfunction and impairment of cardiac function due to the perfusion disturbance at the level of capillaries caused by an enhanced platelet aggregation [13].
Barber et al. found an association between elevated troponin and epinephrine in ischemic stroke patients [14]. Christensen et al. found an association between elevated troponin and cortisol [15]. These findings may suggest a link between the sympathetic nervous system and myocardial cell damage after ischemic stroke.
In this study, we investigated the prognostic significance of troponin elevation for poor short-term outcome after intravenous thrombolysis with recombinant tissue plasminogen activator in acute ischemic stroke patients.
In the current study, an elevated serum level of T-I ≥ 0.01 μg/L was observed in 18% of patients (group 1), and 82% had average normal serum troponin-I level at admission (group 2). Comparison between both groups showed that group 1 had older age, higher incidence of diabetes mellitus, previous stroke, and atrial fibrillation which was statistically significant (P = 0.02, 0.01, 0.003, and 0.04 respectively). Regarding group 1, we found a statistical significant decrease in high-density lipoprotein cholesterol (P = 0.02) and a statistical significant increase of admission NIHSS score (P = 0.01).
In the same line with our results, Faigle and colleagues [3] reported that patients with measured troponin were more likely to have a history of atrial fibrillation and higher NIHSS scores at presentation.
Regarding the neurological outcome, we found that the frequency of major neurological improvement (good outcome) was significantly higher in group 2. Also, death (poor outcome) was significantly higher in group 1. But as regard disability (poor outcome), there was no statistical significant difference between both groups. In the present study, poor outcomes in group 1 were significantly associated with older age groups, diabetes mellitus, atrial fibrillation, elevated serum troponin-I level at admission, and admission NIHSS score. In the same line with our results, Bray and colleagues [16] reported that older thrombolyzed ischemic stroke patients are more likely to have poor outcomes when compared to younger patients.
Also, our results corroborate the findings of Nikneshan and colleagues [17]; they showed that thrombolyzed stroke patients with diabetes have poorer outcomes compared with patients without diabetes. Atrial fibrillation may worsen the clinical outcomes of patients with acute ischemic stroke after thrombolysis. Those patients have increased risk of mortality and less favorable outcome compared to patients without atrial fibrillation [18].
Moreover, thrombolyzed stroke patients with measured troponin had history of atrial fibrillation, and higher NIHSS at presentation that resulted in poor outcome [3]. Stroke can induce stress on the patient’s heart causing troponin to be elevated and this might be an indication of a lower cardiac tolerance caused by the acute stroke [1]. This may be one explanation for the relationship between elevated T-I and a poor short-term outcome found in the present study, and for this reason, physicians should be more careful when dealing with these patients.
In the current study, the most significant risk factors of poor outcome in group 1 were elevated serum troponin-I level at admission, higher NIHSS score on admission, and diabetes mellitus. Our results are supported by that of Faigle and colleagues [3] who found that troponin elevation in thrombolyzed stroke patients is associated with a significant increase in mortality and critical care needs in white but not black patients. Also, this is in accordance with two previous studies [19, 20].
Mehta and colleagues [19] reported that NIHSS at admission > 15, diabetes, and blood sugar > 250 mg/dL, were the significant predictors of the poor outcomes after intravenous thrombolysis for acute ischemic stroke. Liu and colleagues [20] reported that older ages, NIHSS score > 20, and serum glucose on admission > 9.0 mmol/L were independent predictors of poor outcome (hemorrhage) after thrombolysis in their patients.
The association of high serum levels of both of troponin I and glucose in acute cerebrovascular stroke is not yet understood, regardless of that the role of high serum glucose was built up as a hazard factor for platelet-dependent clot formation in coronary illness patients, so coagulation changes might be the ascribed etiology [21]. Moreover, hyperglycemia happens after injury to the central autonomic centers and as a reaction to the release of stress hormones such as cortisol and noradrenaline [22].
Conclusion and recommendation
In conclusion, our study shows that measurement of serum troponin-I level in thrombolyzed ischemic stroke patients could be a useful laboratory marker in the identification of patients at highest risk of poor outcome.
Recommendations
Further large, prospective studies with assessment of both short- and long-term clinical outcomes are needed in the future to improve the outcome in thrombolyzed ischemic stroke patients.
Availability of data and materials
Data and materials supporting the results of this article are included within the article (and its additional file(s)).
Abbreviations
- T-I:
-
Troponin
- NIHSS:
-
National Institute of Health Stroke Scale
- mRS:
-
Modified Rankin scale
- DM:
-
Diabetes mellitus
- AF:
-
Atrial fibrillation
- rt-PA:
-
Recombinant tissue plasminogen activator
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- PT:
-
Prothrombin time
- INR:
-
International normalized ratio
- a PTT:
-
Activated partial thromboplastin time
- ECG:
-
Electrocardiogram
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- SD:
-
Standard deviation
- χ2:
-
Chi-square
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Amin M, Gamal A, Ali M, Awad O. Cardiac troponin T: A sensitive and specific indicator of myocardial injury in patients with cerebrovascular stroke. Egyptian Heart J. 2012;64(3):135–9.
Ashrafi F, Baratloo A, Nasiri Z, Soleymani M, Asaad S. Secondary stroke after thrombolytic administration; a case report. Arch Neurosci. 2014;2(1):e17315. https://doi.org/10.5812/archneurosci.17315.
Faigle R, Marsh EB, Llinas RH, Urrutia VC, Gottesman RF. Troponin elevation predicts critical care needs and in-hospital mortality after thrombolysis in white but not black stroke patients. J Crit Care. 2016;32:3–8.
