Abstract
Background
Medical malpractice presents a significant challenge to the healthcare system in Egypt and other countries, inflicting both physical and psychological harm on patients. Furthermore, it imposes a financial burden on both patients and physicians. This study aimed to analyze the medicolegal aspects of malpractice claims associated with aesthetic interventions. The study also aims to establish explicit criteria for identifying and differentiating positive cases from negative ones. This study is a retrospective descriptive observational analysis of medical malpractice claims related to aesthetic interventions. The data was obtained from the records of the Cairo Medicolegal Area between 2016 and 2020, encompassing a total of 98 cases in the study.
Results
The majority of cases were females (89.8%). The age group most significantly affected was between 26 to 35 years old. Plastic surgery accounted for the highest percentage (51%) of alleged cases among medical specialties. Consultants were the most frequently accused physicians (32.7%). Liposuction was the most frequent procedure (31.6%). Most of the malpractices occurred in private hospitals (45.9%). The outcome indicated that permanent infirmity accounted for 10.2%, while mortality constituted 3.1%.
Conclusions
The current study demonstrated that women constitute the predominant demographic in the examined malpractice cases, with plastic surgery being the most common area for alleged claims. The main complaints include disfigurement, dissatisfaction with results, and burn injuries. Aesthetic malpractice is more frequent in private hospitals than in general hospitals, frequently necessitating further treatment due to complications.
Similar content being viewed by others
Background
Aesthetic medical interventions refer to procedures conducted on an individual to rectify external deformities in their appearance, texture, and contours of the skin, face, and body (Prendergast 2011).
Medical malpractice denotes actions or omissions by healthcare providers during treatment that diverge from established standards of care, resulting in patient harm (Kadakia et al. 2021).
The incidence of aesthetic procedures performed by aesthetic surgeons has increased in recent years (Moura et al. 2023). Practitioners of aesthetic procedures frequently face malpractice claims, leading to financial burdens, significant time loss, and negative impacts on physicians’ reputations (Hung et al. 2023).
The increasing number of malpractice claims places a significant burden on both physicians and the medical system. This is because it affects the way medical practice is conducted, often leading physicians to practice defensive medicine. Defensive medicine involves the excessive use of resources, such as requesting unnecessary investigations, prescribing medications, or performing procedures, with the primary goal of avoiding malpractice claims rather than prioritizing the best interests of the patient (Dolz-Guerri et al. 2017; Lykkegaard et al. 2018).
Medical malpractice claims may negatively impact future physicians. Research has indicated that medical students opt for low-risk specialties due to concerns about medical malpractice litigations (Thomas et al. 2018; Ekmekci et al. 2021).
According to the 2022 “ISAPS Biennial Global Survey” by the International Society of Aesthetic Plastic Surgeons (ISAPS), Egypt was ranked first among Arab countries and 19th globally in the number of plastic surgeons. The survey indicates that Egypt has 1,450 plastic surgeons, representing 2.7% of the global population of plastic surgeons (ISAPS 2022).
Various judicial systems are present in numerous countries to examine malpractice claims. In Egypt, Law No. 96 of 1952 established the framework for the role of expert witnesses in court proceedings. All malpractice cases are submitted to the local attorney and referred to the Medicolegal Department of the Ministry of Justice for expert evaluation (Sherief et al. 2005).
In Egypt, physicians operate within a legal framework encompassing Penal Law, Civil Law, Code of Criminal Procedures, and Instructions for Public Prosecution. When a case of medical malpractice is raised, a series of legal procedures will take place. First, the patient or a family member shall present a claim to the nearby police department. Secondly, the legal authorities will investigate the case either civil (for compensation, in front of civil court) or criminal (in front of criminal justice). Then, a forensic expert will be assigned to issue a forensic report of living or an autopsy report. Finally, establishing the presence or absence of liability will be concluded (Heikal 2016).
