Abstract
Background
To investigate whether baseline serum cartilage oligomeric matrix protein (COMP), patient characteristics, traditional cardiovascular disease (CVD) risk factors and disease activity over time predict CVD, in early rheumatoid arthritis (RA).
Methods
This study included patients with early RA (< 12 months disease duration) (n = 233) recruited 1995–2005. Potential predictors of CVD and coronary artery disease (CAD) were assessed using Cox regression.
Results
A first ever diagnosis of CVD occurred in 70 patients, and CAD in 52. Age, sex, hypertension and diabetes predicted CVD and CAD. COMP was associated with increased risk of CVD and CAD [crude hazard ratios (HRs) per SD 1.45; 95% CI 1.17–1.80 and 1.51; 95% CI 1.18–1.92, respectively]. When adjusted for age, sex, hypertension, diabetes and ESR, results where similar but did not reach significance [HRs 1.32, 95% CI 0.99–1.74 and 1.35, 95% CI 0.99–1.86]. Baseline disease activity did not independently predict CVD. High DAS28 (> 5.1) at two years was associated with increased risk of subsequent CVD [adjusted HR 2.58; 95% CI 1.10–6.04] and CAD. ESR and CRP at two years as well as cumulative disease activity over 2 years independently predicted CVD and CAD.
Conclusion
COMP may be a novel predictor of CVD and CAD in RA. Active disease two years after RA diagnosis, as well as cumulative disease activity, was associated with increased risk of CVD and CAD, independent of traditional CVD risk factors. Awareness of the particularly increased CVD risk among difficult to treat patients is important in order to further reduce CVD in RA.
Similar content being viewed by others
Background
Patients with rheumatoid arthritis (RA) have been shown to have an increased risk of cardiovascular disease (CVD) compared to the general population, with a relative risk between 1.4 and 2.1 [1,2,3,4]. The risk has been reported to be increased already in early RA [5]. Traditional CVD risk factors are predictive of CVD in RA [6]. However, the increased risk of CVD in RA has been shown to be partly independent of traditional CVD risk factors [7], indicating additional mechanisms contributing to its development.
Levels of RA disease activity and inflammation have been associated with endothelial dysfunction, subclinical- and clinical atherosclerosis [8, 9]. Markers of inflammation have been shown to be associated with CVD in patients with RA [10,11,12,13,14]. The ability of disease activity score in 28 joints (DAS28) to predict CVD is uncertain when analysed as single measures [15,16,17], whereas multiple measures over time, indicating cumulative disease activity, may be more useful [10, 13, 16, 18, 19]. Results on the impact of the RA-associated autoantibodies rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPA) on CVD risk are mixed [10, 13, 17, 20, 21].
Cartilage oligomeric matrix protein (COMP, thrombospondin 5), a marker of cartilage turnover, is normally found in synovial joints [22] but also in arterial walls [23], with greater abundance in atherosclerotic plaques, particularly those demonstrating vulnerable characteristics [24]. In RA, while associations between serum-COMP and progression of joint damage have been demonstrated [25,26,27,28], its association with CVD has not been studied.
In the recently updated EULAR recommendations, it is suggested that general population CVD risk algorithms should be adapted for patients with RA with an 1.5 multiplication factor for all patients [29]. This method estimates risk on a group level and does not take into consideration disease associated factors that influence risk among RA patients. There is a need for improved individual prediction of CVD in RA. Hence, the aim of this study was to evaluate how a potential novel prognostic marker such as COMP, as well as disease activity measures, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), RA associated auto-antibodies, traditional CVD risk factors, and time to disease-modifying anti-rheumatic drugs (DMARD) treatment and inflammation control over time predict future CVD in patients with early RA.
Methods
Patients
An inception cohort of 233 consecutive patients with early RA was investigated, as previously described [30, 31]. Patients were recruited from the rheumatology outpatient clinic of Skåne University Hospital Malmö, the only hospital serving the city, or from the four rheumatologists in private practice in the area, between 1995 and 2005.
The patients were diagnosed with RA by a specialist in rheumatology, fulfilled the 1987 American College of Rheumatology (ACR) classification criteria for RA [32] and had duration of symptoms ≤ 12 months at the time of inclusion. There were no additional exclusion criteria.
