Abstract
Context
Patients with malignant middle cerebral artery (MCA) infarction are prone to a mortality rate of 70–80%. Decompressive craniectomy (DC) has been used as an important treatment modality to control refractory intracranial hypertension.
Aim
In this study, we aimed to evaluate the impact of DC in reducing mortality rate and improving the functional outcome in the patients who underwent DC surgery for malignant MCA infarction
Settings and design
The prospective clinical case study included 24 patients with refractory intracranial hypertension due to malignant MCA infarction
Patients and methods
All patients enrolled in the study have refractory intracranial hypertension due to malignant MCA infarction; they were allocated to undergo decompressive craniectomy between 2014 and 2017. Each patient was evaluated clinically using the Glasgow Coma Scale (GCS) and the modified Rankin Scale (mRS).
Results
All patients on admission have the GCS of 5–12 score (mean 8). Fourteen patients underwent DC in the first 48 h while 10 patients were operated upon after 48 h. Postoperatively, two patients (9%) had a score of 3 on the modified Rankin Scale, six patients (25%) had a score of 4, and eight patients (33%) had a score of 5. Mortality occurred in eight patients (33%) with the worst score of 6. Similar unfavorable outcome was reported at 6- and 12-month follow-up with different degrees of disability.
Conclusion
Decompressive craniectomy for malignant MCA infarction has an effective role in decreasing the mean intracranial pressure, reducing the mortality rate, and increasing the number of patients with a favorable outcome.
Similar content being viewed by others
Introduction
Patients suffering from large hemispheric infarction (LHI), which is also known as malignant middle cerebral artery (MCA) infarction, have an increased incidence of significant disability and mortality [1]. They mainly present with hemiparalysis and severe sensory deficits with aphasia if the dominant hemisphere is affected. In spite of maximum medical therapy such as intracranial pressure (ICP) lowering measures, hypothermia, and controlled hyperventilation, malignant MCA infarction could result in death in 70–80% of cases; most survivors are left with long-term disability [2, 3].
The prognosis is poor; it is attributed to space-occupying edematous infarcted brain tissue, which induces compression of normal brain and blood vessels leading to secondary mechanical and ischemic neuronal injury. Therefore, herniation and death occur [4].
The role of decompressive craniectomy in the management of malignant MCA infarction is debatable by many authors. It was initially developed as a life-saving procedure for patients suffering from malignant hemispheric infarction, but the survivors remained with severe disability which formed a serious concern [5].
The aim of dcompressive craniectomy (DC) is to remove part of the ipsilateral cranium in order to allow the outward herniation of the infarcted brain tissue, thus reducing intracranial pressure and improving cerebral perfusion pressure. Respectively, the blood flow to the ischemic penumbra is maintained [6].
The decision for decompressive surgery in malignant MCA infarction is made on the basis of radiological data and progressing clinical course. The American Heart Association/American Stroke Association (AHA/ASA) updated the guidelines recommending DC in malignant MCA infarction in patients 60 years old or less with unilateral MCA infarctions that are neurologically deteriorating within 48 h despite maximal medical treatments [7].
Several prospective studies reported that DC reduces the case mortality rate of malignant middle cerebral artery infarction by 50–75% in comparison to the best medical treatment alone. Better results achieved with earlier surgery immediately after the start of neurological deterioration related to brain edema or even before [8, 9].
The purpose of the present prospective clinical case study was to review our experience with DC in malignant MCA infarction in regard to the mortality rate and the functional outcome.
Patients and methods
From March 2014 to November 2017, 24 patients were assigned to undergo decompressive craniectomy for refractory intracranial hypertension due to malignant MCA infarction. Ethics approval for this work was obtained in our institution.
The inclusion criteria for surgery included the radiological presence of large MCA infarction involving more than 50% of the MCA territory with signs of local brain swelling in the initial computed tomography (CT) of the brain. Clinically, all patients experienced deterioration of consciousness level. Exclusion criteria included patients with GCS < 4 or bilaterally fixed and dilated pupils. All enrolled patients underwent a complete physical and neurological examination on admission. Initial imaging examinations evaluated the infarct territory, midline shift, and brain edema by CT scan and in some cases by magnetic resonance imaging (MRI) of the brain. Early decompressive craniectomy was performed to 14 patients in the first 48 h while 10 patients were operated upon after 48 h. In patients who presented preoperatively with a deteriorated conscious level, an intraventricular catheter for ICP monitoring was inserted.