An extensive examination of published literature revealed a dearth of studies on malpractice litigation following aesthetic interventions in Egypt. Therefore, this study aims to examine the medicolegal aspects of medical malpractice claims associated with aesthetic medical interventions in the Cairo Medicolegal Area in Egypt between 2016 and 2020.
Methods
Subjects
This retrospective cohort study analyzed medical malpractice claims associated with aesthetic interventions. Data were sourced from archived reports investigated by the Forensic Medicine Authority in Zeinhom (2016–2018) and the Cairo Medicolegal Area in Ramses Square 2019–2020).
Data collection adhered to strict privacy protocols, including anonymization via case coding, and was conducted with formal authorization from the relevant medicolegal authorities. This guaranteed compliance with ethical standards while allowing the use of de-identified data for research and educational purposes.
Inclusion criteria (Fig. 1)
-
1.
Male and female cases above 18 years old.
-
2.
All cases of medical malpractice claims following aesthetic interventions during the period from January 2016 to December 2020.
Exclusion criteria
-
1.
Aesthetic malpractice cases dismissed without forensic evaluation (e.g., due to plaintiff withdrawal or unavailability).
-
2.
Incomplete cases lacking essential medical documentation.
-
3.
Claims related to reconstructive plastic surgery (i.e., procedures focused on functional restoration rather than aesthetic enhancement).
Case appraisal criteria
-
The personal data of alleged cases (age, sex).
-
Forensic Medicine Authority Opinion: The Forensic Medicine Authority classifies findings as either positive, supporting the plaintiff’s allegations, or negative, favoring the defendant’s physician.
-
Plaintiff’s complaints leading to litigation.
-
Medical practice setting (e.g., private hospital and clinic)
-
Physician Credentials: Specialty and qualification (specialist vs. consultant), with distinctions defined as follows:
-
Specialist: Bachelor’s degree with postgraduate training (diploma/master’s).
-
Consultant: Awarded after ≥ 10 years of post-masters practice or ≥ 3 years post-doctorate.
-
-
The outcome of malpractice claims
-
Judgment Criteria: (whether positive or negative cases) derived from (Azab 2013; El-Kelany and Shahin 2016).
Ethical approval and consent to participate
The study was approved by the Research Ethics Committee at the Faculty of Medicine for Girls Al-Azhar University (the Committee`s reference number is 202108956). Data access permissions were granted by the Egyptian Forensic Medicine Authority and the Ministry of Justice. All data were anonymized prior to analysis to ensure confidentiality.
Statistical analysis
The collected data were analyzed using the statistical software package for social sciences, version 23.0 (SPSS Inc., Chicago, Illinois, USA). Qualitative variables were presented as numbers and percentages. The comparison of categorical data was conducted using both the Chi-square test and Fisher’s exact test. The statistical significance of the results was assessed at a p-value < 0.05.
Results
A total of 1,829 medical malpractice claims were recorded during the study period, of which 104 (5.7%) pertained to aesthetic interventions. After applying inclusion/exclusion criteria, 98 cases were retained for analysis.
Females comprised the majority of plaintiffs (89.8%), with the highest proportion of claims (41.8%) occurring in the 26–35 age group.
Table 1 demonstrates the relation between plaintiffs’ post-aesthetic intervention complaints and forensic medicine opinions. In positive claims (supporting the plaintiff), disfigurement and unsatisfactory results were the most frequent complaints, accounting for 25% (11/44) of cases. Among negative claims (favoring the defendant), disfigurement remained the predominant complaint, representing 38.9% (21/54) of cases.
Table 2 depicts the relation between practice settings and forensic medicine opinions in aesthetic malpractice claims. Private hospitals were the most common among both positive and negative malpractice claims. The positive malpractice claims accounted for 43.2% (19/44) of all malpractice claims, while the negative malpractice claims accounted for 48.1% (26/54).