Clinical assessment
Patients were followed according to a structured program with evaluations at baseline, 6 months, 1 year and 2 years. The same rheumatologist (see acknowledgements) performed all the clinical examinations. For each follow-up visit, blood samples were analysed, and disease activity parameters recorded. Disability was assessed using the Swedish version of Health Assessment Questionnaire (HAQ) [33]. All patients were managed according to usual care with no pre-specified protocol for anti-rheumatic treatment. The patients were included before the current practice of treat to target [34] was implemented, and before treatment with biologic DMARDs came into widespread use.
Information on height, weight, and smoking history (current/previous/never) was collected at inclusion by a questionnaire filled out by the patients. The time from symptom onset to start of DMARD treatment, and traditional CVD risk factors at the time of inclusion, were assessed by systematic case record reviews.
The presence of hypertension, diabetes or hyperlipidaemia before RA diagnosis was defined as a corresponding diagnosis in the case records. For hyperlipidaemia, only cases with elevated lipid levels in the case record review were classified as having this exposure in the study.
Data on biologic DMARD treatment during the study period was obtained through a regional biologics register [35].
Laboratory investigations
IgM RF was analysed using ELISA, which was calibrated against the World Health Organization (WHO) RF reference preparation. Anti-cyclic citrullinated peptide antibodies (anti-CCP) were analysed using the Quanta Lite CCP IgG ELISA (INOVA Diagnostics, US). ESR and CRP were assessed according to standard methods at Malmö University Hospital. Serum COMP concentrations were determined using a sandwich ELISA (AnaMar, Lund, Sweden). The detection limit of the assay is < 0.1U/L, and its intra-assay and inter-assay coefficient is < 5% [26].
Cardiovascular disease definitions, data sources and outcome variables
Definitions of CVD in this study were based on codes from the 8th, 9th and 10th version of International Classification of Disease (ICD): (Supplementary Table S1). ICD-codes from 1969 to 2019 were retrieved from the Swedish National Hospital Discharge Register and Causes of Death Register. In Sweden, reporting of underlying and contributing causes of death to the Cause of Death Register is mandatory.
In the analyses on potential prognostic markers, the primary outcome was first diagnosis of CVD (coronary artery disease (CAD), cerebrovascular disease or peripheral artery disease) during the follow-up. Secondary outcomes were the first diagnosis of each respective CVD subcategory: CAD, cerebrovascular disease and peripheral artery disease, during the follow-up.
Statistical analysis
The relation between potential predictors and outcomes of CVD, and of each subcategory, were examined in Cox regression models. Patients were censored at death or at the end of follow-up (December 31, 2019).
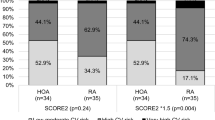
Analyses of COMP, sex, age, time to DMARD, traditional CVD risk factors, serological status, DAS28, HAQ, ESR and CRP as potential baseline predictors of CVD and respective subcategories were performed univariately and adjusted for age, sex, hypertension and diabetes (based on results from the univariate models). To assess whether a potential effect of COMP on the risk of CVD and CAD was influenced by inflammation, we also included ESR in the models. Patients with a registered diagnosis of CVD before inclusion were excluded from analyses of CVD and the respective CVD subcategory.
In separate models, analyses of DAS28, HAQ, ESR and CRP at the 2-years follow-up visit and cumulative measures of DAS28, HAQ and ESR during the first two years after inclusion as potential predictors of subsequent CVD and respective subcategories, were performed univariately and adjusted for age, sex, hypertension and diabetes at baseline (based on results from the univariate models of baseline predictors). For the analyses of the subcategory CAD as outcome, diabetes was not included in the multivariate models due to its lack of independent association with this outcome, and the limited number of patients with CAD in these analyses. Patients with a registered diagnosis of CVD before the 2-year follow-up were excluded from analyses of CVD and the respective CVD subcategory.
All cumulative measures were calculated as area under curve (AUC) from data at inclusion, 6 months, 1 year and 2 years. Risk estimates for continuous disease activity measures (including AUC) were analysed and presented as per standard deviation (SD) to facilitate comparison between potential predictors. Current-, previous-, and ever smoking (current or previous) were each compared to the reference category, never smoking. Body mass index (BMI) was included as a continuous variable.
During part of the study period, high-sensitivity CRP analysis was not available and values between 0 and 9 mg/l were reported as < 9 mg/l. In analyses, CRP was therefore included as a dichotomized variable; that is, above versus below the median (9 mg/l) at inclusion and above versus below the 75th percentile (12 mg/l) at 2 years (since the median at 2 year was < 9 mg/l).
