Abstract
Introduction
Paget’s disease of bone is usually asymptomatic in most cases. The neurosurgeon should be familiar with the common presentation and complications. The rare presentation of this case of Paget’s disease of the skull raised our attention to report it.
Case description
A Paget’s disease patient presented in the emergency department with a disturbed conscious level (GCS 8) without any history of trauma or seizures. CT showed severe hypertrophied left frontal, temporal, and parietal bones with midline shift. The patient underwent an emergency left decompressive craniectomy. Postoperative CT scan was done and showed frontoparietal epidural hematoma on the opposite side which was evacuated immediately. The patient started to improve and became fully conscious in few days with marked improvement of the motor power of her right side.
Discussion and evaluation
Severe skull involvement and impending brain herniation may occur in Paget’s disease of the skull which needs urgent decompressive surgery. Contralateral epidural hematoma after decompressive surgery may rarely occur and should be suspected in case of intraoperative brain swelling and postoperative failure of improvement. Neurosurgeons and radiologists should recognize the rare phenomenon of periosteal bone formation in the pagetic bone and its extension into surrounding tissues.
Conclusions
In our case, we faced an unusual life-threatening condition in a patient of Paget’s disease with severe skull involvement leading to rapid deterioration of consciousness and impending brain herniation. The neurosurgeon should be aware of this rare emergency condition.
Similar content being viewed by others
Introduction
As a focal skeletal disease, Paget’s disease is present in the pelvis, spine, and skull in most of the cases, and it is asymptomatic. The neurosurgeon should be familiar with the common presentation, complication, surgical, and non-surgical modalities of treatment. The pathology of Paget’s disease is excessive bone formation and malremodeling. The disease is polyostotic in more than half of the cases, and in half of these cases, it affects the vertebral column [1, 2].
Case description
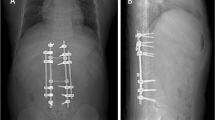
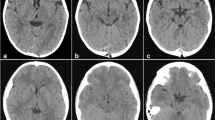
A 30-year-old female, known to have Paget’s disease of bone, presented in the emergency department with a disturbed conscious level (GCS 8) without any history of trauma or seizures. Physical examination found signs of lateralization in the form of unequal pupils and right-sided weakness of gradual onset and progressive course over the past few days in addition to apparent skull deformity. CT scan (using a 16 multi-slice CT scanner, Toshiba Alexion, Japan) was performed which showed severe hypertrophied left frontal, temporal, and parietal bones with midline shift (10 mm) and severe mass effect on the adjacent brain and ventricular system. This patient used to have regular follow-up visits at the rheumatology department in the same institute (Fig. 1).
She had a history of hearing loss, right eye proptosis, and visual loss. The full body scintigraphy (using a nuclear Gamma camera, Philips Forte, USA) revealed increased fixation to the skull bones, right zygoma, bilateral pelvic bones, upper third of left femur, and few osseous lesions at lower cervical spine. The previous biopsy was taken from the osseous lesion of the femur, and the findings were consistent with polyostotic juvenile Paget’s disease of bone (Fig. 2).
The blood chemistries showed an increased level of alkaline phosphatase (2140 IU/ml), serum calcium (10.1), and parathyroid hormone (148 pg/ml). Routine preoperative labs, including bleeding profile, were within normal ranges. The patient underwent an emergency left decompressive craniectomy. The hypertrophied bone was infiltrating into the dura and brain parenchyma. The invaded dura was excised. The hypertrophied bone was carefully elevated off the brain substance, and every attempt was done to create a plane between the bone and the brain surface under the microscope to minimize the brain damage. The use of moist cottonoid, inserted between the bone and the brain, was also useful in spite of pial invasion at many sites. There was increased blood loss during surgery. Duroplasty was done without replacement of the removed bony lesion. Postoperatively, the patient was transported to the ICU without improvement of her clinical condition. CT scan (using a 16 multi-slice CT scanner, Toshiba Alexion, Japan) was done and showed frontoparietal epidural hematoma on the opposite side which was evacuated immediately by right frontoparietal craniotomy. There was blood oozing from the meningeal vessels and the inner table of the pathological bone of the right side leading to the stripping of the dura. This bleeding was controlled by coagulation and bone wax. The space between the dura and the bone was obliterated by dural take-up sutures. The right frontal bony lesion involving the right orbit was not dealt with because it did not cause any brain compression, and the patient had already right visual loss. Our main concern at that time was a prompt evacuation of the life-threatening epidural hematoma which impeded the recovery of the patient (Fig. 3).
The patient started to improve and became fully conscious in few days with marked improvement of the motor power of her right side. The histopathology report of the removed skull lesion was Paget’s disease of bone (Fig. 4).