Table 3 delineates physician specialties implicated in aesthetic malpractice claims. Plastic surgery predominated in positive claims (43.2%, 19/44), followed by dentistry (15.9%, 7/44). Conversely, negative claims most frequently involved dermatology (20.4%, 11/54) and plastic surgery (57.4%, 31/54). Specialty-specific positivity rates were highest in physiotherapy (100%), general surgery (80%), and dentistry (70%) relative to their total caseloads.
Table 4 shows a statistically significant difference between the qualification of the physicians and the opinion of Forensic Medicine, with a p-value (p < 0.05). Specialists had the highest number of positive malpractice claims, 40.9% (18/44). However, consultants had the highest number of negative malpractice claims, 38.9% (21/54). In 34.1% and 40.7% of positive and negative cases, respectively, the qualifications of the defendant physician were not documented.
There was no statistically significant difference in the relation between the type of procedure in aesthetic malpractice claims and the opinion of forensic medicine. Liposuction was the most common procedure among total malpractice claims, followed by a tummy tuck and dental veneers (33/98), (14/98), and (9/98), respectively. Liposuction (15 cases) and dental veneers (6 cases) represented the highest number of positive procedures for malpractice from the total of 44 positive cases. Among positive claims, liposuction (15/44) and dental veneers (6/44) predominated, while liposuction (16/54) and tummy tuck (10/54) were most frequent in negative claims.
Table 5 shows a statistically significant difference between the outcome of aesthetic malpractice claims and the opinion of forensic medicine with a p-value (p < 0.001). Treatment extension resulted in 38.6% (17/44) and 74.1% (40/54) of positive and negative cases, respectively. No permanent infirmity in negative cases, while 10 out of 44 positive cases had permanent infirmity (6 from 10 cases in liposuction operation and 7 from 10 occurred in private hospitals). There was one case of death from the total of 44 positive cases (the cause of death was multiple intestinal perforations during liposuction, which led to peritonitis and septic shock). In addition, out of the total of 54 negative cases, there were two cases of death. Both deaths were caused by pulmonary fat embolism, which resulted in acute cardiopulmonary failure and cardiac arrest. The three fatalities occurred during liposuction procedures.
Figure 2 shows that the most frequent criterion of judgment on negative cases was inevitable complications, accounting for 79.6% (43/54).
Table 6 presents a comparison of the judgment criteria in positive aesthetic malpractice cases alongside their outcomes. The predominant factor was wrong technique, accounting for 68.2% (30/44) of cases, and was involved in 50% (5/10) of permanent infirmity instances. The sole case of mortality resulted from a combination of procedural error and diagnostic oversight.
Discussion
In Egypt, there is an increasing incidence of medical malpractice claims associated with aesthetic interventions. The observed growth can be attributed to continuous medical advancements, increasing public awareness, beauty trends propagated through social media, and various legal and medical factors. The increase was significantly driven by a rise in relevant news articles in the media.
This study aimed to analyze the medicolegal aspects of medical malpractice claims related to aesthetic medical procedures from 2016 to 2020. The data for the study, comprising 98 cases, were obtained from archived records at the Egyptian Forensic Medicine Authority in Cairo.
In our study, females constituted 89.8% of the total cases claiming medical malpractice related to aesthetic interventions. The percentage aligns with findings from a study in Turkey (71.6%) (Öner et al. 2022) and a study in the United States (93.8%) (Reese et al. 2024). Females generally exhibit a greater concern for their appearance than males, associated with body image dissatisfaction and apprehension regarding negative evaluations of their appearance. This finding contradicts the results of other researchers, who indicated that males outnumbered females (Mwaheb 2016).
The age group ranging from 26 to 35 is the most prevalent in the current study, as it is associated with an increased level of anxiety related to aging, body dissatisfaction, and body image. This contradicts the findings of Zhang et al. (2021), who examined malpractice claims among Canadian plastic surgeons and reported that the predominant age group was between 40 and 49.