In exploratory analyses, the relation between baseline COMP and CVD risk from inclusion through follow-up was investigated in models stratified by cumulative disease activity over 2 years (above vs. below the median of AUC for DAS28). Patients with a registered diagnosis of CVD before inclusion were excluded from these analyses.
For dichotomous variables, the proportional hazards (PH) assumption was tested by visual examination of plots for log-minus-log function and CVD follow-up time. For continuous variables, the PH assumption was tested by correlation of the partial residuals from cox regression analyses with the rank of CVD follow-up time, and r > 0.3 with p < 0.05 was used as the cut off for exclusion. All models fulfilled the PH assumptions.
Statistical analysis was performed using IBM SPSS Statistics version 28.0, Armonk, NY, IBM Corp.
Results
Patient characteristics and traditional cardiovascular risk factors
A total of 232 patients with RA and available CVD data [median symptom duration 7 months; interquartile range 5–10] were included. Characteristics of patients at baseline are shown in Table 1.
Disease parameters and treatment at baseline and at the 2-year follow-up are shown in Table 2.
A majority of the patients was treated with methotrexate (MTX), and 14% of all patients in the cohort (n = 32) were treated with a biologic DMARD at some time during the first 5 years. At inclusion, 35% were current- and 69% ever smokers. A documented history of hypertension, diabetes and hyperlipidaemia before time of RA diagnosis was found in 28%, 6% and 8% of the patients.
Distribution of CVD after study start
There were 20 patients with a diagnosis of CVD, and 13 with CAD, before inclusion. These were excluded from the analyses of potential baseline predictors of respective outcomes. From inclusion to end of follow-up (2019), CVD occurred in 70 patients and CAD in 52. Since there were only 32 and 19 patients respectively with incident peripheral artery disease and cerebrovascular disease during follow-up, analysis of predictors of these outcomes were not considered feasible. Numbers and distribution of CVD and subcategories are shown in Supplementary table S2.
Impact of variables at inclusion on the risk of CVD and CAD during follow-up
In both crude and adjusted analyses, increasing age and male sex were strongly associated with a higher risk of CVD and CAD (Tables 3 and 4).
In univariate analysis, the presence of hypertension and diabetes were significant predictors of both CVD and CAD while hyperlipidaemia, BMI and smoking were not. When including age, sex, hypertension and diabetes in the multivariate models, hypertension remained significantly associated with CVD [adjusted hazard ratio (HR) 1.91; 95% confidence interval (CI) 1.17–3.11], whereas there were no independent associations with diabetes (Tables 3 and 4).
Baseline ESR and dichotomized CRP levels were significant predictors of CVD in crude models, but not in adjusted models and not for CAD. Positive associations were observed for baseline COMP analysed as a continuous variable with both CVD and CAD, although they did not reach significance in the adjusted models (p = 0.054 and p = 0.067) (Tables 3 and 4). When additionally adjusting for ESR, results were similar (HR 1.32, 95% CI 0.99–1.74 and HR 1.35, 95% CI 0.99–1.86). With COMP categorized according to quartiles with quartiles 1–2 (i.e., below the median) set as reference, significant associations were seen in the unadjusted models, with levels of the 3rd and 4th quartile being associated with an increased risk of CVD, and the 4th quartile of COMP with CAD. Neither of DAS28, HAQ, serological status or time to first DMARD start were associated with CVD or CAD.
Distribution of CVD after the 2-year follow-up
Twenty-three patients with a diagnosis of CVD, and 13 with CAD, before the two-year visit were excluded from the analyses of potential predictors of subsequent outcomes. After the two-year visit, during the follow-up time ranging from 1997 to 2019, CVD occurred in 56 patients and CAD in 45. Since there were only 25 and 17 patients respectively with incident peripheral artery- and cerebrovascular disease, analysis of predictors of these outcomes were not considered feasible. Numbers and distribution with CVD and each subcategory are shown in Supplementary table S2.
Impact of variables up to the 2-year follow-up on the risk of subsequent CVD and CAD
Disease activity parameters at 2 years had a significant impact on the risk of subsequent CVD as well as CAD (Tables 5 and 6).