Faiz KW, Thommessen B, Einvik G, Brekke PH, Omland T, Rønning OM. Determinants of high sensitivity cardiac troponin T elevation in acute ischemic stroke. BMC Neurol. 2014;14:96. https://doi.org/10.1186/1471-2377-14-96.
Etgen T, Baum H, Sander K, Sander D. Cardiac troponins and N-terminal pro-brain natriuretic peptide in acute ischemic stroke do not relate to clinical prognosis. Stroke. 2005;36(2):270–5.
Jauch EC, Saver JL, Adams HP, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke. Stroke. 2013;44:870–947.
Fonarow GC, Saver JL, Smith EE, Broderick JP, Kleindorfer DO, Sacco R, et al. Relationship of National Institutes of Health Stroke Scale to 30-day mortality in medicare beneficiaries with acute ischemic stroke. J Am Heart Assoc. 2012;1(1):42–50.
New PW, Buchbinder R. Critical appraisal and review of the Rankin scale and its derivatives. Neuroepidemiology. 2006;26(1):4–15.
Saposnik G, Di Legge S, Webster F, Hachinski V. Predictors of major neurologic improvement after thrombolysis in acute stroke. Neurology. 2005;65(8):1169–74.
Levesque R. SPSS programming and data management: a guide for SPSS and SAS users. 4th ed. Chicago: SPSS Inc.; 2007.
Jensen JK, Kristensen SR, Bak S, Atar D, Høilund-Carlsen PF, Mickley H. Frequency and significance of troponin T elevation in acute ischemic stroke. Am J Cardiol. 2007;99(1):108–12.
Ay H, Koroshetz WJ, Benner T, Vangel MG, Melinosky C, Arsava EM, et al. Neuroanatomic correlates of stroke-related myocardial injury. Neurology. 2006;66(9):1325–9.
Jespersen CM, Fischer HJ. Myocardial stress in patients with acute cerebrovascular events. Cardiology. 2008;110(2):123–8.
Barber M, Morton JJ, Macfarlane PW, Barlow N, Roditi G, Stott DJ. Elevated troponin levels are associated with sympathoadrenal activation in acute ischaemic stroke. Cerebrovasc Dis. 2007;23(4):260–6.
Christensen H, Johannesen HH, Christensen AF, Bendtzen K, Boysen G. Serum cardiac troponin I in acute stroke is related to serum cortisol and TNF-α. Cerebrovasc Dis. 2004;18(3):194–9.
Bray BD, Campbell J, Hoffman A, Tyrrell PJ, Wolfe CD, Rudd AG. Stroke thrombolysis in England: an age stratified analysis of practice and outcome. Age Ageing. 2013;42(2):240–5.
Nikneshan D, Raptis R, Pongmoragot J, Zhou L, Johnston SC, Saposnik G, et al. Predicting clinical outcomes and response to thrombolysis in acute stroke patients with diabetes. Diabetes Care. 2013;36(7):2041–7.
Yue R, Li D, Yu J, Li S, Ma Y, Huang S, et al. Atrial fibrillation is associated with poor outcomes in thrombolyzed patients with acute ischemic stroke. A Systematic Review and Meta-Analysis. Medicine (Baltimore). 2016;95(10):e3054. https://doi.org/10.1097/MD.0000000000003054.
Mehta A, Mahale R, Buddaraju K, Majeed A, Sharma S, Javali M, et al. Intravenous thrombolysis for acute ischemic stroke: review of 97 patients. J Neurosci Rural Pract. 2017;8(1):38–43.
Liu M, Pan Y, Zhou L, Wang Y. Predictors of post-thrombolysis symptomatic intracranial hemorrhage in Chinese patients with acute ischemic stroke. PLoS One. 2017;12(9):e0184646.
Schechter M, Merz NB, Paul-Labrador MJ, Kaul S. Blood glucose and platelet-dependent thrombosis in patients with coronary artery disease. J Am Coll Cardiol. 2000;35(2):300–7.
Allport LE, Butcher KS, Baird TA, MacGregor L, Desmond PM, Tress BM, et al. Insular cortical ischemia is independently associated with acute stress hyperglycemia. Stroke. 2004;35(8):1886–91.
Acknowledgements
The work was carried out in the Neurology and Clinical Pathology Departments, Faculty of Medicine, Zagazig University, Zagazig, Sharkia, Egypt. The authors acknowledge the subjects for their participation and cooperation in this study.
Funding
There is no source of funding for the research.
Author information
Authors and Affiliations
Contributions
RN, AO, and WM carried out the work. RN designed the study, coordinated the research team, had done the statistical analysis, and reviewed the manuscript. RN and WM collected the patients, gathered clinical data, and reviewed the manuscript. WM wrote the manuscript, coordinated the research team, and reviewed the manuscript. AO helped the laboratory work of the study. All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved from the Institute Research Board of the Faculty of Medicine, Zagazig University, Egypt (ZU-IRB#5335\24-6-2018). A written informed consent was obtained from all the participants or their responsible relatives (if the patient was unable to provide consent due to weakness or disturbed conscious level) after informing them about the study rationale and their right to withdraw from the study at any time without any consequences.
Consent for publication
All participants had signed an informed consent to participate and for the data to be published.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nageeb, R.S., Omran, A.A. & Mohamed, W.S. Troponin-I elevation predicts outcome after thrombolysis in ischemic stroke patients. Egypt J Neurol Psychiatry Neurosurg 57, 4 (2021). https://doi.org/10.1186/s41983-020-00256-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-020-00256-2