Forensic medicine determined that 44.9% of cases were positive, while 55.1% were negative. Öner et al. (2022) documented 134 cases of aesthetic malpractice claims in Turkey during the period from 2007 to 2011. Positive malpractice claims were identified in 21.6% of cases, negative malpractice claims in 65.7%, and no opinion was rendered in approximately 12.7% of cases. Moura et al. (2023) indicated that most legal verdicts favored the physician (60.9%), while 34.4% favored the patient. Treglia et al. (2021) found that physicians were deemed accountable in 51% of cases.
Private hospitals accounted for the highest percentage of malpractice claims at 45.9%, followed by medical centers at 30.6% and clinics at 15.3%. The proportion of claims was lowest in general hospitals. This suggests that private hospitals may need further regulations and monitoring.
These results align with studies from the United States and Australia, where private practice was the most common setting for cosmetic malpractice lawsuits (Bismark et al. 2012; Sarmiento et al. 2020). Additionally, an Egyptian study evaluating medical liability claims in Alexandria found that private hospitals had the highest proportion of malpractice claims (53.75%) (Mashali et al., (2020). This finding is consistent with Yücel et al., (2024), who determined that 78% of cases were performed in private hospitals. These results contradict Mwaheb (2016), who observed higher claims in general hospitals (67.3%). However, a Danish study found no association between practice location and litigation frequency among general practitioners (Birkeland and Bogh 2019).
This finding is attributable to Egypt’s status as a developing nation, where the private healthcare sector has grown significantly to address demand and compensate for the expected decrease in public funding. Consequently, the private healthcare sector in Egypt is characterized by inadequate regulation (Mills et al. 2002).
The study revealed that plastic surgeons accounted for the highest percentage of cases (51%), followed by dermatologists (17.3%) and dentists (10.2%). The findings align with a study by Jena et al., (2011), who reported that plastic surgeons and other specialists performing cosmetic procedures face a higher risk of litigation or formal complaints than most specialists. Additionally, Treglia et al. (2021) conducted a retrospective analysis of judgments issued by the Civil Court of Rome (January 2018–February 2019), finding that most claims are filed against dentists and plastic surgeons.
The results are consistent with Öner et al. (2022), who reported plastic surgeons as the most implicated specialty (59%), followed by general practitioners (9%) and dermatologists (7.5%). Similarly, Brozynski et al. (2024) reported that plastic surgeons were defendants in 40 (87%) cases.
Regarding the relation between the number of positive claims in each specialty and the total number of claims in the same specialty, Physiotherapy had the highest percentage of positive cases (100%), followed by general surgery (80%) and dentistry (70%).
Plastic surgery was the most common specialty in negative malpractice claims (57.4%). Plastic surgeons have historically been the pioneers and practitioners of cosmetic surgery. Unfortunately, with the legitimization of aesthetic surgery in the medical community, this lucrative field has attracted surgeons from other specialties—and even non-surgical specialties. In less-regulated settings, cosmetic surgery is performed by non-physicians lacking the necessary qualifications (Rohrich 2001).
Currently, individuals with dental degrees perform cosmetic surgery on the face and body (Rohrich 2001). Regarding physician qualifications, consultants represented the highest proportion of claims (32.7%), whereas residents comprised 3.1%. The findings are consistent with those of Mashali et al. (2020), who indicated that consultants were involved in 34.3% of claims. Consultants are increasingly subject to litigation, likely attributable to patients’ preference for their perceived expertise.
Liposuction was the most frequently reported procedure in malpractice claims, followed by tummy tuck and dental veneers. Consistent with our findings, Reese et al., (2024) documented that the most popular surgeries were abdominoplasty (56.3%) and liposuction (53.1%). In contrast, Facchin et al., (2023) reported that breast augmentation and reduction are the most common lawsuit areas. Moura et al., (2023) reported that the face and neck were the most common procedure (45.3%), followed by breast (15.6%) and fat reduction (15.6%).