High disease activity (defined as DAS28 > 5.1) was a strong predictor of subsequent CVD and CAD [HR 2.58; 95% CI 1.10–6.04, adjusted for sex, age, hypertension and diabetes, and HR 3.26; 95% CI 1.37–7.73, adjusted for sex, age, hypertension] respectively, compared to low disease activity (DAS28 ≤ 3.2). Moderate disease activity was not associated with an increased risk of CVD or CAD (Tables 5 and 6).
Both ESR (continuous variable) and CRP levels above 75th percentile (> 12 mg/l) at 2 years showed robust associations with subsequent CAD in crude as well as in models adjusted for age, sex and hypertension [adjusted HR per SD 1.48; 95% CI 1.16–1.88, and adjusted HR 2.33; 95% CI 1.27–4.28 respectively]. ESR predicted CVD, while for CRP a significant association was observed only in the unadjusted analysis (Table 5).
Although baseline disease activity measures showed only limited ability to predict CVD and CAD (Tables 3 and 4), cumulative ESR and DAS28 analysed as AUC from inclusion to the 2-year follow-up were significantly associated with these outcomes in the adjusted models (Tables 5 and 6).
For DAS28 at 2 years, analysed as a continuous variable, non-significant trends towards associations were observed for CVD while the association reached significance in the adjusted model for CAD.
HAQ at 2 years or its cumulative measure up to 2 years showed no significant associations with either of the outcomes.
Relation between COMP and cumulative disease activity, and the risk of CVD during follow-up
In analyses stratified by median AUC for DAS28 over 2 years, baseline COMP was a significant predictor of CVD among those with lower cumulative disease activity [HR per SD 1.70; 95% CI 1.08–2.68], but not among those with cumulative disease activity above the median [HR per SD 1.26; 95% CI 0.90–1.76].
Discussion
Results from this study on a cohort of patients with early RA suggests that COMP may be a novel predictor of CVD. We found persistently active disease to be associated with an increased risk of CVD as well as CAD, independent of traditional CVD risk factors.
To our knowledge, our study is the first to examine the association of COMP with CVD in RA. Our results indicate that higher baseline serum levels of COMP may be prognostic of future CVD and CAD. Interestingly, this is in direct contrast to a large study on the general population by Ueland et al. [36] where higher serum levels of COMP were associated with a lower risk of myocardial infarction (MI). This may reflect a different impact of high levels of COMP derived from increased cartilage turnover in early RA. We have in a previous study shown baseline levels of COMP to be associated with progression of joint erosions over 5 years [27], and this is in accordance with most other studies of early RA [25, 26, 37, 38]. COMP has been identified as a matrix component in atherosclerotic plaques, and it has been suggested that COMP may affect collagen fibre assembly [39] and contribute to a vulnerable plaque phenotype [24]. Interestingly, in non-RA patients with acute coronary syndromes, serum levels of COMP were positively correlated with the risk of subsequent major adverse cardiovascular events [40]. Whether a possible association of serum-COMP with CVD in RA reflects altered vascular morphology or serves as a surrogate marker for disease activity and joint damage, or both, is unknown and requires further investigation. Exploratory analyses in our study indicated that high COMP may be a risk factor for CVD among those with low disease activity. Further studies on COMP and the risk of CVD and potential underlying mechanisms are needed, preferably in larger cohorts.
Higher age, male sex, hypertension, and diabetes were significant predictors of CVD and CAD in this study. Furthermore, we found significant associations for ESR and CRP at baseline with CVD in crude but not in adjusted analyses, while no significant associations were seen for CAD. Baseline DAS28 and HAQ failed to predict CVD or CAD. Similar to our results, previous studies of early RA have shown single baseline levels of DAS28 not to be predictive of future CVD [15,16,17]. By contrast, DAS28 and inflammatory measures up to and including the 2-year follow-up were strongly associated with subsequent CVD and CAD. Similar to our results, others have presented associations of DAS28 over time with CVD [10, 13, 16, 18, 19], although there are some contradictory results [11, 15]. We found ESR at the 2-year follow-up, as well as its cumulative measure up to 2 years, to be significantly predictive of both outcomes, while high CRP at two years was a significant predictor of CAD. Cumulative ESR [11, 13] and CRP have been associated with CVD [11], although there are conflicting results in studies on older cohorts of early RA [15, 18]. In two large scale studies on RA with variable duration, time varying ESR [14] and CRP [41] were associated with MI.