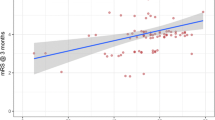
Each patient was evaluated clinically using the Glasgow Coma Scale (GCS). The modified Rankin Scale (mRS) at 3-, 6-, and 12-month post-surgery was used as outcome parameters, and mRS 3 was referred to as moderate disability, mRS 4 defined as a moderate-severe disability, mRS 5 defined as a poor outcome or severe disability, and mRS 6 defined as dead.
Surgical technique
Initially, a large fronto-parieto-temporal skin and muscle flap was performed; a hemicraniectomy of the frontal, parietal, and temporal bones overlying the infarcted hemisphere was removed. The size of the bone flap had a minimum diameter of 12 cm to allow the external herniation of the swollen infarcted brain. Anteriorly, violation of the frontal sinus was avoided. The medial limit of the craniectomy was 2 cm from the midline while it was extended posteriorly approximately 5–6 cm behind the external auditory canal. Basal decompression of the temporal pole was done by removing the temporal squamous bone to the level of the zygomatic arch. A stellate-shaped dural incision was performed; we did not remove the infarcted brain tissue to preserve the salvageable penumbra area or any viable tissue (Figs. 1 and 2). An expansive duraplasty is then performed using a large flap of pericranium to accommodate the brain swelling. Proper hemostasis is done. Finally, the temporalis muscle and skin flap are re-approximated and sutured in layers. Epidural wound drains were routinely used. The bone flap is stored in a tissue bank to be used later after 2–3 months in cranioplasty.
Results
Our study enrolled 24 cases, 9 females (37%) and 15 males (63%); the age varied from 49 to 67 years with mean age 58 years. All patients experienced large hemispheric infarction of the MCA territory. On admission, the Glasgow Coma Scale for all patients varied from 5 to 12 with a mean score of 8 (Table 1). Preoperative clinical symptoms included disturbed consciousness, hemiparalysis, facial nerve palsy, and aphasia. Surgery was performed to 14 patients (59%) in the first 48 h while 10 patients (41%) were operated upon after 48 h.
Overall, eight patients (33%) died in the acute stage. Five deaths were primarily related to a further neurological deterioration. The remaining three deaths were due to secondary complications as infections, in which pneumonia was the leading cause.
Postoperative functional outcomes using the modified Rankin Scale showed moderate disability defined as mRS 3 in two patients (9%), moderately severe disability defined as mRS 4 in six patients (25%), and poor outcome defined as mRS 5 in eight patients (33%) at 3-month follow-up. Similar unfavorable outcome was reported at 6 and 12 months follow-up. Only two patients from the moderately severe disability group were found to have mRS 3 after a 12-month follow-up (Table 2).
Complications reported in our study included postoperative subdural hematomas in two patients, hygroma in four patients, hemorrhagic transformation in two patients, systemic infection as pneumonia in four patients, and wound infection in a single patient. All complications did not require surgical interference and were managed conservatively over time.
Discussion
Malignant middle cerebral artery infarction which usually results from the MCA acute occlusion is considered a serious fatal condition. Life-threatening herniation and brain edema can occur within 1 week after the stroke onset leading to a mortality rate of 80% [10].
Decompressive hemicraniectomy surgery is considered as a life-saving procedure for patients experiencing malignant hemispheric infarction with refractory intracranial hypertension in spite of maximum medical therapy. It is the last resort to prevent fatal cerebral herniation and to achieve better functional outcomes [11].
Despite the effective role of DC in malignant MCA infarction, the severe disability and poor quality of life suffered by many survivors is still a serious concern [12, 13].
The optimal surgical timing should be before or immediately after the neurological deterioration that is related to brain edema. Surgery is then initiated in the first 48 h or even day 7 after stroke onset [14].