Medical malpractice associated with liposuction has garnered significant attention due to severe complications such as pulmonary emboli and fatalities (Mofid et al. 2017). According to Egypt’s 100 Million Health Survey (2019), which screened 49.7 million adults, 39.8% of Egyptians had obesity (BMI ≥ 30 kg/m2) (Aboulghate et al., 2021), likely explaining liposuction’s prevalence in the current study.
Contrary to the findings of Balcik and Cakmak, (2019), which indicated that laser epilation accounts for 30.9% of medical malpractice cases, liposuction represents only 4.9%.
The most common outcome was treatment extension, occurring in 58.2% of cases, followed by complications requiring reoperation at 16.3%. Balcik and Cakmak, (2019) reported that 14.8% of patients required a subsequent operation to address malpractice-related damage.
In this study, permanent infirmities accounted for 22.7% of all positive cases, while no permanent infirmities were observed in negative cases. Permanent infirmity represents a significant legal and medical concern. An irremediable functional restriction, characterized by the loss of an organ’s function, or an irreversible deprivation, marked by the loss of a functioning organ, leads to physical or mental damage that impairs an individual’s ability to perform daily activities (Abd El-Hady et al. 2013).
Moura et al., (2023) identified lasting disability/deformity and poor complication management as primary litigation triggers. Three fatalities occurred during liposuction (two negative, one positive). Forensic experts attributed negative-case deaths to inevitable complications despite physician efforts, while positive-case deaths resulted from wrong diagnosis and wrong technique. These findings align with Balcik and Cakmak, (2019), who reported a 3.7% mortality rate. Conversely, Azab (2013) found death to be the most frequent outcome (42%) in Egyptian Medical Syndicate malpractice claims (2008–2009).
The present study identified wrong technique as the predominant criterion for positive cases, accounting for 68.2%, followed by inadequate postoperative follow-up at 25%. This indicates that physicians must adhere to established protocols and enhance their understanding of medical errors and strategies for prevention. The findings align with an Egyptian study that examined the medico-legal aspects of medical malpractice death cases in Cairo and Giza through 2014. The researchers indicated that the predominant cause of medical errors was negligence (73.68%), followed by complications from surgical therapy (15.79%) (Nagieb et. al, 2023). This finding agrees with El Kelany and Shahin (2016), who examined medical malpractice claims presented to the Medicolegal Consultation Centre (MLCC) in the Faculty of Medicine, Tanta University, Egypt, from 2008 to 2015. The report indicates that instances of positive malpractice were uniformly distributed across four judgment criteria: inadequate follow-up, inadequate measures to prevent complications, improper procedure performance, grave mistake, and wrong diagnosis. Azab (2013) demonstrated that improper procedure performance is the most frequent cause (21%), followed by unethical conduct (19%).
The predominant criterion for negative cases in this study was inevitable complications, accounting for 79.6%. The findings align with the research by El Kelany and Shahin, (2016), which identified inevitable complications as the predominant criterion for negative cases (46.15%). Similarly, Azab, (2013) reported that the most common criterion for negative cases was unsubstantiated error (29.0%), followed by inevitable complications (23.0%). Judgments may incorporate multiple criteria.
The analysis of outcomes in relation to judgment criteria revealed that the most common positive criterion identified was wrong technique, with inadequate follow-up ranking second in cases of permanent infirmity, reoperation, treatment extension, or death. The criteria are essential as they represent the main defenses for accused physicians. A comprehensive evaluation and exclusion of these defenses are crucial prior to the final judgment (El Kelany and Shahin 2016). In contrast, Yücel et al., (2024) identified insufficient or absent informed consent as the most common basis for malpractice claims in Turkey. Future research should aim to address three limitations identified in this study. The first limitation of the study is the limited number of claims studied. This limitation stems from the study's focus on the Cairo Medicolegal Area, which exclusively handles cases from the Cairo, Giza, and Qalyubia governorates. The second limitation pertains to the inclusion of only the final medicolegal reports, as there were no court verdicts to verify the final judgment. Third, the information in each case report is inconsistent; some reports omit factors such as practice setting, physician license, qualifications, and specialty.