Taken together, results from the present as well as most previous studies indicate that disease activity and inflammatory markers over time are of importance for the development of CVD, while initial disease activity and inflammation at RA onset may not be as predictive.
Since patients respond differently to anti-rheumatic treatment, high disease activity measures at RA onset does not necessarily translate into a major burden of inflammation in subsequent years of disease. It appears more important for the prevention of CVD that a substantial long-term reduction in disease activity and inflammation is achieved.
A number of studies indicate that suppression of disease activity and inflammation by DMARDs used according to modern treatment strategies has decreased the risk of CVD and related mortality in RA [42,43,44,45]. This is compatible with the concept that inflammation partly explains the excess CVD in RA.
Based on results from this study, close monitoring of patients with negative prognostic markers is suggested, and timely pharmacologic as well as non-pharmacologic interventions aimed at reducing the effects of disease activity and cardiovascular risk factors are needed to further improve CVD related outcomes in RA.
One limitation in this study was the relatively small sample size, affecting the statistical power for the multivariate analyses. Also, the patients in our cohort were included just prior to or shortly after the introduction of biologic DMARD use in RA and were classified according to the older 1987 ACR criteria. Hence, the results of this study may not apply to patients diagnosed according to more recent criteria, with more readily accessible biologics and who are treated according to a treat to target strategy [34].
Data on smoking, BMI, and COMP were only collected at baseline, therefore longitudinal assessment of the impact of these factors was not possible. Furthermore, the ICD-codes used for defining CVD in this study may not completely exclude care related to chronic CVD.
Strengths of this study includes the structured longitudinal follow-up of an inception cohort recruited from a defined catchment area. This approach minimizes the impact of selection bias, allowing for greater generalizability of our results to patients with RA seen in real-world clinical practice.
Conclusions
Circulating COMP, which has been used as a marker of cartilage turnover in RA, may be associated with an increased risk of CVD and CAD. High levels of systemic inflammation and DAS28 at two years after diagnosis, as well as cumulative disease activity, were associated with increased risk of CVD and CAD, independent of traditional CVD risk factors. Awareness of the particularly increased CVD risk among difficult to treat patients is important in order to further improve CVD related outcomes in RA.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available due to Swedish legislation (the Personal Data Act), but a limited and fully anonymized dataset containing the individual patient data that support the main analyses is available from the corresponding author on reasonable request.
Abbreviations
- ACPA:
-
anti-citrullinated protein antibodies
- ACR:
-
American College of Rheumatology
- Anti-CCP:
-
anti-cyclic citrullinated peptide antibodies
- AUC:
-
area under curve
- BMI:
-
body mass index
- CAD:
-
coronary artery disease
- CI:
-
confidence interval
- COMP:
-
cartilage oligomeric matrix protein
- CRP:
-
c-reactive protein
- CVD:
-
cardiovascular disease
- DAS28:
-
disease activity score in 28 joints
- DMARD:
-
disease-modifying anti-rheumatic drugs
- ESR:
-
erythrocyte sedimentation rate
- EULAR:
-
European League Against Rheumatism
- HAQ:
-
health assessment questionnaire
- HR:
-
hazard ratio
- ICD:
-
International Classification of Disease
- MI:
-
myocardial infarction
- MTX:
-
methotrexate
- PH:
-
proportional hazards
- RA:
-
rheumatoid arthritis
- RF:
-
rheumatoid factor
- SD:
-
standard deviation
- WHO:
-
World Health Organization
References
Meune C, Touze E, Trinquart L, Allanore Y. High risk of clinical cardiovascular events in rheumatoid arthritis: levels of associations of Myocardial Infarction and Stroke through a systematic review and meta-analysis. Arch Cardiovasc Dis. 2010;103(4):253–61.
Holmqvist M, Ljung L, Askling J. Acute coronary syndrome in new-onset rheumatoid arthritis: a population-based nationwide cohort study of time trends in risks and excess risks. Ann Rheum Dis. 2017;76(10):1642–7.
Jang SY, Kang KW, Jo M, Park M. Risk of New-Onset Acute Coronary Syndrome and Atrial Fibrillation in patients with rheumatoid arthritis compared with a risk-set and propensity score-matched Cohort- A Nationwide Cohort Study. Circ J. 2021;85(2):194–200.
Wiseman SJ, Ralston SH, Wardlaw JM. Cerebrovascular Disease in Rheumatic Diseases: a systematic review and Meta-analysis. Stroke. 2016;47(4):943–50.