It is recommended to perform surgical decompression early before the development of major midline shift and conscious level deterioration. Some researches mentioned that patients for whom early DC was done show better functional outcomes brought about by preventing fatal brain herniation and improving cerebral hemodynamics, thereby limiting secondary injury [15]. In most cases, DC is performed within 48 h after the ischemic stroke. Thus, all patients with acute large hemispheric infarction should be monitored in an intensive care unit (ICU) or stroke unit for the expedition of the timely surgical decompression. ICP monitoring prior to DC in cases with severe neurological deterioration is one of the predicting factors of decompression surgery decision [16].
Repeated publications mentioned that DC in the management of malignant middle cerebral artery infarction revealed low fatality rate and improved functional outcome. Many cohort data reported the case fatality rates during the acute stage as varying between 18 and 35% and moderate disability (mRS 3) at 3 months as varying between 20 and 59% [17].
In our study, the fatality rate was 33%, while in destiny trials, the case fatality rate was 22% but moderate disability (mRS 3) rate was 7% and moderate-severe disability (mRS 4) rate was 32% at the 3-month follow-up [9].
We reported 9% of patients included in our research had mRS 3 and 25% had moderate-severe disability (mRS 4) at the 3-month follow-up, while poor outcome (mRS 5) was 33%.
In Kürten and colleague’s trial [18], 22.8% of patients recovered to moderate disability (mRS 3) at 3-month follow-up, 44.6% remained with moderate-severe disability (mRS 4), and 32.6% suffered a poor outcome (mRS 5).
In our series after the 12-month follow-up, two patients from the severe disability group showed functional improvement. 16.5% of patients recovered to moderate disability (mRS 3) instead of 9% at the 3 -month follow-up and 33% remained mRS 5 with poor outcome. Approximate results were obtained by Zhao and colleagues [19], a cohort who reported moderate disability (mRS 3) in 11.4% and poor outcome (mRS 5) in 24.2% of patients at 12 months. Our study demonstrates that DC improves functional outcomes at 12 months and lowers fatality rates in patients with malignant MCA infarction. Meticulous postoperative management after the decompressive surgery can increase the chance of favorable recovery.
Conclusion
Decompressive craniectomy for malignant MCA infarction has an effective role in decreasing the mean intracranial pressure, reducing the mortality rate, and increasing the number of patients with a favorable outcome.
Abbreviations
- AHA/ASA:
-
American Heart Association/American Stroke Association
- CT:
-
Computed tomography
- DC:
-
Decompressive craniectomy
- GCS:
-
Glasgow Coma Scale
- ICP:
-
Intracranial pressure
- ICU:
-
Intensive care unit
- LHI:
-
Large hemispheric infarction
- MCA:
-
Middle cerebral artery
- MRI:
-
Magnetic resonance imaging
- mRS:
-
Modified Rankin Scale
References
Wijdicks E, Sheth K, Carter B, Greer D, Kasner S, Kimberly W, et al. Recommendations for the management of cerebral and cerebellar infarction with swelling: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(4):1222–38.
Park J, Goh DH, Sung JK, Yang-Ha Hwang YH, Kang DH, Kim Y. Timely assessment of infarct volume and brain atrophy in acute hemispheric infarction for early surgical decompression: strict cutoff criteria with high specificity. Acta Neurochir. 2012;154:79–85.
Rai V, Bhatia R, Prasad K, Srivastava M, Singh S, Rai N, et al. Long-term outcome of decompressive hemicraniectomy in patients with malignant middle cerebral artery infarction: a prospective observational study. Neurol India. 2014;62:26–31.
Soinne L, Sundararajan S, Strbian D. Malignant hemispheric infarction: diagnosis and management by hemicraniectomy. Stroke. 2014;45:185–7.
Hofmeijer J, Algra A, Kappelle LJ, van der Worp HB. Predictors of life-threatening brain edema in middle cerebral artery infarction. Cerebrovasc Dis. 2008;25:176–84.
Slezins J, Keris V, Bricis R, Millers A, Valeinis E, Stukens J, et al. Preliminary results of randomized controlled study on decompressive craniectomy in treatment of malignant middle cerebral artery stroke. Medicina. 2012;48:521–4.