Conclusions
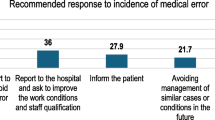
The findings of our study indicate that females aged 26–35 years constitute the majority of the analyzed cases. General surgery represented the highest percentage of reported malpractice claims during the study period. The predominant complaint expressed by most individuals was disfigurement, followed by dissatisfaction with the results and burn injuries. Aesthetic malpractice is more prevalent in private hospitals compared to general hospitals. The predominant outcome of positive claims concerning aesthetic malpractice was the necessity for extended treatment due to complications. Malpractice claims resulting from incorrect techniques were more common than those due to inadequate follow-up. The most common type of malpractice was technical error. We recommend that physicians communicate clearly with patients, detailing the procedure's limitations and potential benefits while eliminating unrealistic expectations to prevent unsatisfactory outcomes. Physicians should adequately follow and monitor their patients after surgery. Moreover, physicians should perform interventions only within their area of specialization, along with professional training, to prevent serious errors, incorrect techniques, and diagnostic errors.
Data availability
Data supporting the findings of the present study will be made available on reasonable request.
Abbreviations
- ISAPS:
-
International Society of Aesthetic Plastic Surgeons
- SPSS:
-
Statistical software package for social sciences
References
Abd El-Hady RH, Thabet RH, Ghandour NM, Mandor AM (2013) Medicolegal aspects of permanent infirmities as a sequel of different types of injuries (a retrospective study in Assiut Governorate, Egypt). Ain Shams J Foren Med Clin Toxicol 20:92–98. https://doi.org/10.21608/AJFM.2013.19389
Aboulghate M, Elaghoury A, Elebrashy I, Elkafrawy N, Elshishiney G, Abul-Magd E, Bassiouny E, Toaima D, Elezbawy B, Fasseeh A, Abaza S, Vokó Z (2021) The Burden of Obesity in Egypt. Front Pub Health 9:718978. https://doi.org/10.3389/fpubh.2021.718978
Azab S (2013) Claims of malpractice investigated by the Committee of medical ethics, Egyptian medical syndicate. Cairo Egypt J Forensic Sci 3(4):104–111. https://doi.org/10.1016/j.ejfs.2013.03.003
Balcik PY, Cakmak C (2019) The evaluation of malpractice cases arising from aesthetic intervention in Turkey based on Supreme Court case law. Int J Health Plann Manage 34(1):e885–e895. https://doi.org/10.1002/hpm.2705
Birkeland S, Bogh SB (2019) General practice location and malpractice litigation. Rural and Remote Health 19:4663. https://doi.org/10.22605/RRH4663
Bismark MM, Gogos AJ, McCombe D, Clark RB, Gruen RL, Studdert DM (2012) Legal disputes over informed consent for cosmetic procedures: a descriptive study of negligence claims and complaints in Australia. J Plast Reconstr Aesthet Surg 65(11):1506–1512. https://doi.org/10.1016/j.bjps.2012.05.004. (PMID: 22652290)
Brozynski M, Via Di, loschpe A, Oleru O, Seyidova N, Rew C, Peter J. Taub PJ, (2024) Never events in plastic surgery: An analysis of surgical burns and medical malpractice litigation. Burns 50(5):1232–1240. https://doi.org/10.1016/j.burns.2024.02.007