Kerola AM, Kauppi MJ, Kerola T, Nieminen TV. How early in the course of rheumatoid arthritis does the excess cardiovascular risk appear? Ann Rheum Dis. 2012;71(10):1606–15.
Baghdadi LR, Woodman RJ, Shanahan EM, Mangoni AA. The impact of traditional cardiovascular risk factors on cardiovascular outcomes in patients with rheumatoid arthritis: a systematic review and meta-analysis. PLoS ONE. 2015;10(2):e0117952.
del Rincon ID, Williams K, Stern MP, Freeman GL, Escalante A. High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors. Arthritis Rheum. 2001;44(12):2737–45.
de Groot L, Jager NA, Westra J, Smit AJ, Kallenberg CG, Posthumus MD, Bijl M. Does reduction of disease activity improve early markers of cardiovascular disease in newly diagnosed rheumatoid arthritis patients? Rheumatology 2015.
Ambrosino P, Lupoli R, Di Minno A, Tasso M, Peluso R, Di Minno MN. Subclinical Atherosclerosis in patients with rheumatoid arthritis. A meta-analysis of literature studies. Thromb Haemost. 2015;113(5):916–30.
Innala L, Moller B, Ljung L, Magnusson S, Smedby T, Sodergren A, Ohman ML, Rantapaa-Dahlqvist S, Wallberg-Jonsson S. Cardiovascular events in early RA are a result of inflammatory burden and traditional risk factors: a five year prospective study. Arthritis Res Therapy. 2011;13(4):R131.
Ajeganova S, Andersson ML, Frostegard J, Hafstrom I. Disease factors in early rheumatoid arthritis are associated with differential risks for cardiovascular events and mortality depending on age at onset: a 10-year observational cohort study. J Rhuematol. 2013;40(12):1958–66.
Zhang J, Chen L, Delzell E, Muntner P, Hillegass WB, Safford MM, Millan IY, Crowson CS, Curtis JR. The association between inflammatory markers, serum lipids and the risk of cardiovascular events in patients with rheumatoid arthritis. Ann Rheum Dis. 2014;73(7):1301–8.
Mantel A, Holmqvist M, Nyberg F, Tornling G, Frisell T, Alfredsson L, Askling J. Risk factors for the rapid increase in risk of acute coronary events in patients with new-onset rheumatoid arthritis: a nested case-control study. Arthritis Rheumatol. 2015;67(11):2845–54.
Navarro-Millan I, Yang S, DuVall SL, Chen L, Baddley J, Cannon GW, Delzell ES, Zhang J, Safford MM, Patkar NM et al. Association of hyperlipidaemia, inflammation and serological status and coronary heart disease among patients with rheumatoid arthritis: data from the National Veterans Health Administration. Annals of the rheumatic diseases 2015.
Radovits BJ, Popa-Diaconu DA, Popa C, Eijsbouts A, Laan RF, van Riel PL, Fransen J. Disease activity as a risk factor for Myocardial Infarction in rheumatoid arthritis. Ann Rheum Dis. 2009;68(8):1271–6.
Arts EE, Fransen J, Den Broeder AA, van Riel P, Popa CD. Low Disease activity (DAS28 ≤ 3.2) reduces the risk of first cardiovascular event in rheumatoid arthritis: a time-dependent Cox regression analysis in a large cohort study. Ann Rheum Dis. 2017;76(10):1693–9.
Westerlind H, Ronnelid J, Hansson M, Alfredsson L, Mathsson-Alm L, Serre G, Cornillet M, Holmdahl R, Jakobsson PJ, Skriner K et al. Anti-citrullinated protein antibody specificities, rheumatoid factor isotypes, and Incident Cardiovascular events in patients with rheumatoid arthritis. Arthritis Rheumatol 2020.
Arts EE, Fransen J, den Broeder AA, Popa CD, van Riel PL. The effect of Disease duration and Disease activity on the risk of Cardiovascular Disease in rheumatoid arthritis patients. Ann Rheum Dis. 2015;74(6):998–1003.
Ajeganova S, de Faire U, Jogestrand T, Frostegard J, Hafstrom I. Carotid Atherosclerosis, Disease measures, oxidized low-density lipoproteins, and atheroprotective natural antibodies for Cardiovascular Disease in early rheumatoid arthritis -- an inception cohort study. J Rhuematol. 2012;39(6):1146–54.