Tanrikulu L, Oez-Tanrikulu A, Weiss C, Scholz T, Schiefer J, Clusmann H, et al. The bigger, the better? About the size of decompressive hemicraniectomies. Clin Neurol Neurosurg. 2015;135:15–21.
Guresir E, Schuss P, Oszvald A, Raabe A, Seifert V, Beck J. Rapid closure technique in decompressive craniectomy. J Neurosurg. 2011;114:954–60.
Yoo BR, Yoo CJ, Kim MJ, Kim WK, Choi DH. Analysis of the outcome and prognostic factors of decompressive craniectomy between young and elderly patients for acute middle cerebral artery infarction. J Cerebrovasc Endovasc Neurosurg. 2016;18(3):175–84.
Huttner HB, Schwab S. Malignant middle cerebral artery infarction: clinical characteristics, treatment strategies, and future perspectives. Lancet Neurol. 2009;8:949–58.
Neugebauer H, Creutzfeldt CJ, Hemphill JC 3rd, Heuschmann PU, Jüttler E. DESTINY-S: attitudes of physicians toward disability and treatment in malignant MCA infarction. Neurocrit Care. 2014;21:27–34.
Mori K, Aoki A, Yamamoto T, Horinaka N, Maeda M. Aggressive decompressive surgery in patients with massive hemispheric embolic cerebral infarction associated with severe brain swelling. Acta Neurochir. 2001;143:483–91.
Zanaty M, Chalouhi N, Starke RM, Clark SW, Bovenzi CD, Saigh M, et al. Complications following cranioplasty: incidence and predictors in 348 cases. J Neurosurg. 2015;123(1):182–8.
Pillai A, Menon SK, Kumar S, Rajeev K, Kumar A, Panikar D. Decompressive hemicraniectomy in malignant middle cerebral artery infarction: an analysis of long-term outcome and factors in patient selection. J Neurosurg. 2007;106:59–65.
Geurts M, van der Worp HB, Kappelle LJ, Amelink GJ, Algra A, Hofmeijer J. Surgical decompression for space-occupying cerebral infarction: outcomes at 3 years in the randomized HAMLET trial. Stroke. 2013;44:2506–8.
Vibbert M, Mayer SA. Early decompressive hemicraniectomy following malignant ischemic stroke: the crucial role of timing. Curr Neurol Neurosci Rep. 2010;10:1–3.
Von Olnhausen O, Thorén M, Von Vogelsang AC, Svensson M, Schechtmann G. Predictive factors for decompressive hemicraniectomy in malignant middle cerebral artery infarction. Acta Neurochir. 2016;58(5):865–72.
Kürten S, Munoz C, Beseoglu K, Fischer I, Perrin J, Steiger H-J. Decompressive hemicraniectomy for malignant middle cerebral artery infarction including patients with additional involvement of the anterior and/or posterior cerebral artery territory—outcome analysis and definition of prognostic factors. Acta Neurochir. 2018;160:83–9.
Zhao J, Su YY, Zhang Y, Zhang YZ, Zhao R, Wang L, et al. Decompressive hemicraniectomy in malignant middle cerebral artery infarct: a randomized controlled trial enrolling patients up to 80 years old. Neurocrit Care. 2012;17:161–71.
Acknowledgements
Not applicable.
Funding
The design of the study and collection, analysis, and interpretation of data and writing the manuscript are funded by the authors.
Availability of data and materials
The data supporting the results reported in the article are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
AE performed the design of this work, writing of the manuscript and participated in clinical examination and surgical intervention of the patients included in this study. Ad E performed the analysis and interpretation of the data, as well as clinical role in the study. All authors read and approved the final manuscript and agreed to take public responsibility for it and have agreed to have their names listed as contributors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was ethically approved by Neurosurgery ethical review committee, Faculty of Medicine, Cairo University on 12th February, 2014. Informed written consent to participate in the study was obtained from participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Elsayed, A., Elsayed, A. Decompressive craniectomy in malignant hemispheric infarction: favorable outcome and disability. Egypt J Neurol Psychiatry Neurosurg 55, 25 (2019). https://doi.org/10.1186/s41983-019-0077-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-019-0077-8