Dolz-Guerri F, Gomez-Duran EL, Martinez-Palmer A, Arimany-Manso CCM, J, (2017) Clinical safety and professional liability claims in Ophthalmology. Arch Soc Esp Ophthalmol 92:528–534. https://doi.org/10.1016/j.oftal.2017.05.005
Ekmekci PE, Kurtoglu B, Güner MD (2021) Change in choices regarding the residency of Turkish medical students during medical education. Tıp EgitimiDunyasi 20(60):35–48. https://doi.org/10.25282/ted.757823
El Kelany RS, Shahin MM (2016) Medical Malpractice Claims Investigated by the Medicolegal Consultation Center, Tanta University, Egypt (2008–2015). Mansoura Journal of Forensic Medicine and Clinical Toxicology 24(1):39–55. https://doi.org/10.21608/MJFMCT.2016.48228
Facchin F, Pagani A, Perozzo FAG et al (2023) Litigation Cases after Post-Bariatric Surgery: Lesson from the past Aesth Plast Surg 47:2479–2485. https://doi.org/10.1007/s00266-023-03287-1
Heikal S (2016) Globalization initiatives and Arab penal codes. J Stud Soc Sci 15(2):98–112
Hung YT, Lin JM, Chen YW, Huang YL (2023) Retrospective analysis of aesthetic medical malpractice in mediation proceeding A single-court experience. J Cosmet Dermatol. https://doi.org/10.1111/jocd.15892
ISAPS 2022 https//www.isaps.org/discover/about-isaps/global-statistics/global-survey-2022-full-report-and-press-release/. Accessed 17 July 2024
Jena AB, Seabury S, Lakdawalla D, Chandra A (2011) Malpractice risk according to physician specialty. N Engl J Med 365:629e36. https://doi.org/10.1056/NEJMsa1012370
Kadakia RJ, Orland KJ, Sharma A, Akoh CC, Chen J and Parekh SG. Medical Malpractice Trends in Foot and Ankle Surgery. J Foot Ankle Surg, 2021:22:S1067–2516(21)00227- 1. https://doi.org/10.1053/j.jfas.2021.02.016
Lykkegaard J, Andersen MK, Nexøe J, Hvidt EA (2018) Defensive medicine in primary health care. Scand J Prim Health Care 36:225–226. https://doi.org/10.1080/02813432.2018.1499483
Mashali AA, Omar TEI, Salama NH, Badr El Dine FMM, Mohamed OI (2020) A descriptive study of alleged medical malpractice claims in Alexandria, Egypt How far is it helpful? Annals of Clinical and Analytical Medicine 11(Suppl 3):S248-254. https://doi.org/10.4328/ACAM.20186
Mills A, Brugha R, Hanson K and McPake B (2002) What can be done about the private health sector in low-income countries? Bull World Health Organ 80(4): 325–30. PMID: 12075370; PMCID: PMC2567770.
Mofid MM, Teitelbaum S, Suissa D, Ramirez-Montañana A, Astarita DC, Mendieta C, Singer R (2017) Report on mortality from gluteal fat grafting: recommendations from the ASERF task force. Aesthet Surg J 37(7):796–806
Moura SP, Shaffrey EC, Lam CS, Wirth PJ, Attaluri PK, Rao VK (2023) Out-of-scope Cosmetic Surgery A Review of Malpractice Lawsuits against Nonplastic Surgeons. Plastic & Reconstructive Surgery-Global Open 11(3):e4873. https://doi.org/10.1097/GOX0000000000004873
Mwaheb MA (2016) Screening of Alleged Medical Malpractice in Egypt (Fayoum Governorate). J Forensic Res 7:341. https://doi.org/10.4172/2157-71451000341
Nagieb MM, El-Gallad GA, Ghaleb SS and Saleh AR (2023) Medico legal aspects of medical malpractice dead cases in Cairo and Giza governorates from 2014–2015. Egyptian Journal of Forensic Sciences 13:30. https://doi.org/10.1186/s41935-023-00350-5.