Lopez-Longo FJ, Oliver-Minarro D, de la Torre I, Gonzalez-Diaz de Rabago E, Sanchez-Ramon S, Rodriguez-Mahou M, Paravisini A, Monteagudo I, Gonzalez CM, Garcia-Castro M, et al. Association between anti-cyclic citrullinated peptide antibodies and Ischemic Heart Disease in patients with rheumatoid arthritis. Arthritis Rheum. 2009;61(4):419–24.
Mackey RH, Kuller LH, Deane KD, Walitt BT, Chang YF, Holers VM, Robinson WH, Tracy RP, Hlatky MA, Eaton CB, et al. Rheumatoid Arthritis, anti-cyclic citrullinated peptide positivity, and Cardiovascular Disease Risk in the women’s Health Initiative. Arthritis Rheumatol. 2015;67(9):2311–22.
Saxne T, Heinegard D. Cartilage oligomeric matrix protein: a novel marker of cartilage turnover detectable in synovial fluid and blood. Br J Rheumatol. 1992;31(9):583–91.
Riessen R, Fenchel M, Chen H, Axel DI, Karsch KR, Lawler J. Cartilage oligomeric matrix protein (thrombospondin-5) is expressed by human vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 2001;21(1):47–54.
Hultman K, Edsfeldt A, Bjorkbacka H, Duner P, Sundius L, Nitulescu M, Persson A, Boyle JJ, Nilsson J, Hultgardh-Nilsson A, et al. Cartilage oligomeric matrix protein associates with a vulnerable plaque phenotype in human atherosclerotic plaques. Stroke. 2019;50(11):3289–92.
Forslind K, Eberhardt K, Jonsson A, Saxne T. Increased serum concentrations of cartilage oligomeric matrix protein. A prognostic marker in early rheumatoid arthritis. Br J Rheumatol. 1992;31(9):593–8.
Andersson ML, Svensson B, Petersson IF, Hafstrom I, Albertsson K, Forslind K, Heinegard D, Saxne T. Early increase in serum-COMP is associated with joint damage progression over the first five years in patients with rheumatoid arthritis. BMC Musculoskelet Disord. 2013;14:229.
Rydell E, Forslind K, Nilsson JA, Karlsson M, Akesson KE, Jacobsson LTH, Turesson C. Predictors of radiographic erosion and joint space narrowing progression in patients with early rheumatoid arthritis: a cohort study. Arthritis Res Therapy. 2021;23(1):27.
Tseng S, Reddi AH, Di Cesare PE. Cartilage oligomeric matrix protein (COMP): a biomarker of arthritis. Biomark Insights. 2009;4:33–44.
Agca R, Heslinga SC, Rollefstad S, Heslinga M, McInnes IB, Peters MJ, Kvien TK, Dougados M, Radner H, Atzeni F, et al. EULAR recommendations for Cardiovascular Disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis. 2017;76(1):17–28.
Rydholm M, Book C, Wikstrom I, Jacobsson L, Turesson C. Course of grip force impairment in patients with early rheumatoid arthritis over the first five years after diagnosis. Arthritis Care Res. 2018;70(4):491–8.
Rydell E, Forslind K, Nilsson JA, Jacobsson LTH, Turesson C. Smoking, body mass index, Disease activity, and the risk of rapid radiographic progression in patients with early rheumatoid arthritis. Arthritis Res Therapy. 2018;20(1):82.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–24.
Ekdahl C, Eberhardt K, Andersson SI, Svensson B. Assessing disability in patients with rheumatoid arthritis. Use of a Swedish version of the Stanford Health Assessment Questionnaire. Scand J Rheumatol. 1988;17(4):263–71.
Smolen JS, Aletaha D, Bijlsma JW, Breedveld FC, Boumpas D, Burmester G, Combe B, Cutolo M, de Wit M, Dougados M, et al. Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis. 2010;69(4):631–7.
Geborek P, Nitelius E, Noltorp S, Petri H, Jacobsson L, Larsson L, Saxne T, Leden I. Population based studies of biological antirheumatic drug use in southern Sweden: comparison with pharmaceutical sales. Ann Rheum Dis. 2005;64(12):1805–7.