Discussion and evaluation
Paget’s disease is a chronic disease with hypertrophied and deformed bones mostly at multiple sites. Its pathophysiology is not clear but genetic factors and viral infections may play a role [3, 4]. Paget’s disease is asymptomatic in 70% of patients. There is a predilection for the skull and vertebral column resulting in neurological complications secondary to compressive bony pathology. The neurological complications of cranial disease excluding auditory affection are rare and usually slowly progressive over the years. Basilar invagination may occur due to softening of the base of the skull resulting in the brainstem, cerebellar compression vertebrobasilar insufficiency and obstructive hydrocephalus which usually needs CSF diversion. The severity ranges from asymptomatic to acute tonsillar herniation and death [5]. Osteosarcoma of the skull occurs in less than 1% of patients resulting in the rapid neurological deterioration with poor prognosis despite surgical and radiation therapy. Increased blood flow to the bone results in reported cases of acute compression from epidural hematoma with a poor prognosis due to excessive bleeding during surgery [6]. Thompson and colleagues reported 14 cases of Paget’s osteogenic sarcoma of the skull. Two cases of them had intraparenchymal invasion [7]. The dura mater acts as a potent barrier to the spread of osteogenic sarcoma of the skull. Thus, the intraparenchymal invasion is very rare and considered as a very late stage of the disease [8]. However, infiltration of the surrounding soft tissues appears to be more logic with the sarcomatous transformation of the pagetic bone, such infiltration may occur in the absence of this transformation. Janez Lamovec and colleagues reported a rare case of periosteal bone formation in the pagetic femur with extension in the surrounding soft tissues simulating juxtacortical osteosarcoma but in the absence of any sarcomatous changes. Being a rare event and not recognized enough by radiologists and pathologists, they called it pseudosarcoma of Paget’s disease [9]. We think that was similar to our case. The intracranial dura mater consists of two layers: the inner meningeal layer and the outer endosteal layer that line the inner surface of the cranial bones. We believe that the abnormal dynamic bone remodeling at the periosteal and endosteal envelope of the skull bones in addition to periosteal bone proliferation may explain the invasion of the surrounding soft tissues including the dura and brain without malignant transformation. The occurrence of remote epidural hematoma after decompressive craniectomy is rarely documented in the literature [10]. We think that the cause of this epidural hematoma was the rapid reduction and unequal distribution of ICP after decompressive craniectomy. This created negative pressure after brain shift leading to traction on meningeal vessels. The source of bleeding in our case was the meningeal vessels in addition to bleeding from the inner surface of the pathological bone at that site. Rapidly progressive neurological deterioration should be treated concurrently with medical therapy (calcitonin or iv bisphosphonates) and surgery. The response of cranial complications to medical or surgical treatment is not well documented [6].
Conclusions
In our case, we faced an unusual life-threatening emergency condition in a patient of Paget’s disease with severe skull involvement leading to rapid deterioration of consciousness and impending brain herniation which needed urgent decompressive surgery. The aim of this work is to raise the attention of the neurosurgeons to such rare emergency condition especially in almost asymptomatic disease. Intraoperative brain swelling and failure of improvement after the first surgery raised our suspicious of contralateral hematoma especially in limited resources countries where ICP monitoring is unavailable. Neurosurgeons and radiologists should recognize the rare phenomenon of periosteal bone formation in pagetic bone and its extension into surrounding tissues. To the best of our knowledge, there are no reported cases of such clinical scenario.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- GCS:
-
Glasgow Coma Scale
- ICP:
-
Intracranial pressure
- ICU:
-
Intensive care unit
- iv:
-
Intravenous
References
Mirra JM, Brien EW, Tehranzadeh J. Paget’s disease of bone: review with emphasis on radiologic features, part I. Skelet Radiol. 1995;24(3):163–71.
Mirra JM, Brien EW, Tehranzadeh J. Paget’s disease of bone: review with emphasis on radiologic features, part II. Skelet Radiol. 1995;24(3):173–84.
Mee AP. Paramyxoviruses and Paget’s disease: the affirmative view. Bone. 1999;24(Suppl 5):19S–21S.
Hocking L, Slee F, Haslam SI, Cundy T, Nicholson G, Ralston SH, et al. Familial Paget’s disease of bone: patterns of inheritance and frequency of linkage to chromosome 18q. Bone. 2000;26(6):577–80.
Martin Rubio A, Romero Fernandez AB, Moratinos Yaguez C, Alonso Yague JA, Moron de Miguel C. Paget disease and obstructive hydrocephaly. Rev Esp Anestesiol Reanim. 2006;53(9):590.
Huang TL, Cohen NJ, Sahgal S, Tseng CH. Osteosarcoma complicating Paget’s disease of the spine with neurologic complications. Clin Orthop Relat Res. 1979;(141):260–5.
Thompson JB, Patterson RH Jr, Parsons H. Sarcomas of the calvaria: surgical experience with 14 patients. J Neurosurg. 1970;32:534–8.
Henin D, Weiss AM, Dairou A, Masson M. Osteogenic cranial sarcoma in Paget’s disease. Ann Med Interne (Paris). 1979;130:169–72.
Lamovec J, Rener M, Spiler M. Pseudosarcoma in Paget’s disease of bone. Ann Diagn Pathol. 1999;3(2):99–103.
Su TM, Lee TH, Chen WF, Lee TC, Cheng CH. Contralateral acute epidural hematoma after decompressive surgery of acute subdural hematoma: clinical features and outcome. J Trauma. 2008;65(6):1298–302.
Acknowledgements
Not applicable.
Funding
No fund was needed.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
ME carried out the literature search and review. AE carried out the manuscript preparation. DA performed the manuscript editing. AA collected the clinical and surgical data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We confirm that ethical clearance was not required for publication of this case report. Written informed consent was obtained from the patient.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ashry, A.H., Alnajjar, D.M., Elkatatny, A.A.A.M. et al. Unusual neurosurgical emergency in Paget’s disease of the skull: a case report and review of the literature. Egypt J Neurol Psychiatry Neurosurg 55, 42 (2019). https://doi.org/10.1186/s41983-019-0083-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-019-0083-x