Öner BS, Gündoğmuş ÜN, Çetin S, Şirin G, İritaş SB, Dinç AH, Turan Ö (2022) Evaluation of alleged malpractice due to aesthetic and cosmetic interventions and medical applications. Sabuncuoglu Serefeddin Health Science 4(1):14–27. https://doi.org/10.55895/sshs.1095092
Prendergast PM (2011) Defining Aesthetic Medicine. In: Prendergast PM, Shiffman MA Aesthetic Medicine Art and Techniques. Springer-Verlag Berlin Heidelberg
Rohrich RJ (2001) The market of plastic surgery cosmetic surgery for sale—at what price? Plast Reconstr Surg 107(7):1845–1847. https://doi.org/10.1097/00006534-200106000-00033
Reese A, Navarro A, Kozlowski K, Singh S, Vu G, Neimanis S, Burke M, Morrison C (2024) An Updated Analysis of Body Contouring Malpractice Cases. Ann Plast Surg 1;92(4S Suppl 2):S275-S278. https://doi.org/10.1097/SAP.0000000000003870. PMID: 38556689.
Sarmiento S, Wen C, Cheah MA, et al (2020) malpractice litigation in plastic surgery: can we identify patterns? Aesthet Surg J; 40:NP394–NP401. https://doi.org/10.1093/asj/sjz258
Sherief HM, El Segeeny AL, El Masry MK and Abdel Kareem MA (2005): Retrospective study of medical malpractice cases in Greater Cairo. Msc Thesis, Faculty on Medicine, Ain Shams University, Egypt, pp. 3–152.
Thomas R, Gupta R, Griessenauer CJ, Moore JM, Adeeb N, Motiei-Langroudi R, Guidal B, Agarwal N, Alterman RL, Friedlander RM, Ogilvy CS, Thomas AJ (2018) Medical malpractice in neurosurgery a comprehensive analysis. World Neurosurg 110:e552ee559. https://doi.org/10.1016/j.wneu.2017.11.051
Treglia M, Pallocci M, Passalacqua P, Giammatteo J, De Luca L, Mauriello S, Cisterna AM, Marsella LT (2021) Medical Liability: Review of a Whole Year of Judgments of the Civil Court of Rome. Int J Environ Res Public Health 18(11):6019. https://doi.org/10.3390/ijerph18116019
Yücel AF, Cenger CD, Arıncı RA, Tüzün B (2024) Evaluation of medical malpractice claim reports regarding aesthetic medical intervention cases. Turk J Plast Surg 32:49–53. https://doi.org/10.4103/tjps.tjps_59_23
Zhang Z, Calder L, Finestone PJ, Liu R, Bucevska M, Arneja Jugpal S (2021) Medicolegal Closed Case Trends in Canadian Plastic Surgery A Retrospective Descriptive Study. Plastic and Reconstructive Surgery - Global Open 9(8):e3754. https://doi.org/10.1097/GOX0000000000003754
Acknowledgements
Dr. Ayman Ahmed Hassan, The Head of Forensic Sector and Chief of Forensic Physicians, The Department of Forensic Medicine – Ministry of Justice and Dr. Mohammed Farouq, The Head of Cairo Medico-Legal Area, for their help and cooperation to complete this work.
Funding
None.
Author information
Authors and Affiliations
Contributions
GAR was major contributor in data collection, coding, analysis, and manuscript writing. NAI shared in data collection, coding, analysis, and manuscript writing. IMF shared in data analysis, manuscript writing and submission. SYM was major contributor in data analysis and manuscript writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Research was performed with the approval of Research Ethics Committee at faculty of Medicine for Girls Al-Azhar University (Committee`s reference number is 202108956). Data access permission has been issued from the Egyptian Forensic Medicine authority and the Egyptian Ministry of Justice. Data collection was anonymous.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rawash, G.A., Ibrahim, N.A., Farrag, I.M. et al. Medicolegal aspects of medical malpractice claims following aesthetic interventions in Cairo, Egypt. Egypt J Forensic Sci 15, 2 (2025). https://doi.org/10.1186/s41935-024-00419-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1186/s41935-024-00419-9