Ueland T, Laugsand LE, Vatten LJ, Janszky I, Platou C, Michelsen AE, Damas JK, Aukrust P, Asvold BO. Extracellular matrix markers and risk of Myocardial Infarction: the HUNT study in Norway. Eur J Prev Cardiol. 2017;24(11):1161–7.
Fujikawa K, Kawakami A, Tamai M, Uetani M, Takao S, Arima K, Iwamoto N, Aramaki T, Kawashiri S, Ichinose K, et al. High serum cartilage oligomeric matrix protein determines the subset of patients with early-stage rheumatoid arthritis with high serum C-reactive protein, matrix metalloproteinase-3, and MRI-proven bone erosion. J Rhuematol. 2009;36(6):1126–9.
Fex E, Eberhardt K, Saxne T. Tissue-derived macromolecules and markers of inflammation in serum in early rheumatoid arthritis: relationship to development of joint destruction in hands and feet. Br J Rheumatol. 1997;36(11):1161–5.
Bond AR, Hultgardh-Nilsson A, Knutsson A, Jackson CL, Rauch U. Cartilage oligomeric matrix protein (COMP) in murine brachiocephalic and carotid atherosclerotic lesions. Atherosclerosis. 2014;236(2):366–72.
Chen H, Wang J, Xie L, Shen YL, Wang HM, Zheng KL, Zhang Q. Correlation between serum cartilage oligomeric matrix protein and major adverse cardiovascular events within 30 days in patients with acute coronary syndrome. Ann Transl Med. 2021;9(4):353.
Zhang J, Chen L, Delzell E, Muntner P, Hillegass WB, Safford MM, Millan IY, Crowson CS, Curtis JR. Republished: the association between inflammatory markers, serum lipids and the risk of cardiovascular events in patients with rheumatoid arthritis. Postgrad Med J. 2014;90(1070):722–9.
Jacobsson LT, Turesson C, Nilsson JA, Petersson IF, Lindqvist E, Saxne T, Geborek P. Treatment with TNF blockers and mortality risk in patients with rheumatoid arthritis. Ann Rheum Dis. 2007;66(5):670–5.
Ozen G, Pedro S, Michaud K. The risk of Cardiovascular events Associated with Disease-modifying Antirheumatic Drugs in rheumatoid arthritis. J Rhuematol. 2021;48(5):648–55.
Karpouzas GA, Ormseth SR, Hernandez E, Budoff MJ. Biologics May prevent Cardiovascular events in rheumatoid arthritis by inhibiting coronary plaque formation and stabilizing high-risk lesions. Arthritis Rheumatol. 2020;72(9):1467–75.
Roubille C, Richer V, Starnino T, McCourt C, McFarlane A, Fleming P, Siu S, Kraft J, Lynde C, Pope J, et al. The effects of tumour necrosis factor inhibitors, methotrexate, non-steroidal anti-inflammatory Drugs and corticosteroids on cardiovascular events in rheumatoid arthritis, psoriasis and psoriatic arthritis: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74(3):480–9.
Acknowledgements
Christina Book, MD, PhD, initiated this project and performed a major part of the data collection. She passed away before preparation of this manuscript.
Funding
Open access funding provided by Lund University. This work was supported by The Swedish Research Council [grant number 2015–02228], The Swedish Rheumatism Association [grant number R-664091] and Lund University [grant number ALFSKANE-446501] and Region Skåne [grant number 2021 − 0861]. The funding bodies played no role in the design of the study and collection, analysis, interpretation of data, and in writing the manuscript.
Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
ER participated in the study design, performed the statistical analysis, participated in the interpretation of the results, and drafted the manuscript. LTHJ participated in the initiation of this project, the study design and in the interpretation of the results. TS participated in the interpretation of the results and contributed with expertise and literature regarding COMP. CT participated in the study design and the interpretation of the results and helped draft the manuscript. All authors participated in the critical revision of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Regional Ethical Review Board for southern Sweden (Lund, Sweden: LU 410 − 94 and 2021–03421), and complied with the Declaration of Helsinki. All patients gave their written informed consent for participation in the study, including data collection and inclusion in the database.
Consent for publication
Consent obtained directly from patients.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rydell, E., Jacobsson, L.T., Saxne, T. et al. Cardiovascular disease risk in early rheumatoid arthritis: the impact of cartilage oligomeric matrix protein (COMP) and disease activity. BMC Rheumatol 7, 43 (2023). https://doi.org/10.1186/s41927-023-00367-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41927-023-00367-2